Transcription
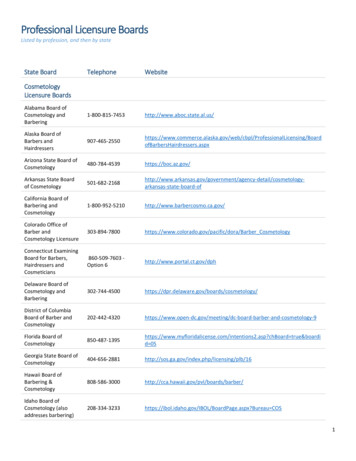
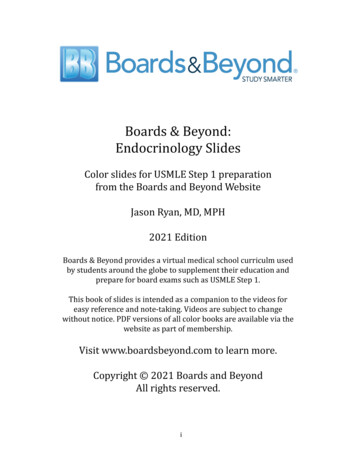
Boards & Beyond:Endocrinology SlidesColor slides for USMLE Step 1 preparationfrom the Boards and Beyond WebsiteJason Ryan, MD, MPH2021 EditionBoards & Beyond provides a virtual medical school curriculm usedby students around the globe to supplement their education andprepare for board exams such as USMLE Step 1.This book of slides is intended as a companion to the videos foreasy reference and note-taking. Videos are subject to changewithout notice. PDF versions of all color books are available via thewebsite as part of membership.Visit www.boardsbeyond.com to learn more.Copyright 2021 Boards and BeyondAll rights reserved.i
ii
Table of ContentsThyroid Gland .1Thyroid Disorders .9Thyroid Cancer . 17Adrenal Glands . 20CAH . 25Adrenal Disorders . 30Endocrine Pancreas . 39Diabetes . 46Insulin . 55Treatment of Diabetes . 59Reproductive Hormones . 65Male Reproductive Hormones . 69Female Reproductive Hormones . 77Menstrual Cycle . 81Pituitary Gland . 88Parathyroid Gland . 96MEN Syndromes .104Signaling Pathways .107iii
iv
Thyroid GlandThyroid Anatomy Two lobes (left, right) Isthmus: thin band of tissue between lobes Sometimes pyramidal lobe above isthmusThyroid GlandJason Ryan, MD, MPHThyroid AnatomyThyroid Embryology Blood supply: superior and inferior thyroid arteries Superior thyroid: 1st branch external carotid artery Inferior thyroid: Thyrocervical trunk (off subclavian) Forms from floor of pharynx (epithelial cells)24-28 Day Old EmbryoWikipedia/Public DomainThyroid EmbryologyForamen Cecum Descends into neck Initially maintains connection to tongueForamen Cecum(end of median sulcus) Thyroglossal duct Disappears later in development Two remnants of duct in child/adult Foramen cecum in tongue Pyramidal lobe of thyroid1
Thyroglossal Duct CystEctopic Thyroid Functioning thyroid tissue outside of gland Most common location is base of tongue Presents as a mass in the tonguePersistent remnant of thyroglossal ductMidline neck mass; usually painlessUsually discovered in childhoodClassically, move up with swallowing or tongueprotrusion May contain thyroid cells Commonly detected during increased demand for hormones Puberty and pregnancy May be the only functioning thyroid tissue May under-produce thyroid hormone hypothyroidism TSH growth of ectopic tissueKlaus D. Peter, Gummersbach, GermanyThyroid HistologyThyroid Hormones Contain the element iodine Iodized salt Thyroid gland contains “follicles” Filled with colloid (protein material) Single layer of epithelial cells lines each follicle Table salt (NaCl) mixed with small minute amount of iodine Done in many countries to prevent iodine deficiency Added to salt in US in 1924 “Follicular cells” Hormone synthesized by follicular cellsUwe Gille/WikipediaThyroid HormonesThyroglobulin Two hormones: T3 and T4 Synthesized from tyrosine and iodine Large protein Produced by thyroid follicular cells Contains numerous tyrosine moleculesTyrosineTriiodothyronine hyroxine (T4)2Tyrosine
Iodine Iodine I (chemical element, atomic number 53) Iodide iodine bound to another atomFollicular Cell “Iodide salt” with negative charge (I-) Potassium iodide KI Plasma iodine exists as iodide salt For thyroid hormone, iodide in our diet needs to be: Taken up by follicular cells Oxidized to I2 (undergo “oxidation”) Added to organic/carbon structures (“organification”)IodideNISNaNISNa-Iodine SymporterPerchlorate (ClO4-)Pertechnetate (TcO4-)XTyPlasmaTyTyTyTGFollicle LumenFollicular CellIodideTyrosineThyroid Peroxidase(TPO) I2PlasmaTyTyTyTyThyroid Peroxidase(TPO)Iodine llicle LumenHormone SynthesisCoupling ReactionsThyroid (MIT)Triiodothyronine (T3)Thyroid Peroxidase(TPO)Thyroxine (T4)Diiodotyrosine(DIT)Diiodotyrosine(DIT)3Ty
TPOHormone SynthesisThyroid PeroxidasePlasma Multifunctional enzyme Catalyzes:T3 Oxidation of iodide Organification of iodine into MIT/DIT Coupling of MIT/DIT into T3/T4T4Follicular CellT4IodideThyroid HormonesT3Follicle LumenT4T3Thyroid Peroxidase(TPO)T4TGTPOI2T4TPOTyMIT DITTyTyTyMIT DITTGTyTGHyperthyroid Medications Propylthiouracil (PTU) T4 is major hormone produced by thyroid gland 90% of thyroid hormone produced is T4 Inhibits TPO: T3/T4 from thyroid gland Inhibits 5’-deiodinase: T4 to T3 conversion peripherallyT3 more potent hormoneT4 is a “prohormone” for T35’ deiodinase converts T4 T3Most conversion occurs in peripheral tissues Methimazole Inhibits TPO Propranolol IodineThyroxine (T4)T4Proteolysis TPO antibodies common in autoimmune thyroiddisease T35’-deiodinasePTU and Methimazole are both“thioamides”Beta blockerWeak inhibitor of 5’-deiodinaseExcellent drug in thyrotoxicosisBlocks catecholamines and T4-T3 conversionTriiodothyronine (T3)Wolff-Chaikoff EffectAmiodarone Excessive iodide in diet could lead to hyperthyroidism Thyroid protects itself via Wolff-Chaikoff Effect Organification inhibited by iodide Less synthesis of MIT/DITClass III antiarrhythmic drugCommonly used in atrial fibrillationContains iodineCan cause hypothyroidism via excess iodine Wolff-Chaikoff Effect4
AmiodaroneRadioactive Iodine Mimics T4 I131 is an isotope of iodine Inhibits 5’-deiodinase T3 TSH from pituitary gland TSH rises after start of therapy then normalizes Has 53 protons like elemental iodine Extra neutrons Emits radiation (β-decay) Exposure radioactive iodine in thyroid gland Competes with elemental iodine for uptake Will concentrate in thyroid gland Small dose: Used for imaging Large dose: Destroys thyroid tissue Used as therapy for hyperthyroidismTBGTBGThyroxine-Binding GlobulinThyroxine-Binding Globulin Estrogen raises TBG levels Most plasma thyroid hormone is T4 Thyroid hormones poorly soluble in water Most T4 is bound to TBG Some with transthyretin and albumin TBG present in small amount but has high affinity TBG produced in liverModifies TBG moleculesSlows clearance from plasmaPregnancy, OCP usersWill raise total T4 levels Liver failure lowers TBG levels Less production of protein Can lower total T4 levels Key point: Less TBG less available T4/T3 to tissuesTBG-T4 T4TBGThyroid Hormone ReceptorThyroxine-Binding Globulin Family of nuclear receptors Hormone-activated transcription factors Modulate gene expressionRise in TBGMore bound T4Less free T4 TSH Total T4 Free T4 (back to normal) TSH (back to normal)5
Thyroid HormoneEffects of Thyroid Hormone Metabolic EffectsMajor regulator of metabolic activity and growthGlucose, lipid metabolismCardiac functionBone growthCNS development Carbohydrate Metabolism glycogenolysis, gluconeogenesis Fat Metabolism Hypothyroid patients: cholesterol Hyperthyroid patients: hyperglycemiaThyroid HormoneThyroid HormoneMetabolic EffectsCardiac Effects basal metabolic rate CO/HR/SV/contractility β1 receptors in heart Hyperthyroid patients: Tachycardia Basal rate of energy use per time Amount of energy burned if you slept all day Na/K ATPase pumps lipolysis concentrations of cholesterol, triglycerides low‐density lipoprotein receptors in liver ( LDL) cholesterol secretion in bileMore pumps more ATP consumed oxygen demand to replenish ATP respiratory rate body temperature Hyperthyroid patients: weight lossMcDonough AA, et al. Thyroid hormone coordinately regulates Na -K -ATPase alpha- and beta-subunitmRNA levels in kidney. Am J Physiol. 1988 Feb;254(2 Pt 1):C323-9.Thyroid HormoneThyroid HormoneCNS and Bone effectsCNS and Bone effects Most common treatable cause intellectual disability Most babies appear normal TH required for normal bone growth/CNS maturation Childhood hypothyroidism cretinism Stunted growth Intellectual disability Maternal T3/T4 crosses placenta Newborn screening programs Causes Measure T4 or TSH from heel-stick blood specimensIodine deficiencyThyroid dysgenesisInborn errors of hormone synthesis (dyshormonogenesis)TPO most common6
Thyroid HormoneThyroid Hormone RegulationCNS and Bone effects Intellectual disabilityCoarse facial featuresShort statureUmbilical herniaEnlarged tongueTSH (thyrotropin) released by anterior pituitaryBinds to receptors on follicular cellsActivates cAMP/PKA 2nd messenger system T3/T4 release rate of proteolysis of thyroglobulin Leads to rapid release of more T3/T4 Also stimulates thyroid cell growth, TG synthesisWellcome Images/WikipediaThyroid Hormone RegulationPregnancy Serum T4/T3 level sensed by hypothalamus Releases thyroid releasing hormone (TRH) Multiple effects on thyroid hormone production Rise in total plasma T4/T3 levels Rise in TBG levels (estrogen) hCG stimulates thyroid (same alpha unit as TSH) Raises free T4 lower TSHTBGTotal T4Free T4Mikael Häggström/WikipediaTSHWeeks of PregnancyThyroid PanelCalcitonin Four standard measurements to assess thyroid Hormone produced by thyroid Synthesized by parafollicular cells (C-cells)C cellAndrea Mazza/Wikipedia7
Calcitonin Lowers serum calcium Suppresses resorption of bone; inhibits osteoclasts Inhibits renal reabsorption of calcium, phosphorus Increased calcium in urine Probably minor role in calcium handling in humans Used as pharmacologic therapy for hypercalcemia8
Thyroid DisordersThyroid DisordersThyroid DisordersThyroid DisordersHyperthyroidJason Ryan, MD, MPHHypothyroidism HyperlipidemiaMetabolism SLOWS DOWNLethargy, fatigueWeakness; dyspnea on exertionCold intoleranceWeight gain with loss of appetiteConstipationHyporeflexiaDry, cool skinCoarse, brittle hairBradycardia MyxedemaThyroid dermopathyThyroid dermopathyNon-pitting edema of the skin from hypothyroidismHyaluronic acid deposits in dermisDraws water out swellingUsually facial/periorbital swellingPretibial myxedema Special form of myxedema over shin Seen in Graves' disease (hyperthyroidism) Myxedema coma coma from hypothyroidismHerbert L. Fred, MD and Hendrik A. van Dijk9ThyroiditisClassic feature of hypothyroidism total cholesterol LDL cholesterolPrimary mechanism: LDL receptor density T3 upregulates LDL receptor gene activationMyxedema Hypothyroid
Hypothyroid MyopathyHyponatremia Muscle symptoms common in hypothyroid Weakness, cramps, myalgias serum creatine kinase (CK) common (up to 90%) Hypothyroidism is a well-described cause Na High levels of ADH (SIADH) May lead to confusionWikipedia/Public DomainThyroid ReplacementHyperthyroidism Levothyroxine (Synthroid): synthetic T4 Liothyronine (Cytomel): synthetic T3 Levothyroxine preferred T3 absorbed from intestines rapidlyCan cause mild hyperthyroidism symptomsTachycardia, tremorAlso, T4 converted to T3 Titrate dose until TSH is normalThyroid StormGoiter Life-threatening hyperthyroidism (thyrotoxicosis) Usually precipitated by acute event Metabolism SPEEDS UPHyperactivityHeat intoleranceWeight loss with increased appetiteDiarrheaHyperreflexiaWarm, moist skinFine hairTachycardia (atrial fibrillation) Enlarged thyroid High TSH, inability to produce T3/T4 Thyroid stimulating antibodies (Graves') Patient with pre-existing hyperthyroid disease Graves' or toxic multinodular goiter Surgery, trauma, infectionMassive catecholamine surgeFever, deliriumTachycardia with death from arrhythmiaHyperglycemia (catecholamines/thyroid hormone)Hypercalcemia (bone turnover)Wikipedia/Public Domain10
Lab FindingsLab Findings Best initial test is TSH Most disorders are primary disease TSHLab FindingsReverse T3 Central hyper/hypo thyroid disease Disorder of the thyroid glandTSH is opposite thyroid hormoneHypothyroidism TSH with low T3/T4Hyperthyroidism TSH with high T3/T4 Isomer of T3 also derived from T4Low TSH and low T3/T4; High TSH and high T3/T4Rare disorders of the pituitary, hypothalamusUsually hypothalamic-pituitary tumorsTumors block secretion TRH/TSH (hypothyroidism)Rarely a TSHoma can secrete TSH (hyperthyroidism)Pituitary resistance to thyroid hormone (hyperthyroidism)Reverse T3Thyroxine (T4)Triiodothyronine (T3)Reverse T3Hyperthyroidism Level usually parallels T4 Low T4 Low rT3 One special use: Euthyroid sick syndrome Critically ill patients low TSH Low T3/T4 Can look like central hypothyroidism rT3 rises in critical illness (impaired clearance) Critically ill patient with low TSH/T4/T3 Check rT3 Low central hypothyroidism High sick euthyroid syndrome11Graves' disease (#1 cause)Toxic multinodular goiterAmiodaroneIodine loadEarly thyroiditis
Graves' DiseaseGraves' Disease Autoimmune disease Thyroid stimulating antibodies produced Symptoms of hyperthyroidism occur Exophthalmos (bulging eyes) Proptosis (protrusion of eye) and periorbital edema Usually no ocular symptomsPretibial myxedema (shins)T-cell lymphocyte activation of fibroblastsFibroblasts contain TSH receptorStimulation secretion of glycosaminoglycans Hydrophilic substances, mostly hyaluronic acid Draws in water swellingGraves' DiseaseGraves' Disease Diagnosis: Usually hyperthyroid labs plus exophthalmos Can measure TSH receptor antibodies “Thyroid stimulating immunoglobulins” TreatmentJonathan Trobe, M.D./Wikipedia Symptoms: beta blockers, thionamides Drugs often started in preparation for definitive therapy Radioactive iodine ablation or surgeryHerbert L. Fred, MD and Hendrik A. van DijkThionamidesThionamides Methimazole Skin rash (common) Agranulocytosis Inhibits thyroid peroxidase (TPO) Organification of iodine Coupling of MIT/DIT Propylthiouracil (PTU) Inhibits TPO Also inhibits 5’-deiodinase Blunts peripheral conversion T4 T3Rare drop in WBCMay present as fever, infection after starting drugWBC improves with stopping drugAplastic anemia cases reported Hepatotoxicity12
Thyroid StormThionamidesTreatment Methimazole: teratogen Propranolol Associated with congenital malformations Especially 1st trimester PTU often used during early pregnancy Beta blocker Blocks T4 T3 conversion Thionamides (PTU, Methimazole) SSKI (saturated solution of potassium iodide) Iodide load shuts down T4 production Wolff-Chaikoff effect Steroids Reduce T4 T3 conversion Suppress auto-immune damage Treat possible concomitant adrenal insufficiencyGraves' Ophthalmopathy Toxic Adenomas Nodules in thyroid that function independentlySometimes worsens despite treating hyperthyroidismCan cause irritation, excessive tearing , painSymptoms often worse by cold air, wind, bright lightsSevere inflammation treatments: Steroids Radiation SurgeryUsually contain mutated TSH receptorDo not respond to TSHOne nodule: Toxic adenomaMultiple: Toxic multinodular goiter Findings: Palpable nodule Hyperthyroidism symptoms/labs Treatment: Radioactive iodine or surgeryJonathan Trobe, M.D./WikipediaJod-Basedow PhenomenonRadioactive Iodine Uptake Iodine-induced hyperthyroidism Often occurs in regions of iodine deficiencyImportant test for thyroid nodulesAdministration of I131 (lower dose than ablation)Contraindicated in pregnancy/breast feeding“Hot” nodule Introduction of iodine hyperthyroidism Often occurs in patients with toxic adenomas Takes up I131 Not-cancerous “Cold” nodule Chance of cancer ( 5%) Often biopsied (Fine-needle aspiration)13Drugs administered with high iodine contentExpectorants (potassium iodide)CT contrast dyeAmiodarone
AmiodaroneHypothyroidism Two types of hyperthyroidism Type I Occurs in patients with pre-existing thyroid disease Graves' or Multi-nodular goiter Amiodarone provides iodine excess hormone production Type II Iodine deficiencyIodine excessCongenital hypothyroidismAmiodaroneThyroiditis Hashimoto’s (#1 cause when dietary iodine is sufficient) Subacute Riedel’sDestructive thyroiditisExcess release T4/ T3 (no hormone synthesis)Direct toxic effect of drugCan occur in patients without pre-existing thyroid illnessIodine DeficiencyIodine Excess “Endemic goiter” Excessive iodide in diet could lead to hyperthyroidism Thyroid protects itself via Wolff-Chaikoff Effect Organification inhibited by iodide Goiter in region with widespread iodine deficiency Common in mountainous areas (iodine depleted by run-off) Constant elevation of TSH enlarged thyroid Less synthesis of MIT/DIT Chronic, high iodine intake goiter/hypothyroidismWellcome ImagesIodineDeficiencyIodineExcessHypothyroidism HypothyroidismWolff-ChaikoffGoiterGoitrogens LoadHyperthyroidism14Substances that inhibit thyroid hormone productionMost common is iodineLithium (inhibits release of thyroid hormone)Certain foods (cassava and millet)
AmiodaroneAmiodarone Can cause hypothyroidism Excess iodine Wolff-Chaikoff Effect Suppression of thyroid hormone synthesis Normal patients “escape” in few weeks Pre-existing subclinical thyroid disease “failure to escape”Hypothyroidism Also mimics T4Iodine Excess Inhibits 5’-diodinaseHypothyroidismWolff-ChaikoffIodine LoadThyroiditisHypothyroidism T4 T3CNS and Bone effects Most common treatable cause intellectual disability Newborn screening programs TH required for normal bone growth/CNS maturation Childhood hypothyroidism cretinism Stunted growth Intellectual impairment Measure T4 or TSH from heel-stick blood specimens CausesIodine deficiencyThyroid dysgenesisInborn errors of hormone synthesis (dyshormonogenesis)TPO most commonThyroid HormoneIatrogenic HypothyroidismCNS and Bone effects Inhibits5’-diodinaseHyperthyroidismThyroid HormoneCongenital Hypothyroidism AmiodaroneAlways check TSHbefore startingamiodarone Thyroid surgeryIntellectual impairmentCoarse facial featuresShort statureUmbilical herniaEnlarged tongue Often done for Graves' or malignancy Radioiodine therapy I131 administered orally as solution or capsuleBeta-emissions tissue damageAblation of thyroid function over weeksDone for Graves' or malignancy Neck radiation Hodgkin’s lymphoma Head and neck cancerWellcome Images/Wikipedia15
Hashimoto’s ThyroiditisHashimoto’s ThyroiditisChronic Autoimmune ThyroiditisChronic Autoimmune Thyroiditis Most common cause of hypothyroidism (non-diet) Lymphocytes infiltrate thyroid gland Antibodies produced Anti-TPO Anti-thyroglobulin Autoimmune disorder (T-cell attack thyroid; B cell activation) HLA-DR3, HLA-DR5 and others Histology: Massive lymphocytic infiltrate (germinal centers) Hurthle cells (enlarged eosinophilic follicular cells)Hashimoto’s ThyroiditisSubacute ThyroiditisChronic Autoimmune Thyroiditis de Quervain’s/granulomatous thyroiditis Primarily occurs in womenEnlarged non-tender thyroid glandGradual loss of thyroid function symptomsSymptoms/labs of hypothyroidismTreatment: thyroid hormone replacementIncreased risk of Non Hodgkin B cell lymphoma Anti-inflammatories (aspirin, NSAIDs, steroids) Thyroid symptoms usually mild (no treatment) Usually resolves in few weeksLymphocytic ThyroiditisRiedel’s Thyroiditis Granulomatous inflammation of thyroidOccurs in young femalesTender, enlarged thyroid glandHyperthyroid euthyroid hypothyroidTreatment:Painless Thyroiditis Variant of Hashimoto’s Lymphocytic infiltration of thyroid gland Transient hyperthyroidismFibroblast activation/proliferationFibrous tissue (collagen) deposition in thyroid“Rock hard” thyroidOften extends beyond the thyroid Can look like Graves' without eye/skin findings Serum thyroid stimulating immunoglobulins not elevated Parathyroid glands hypoparathyroidism Recurrent laryngeal nerves hoarseness Trachea compression difficulty breathing Followed sometimes by hypothyroidism Can look like Hashimoto’s Associated with IgG4 plasma cells Usually self-limited (weeks) May be an “IgG4-related disease” (autoimmune pancreatitis) IgG4 plasma cells identified in biopsy specimens16
Thyroid CancerGeneral Principles Thyroid CancerThyroid cancer usually no hyper/hypo symptomsOften presents as noduleDifferential is benign adenoma versus cancerBiopsy done by fine needle aspirationJason Ryan, MD, MPHThyroid ImagingRadioactive Iodine Uptake Ultrasound Some characteristics suggest cancer Borders, vascularity, calcifications Most cancers do not make hormone About 10% cold nodules are malignantNevit Dilmen/WikipediaFollicular Adenoma Small oral dose I131 given to patientScintillation camera image of thyroidNormal: diffuse, even uptakeDiffuse high uptake: Graves'Diffuse low uptake: Hashimoto’sMultiple areas of high uptake: nodular goiterSingle “hot” nodule: adenomaSingle “cold” nodule: Possible cancerThyroid Cancer Common cause of thyroid nodulesBenign proliferation of folliclesNormal follicular tissue seen on biopsyCompletely surrounded by fibrous capsuleFNA cannot distinguish between adenomas/cancer Cannot see entire capsule Follicular carcinoma has similar histology by FNA FNA follicular pathology followed over time Growth, suspicious new findings han /Wikipedia
Papillary CarcinomaPapillary Carcinoma Most common form thyroid cancer ( 80%) Increased risk with prior radiation exposure Childhood chest radiation for mediastinal malignancy or acne Survivors of atomic bomb detonation (Japan) Nuclear power plant accidents (Chernobyl) Presents as thyroid nodule Sometimes seen on chest/neck imaging (CT/MRI) Diagnosis made after fine needle aspiration (FNA) Excellent prognosis Treated with surgery plus radioactive iodine ablationKGH/WikipediaPapillary CarcinomaPsammoma Bodies Three key pathology findings: Calcifications with an layered pattern Seen in other neoplasms but only papillary for thyroid Psammoma bodies Nuclear grooves Orphan Annie’s Eye Nuclei Diagnosis made by nuclear findingsWikipedia/Public DomainNuclear GroovesOrphan Annie's Eyes Empty-appearing nucleiKGH/WikipediaWhite clearingKGH/Wikipedia18William Creswell/Flikr
Follicular Carcinoma Follicular Carcinoma Possible hematogenous metastasis Treatment:Similar to follicular adenomaBreaks through (“invades”) fibrous capsuleFNA cannot distinguish between adenomas/cancerFollicular pathology followed over time Thyroidectomy I131 to ablate any remaining tissue or metastasis Growth, suspicious new findings surgeryYale Rosen/WikipediaMedullary CarcinomaMedullary Carcinoma Cancer of parafollicular cells (C cells) Produces calcitoninMalignant cells/Amyloid “stroma” Lowers serum calcium Normally minimal effect on calcium levels Used for monitoring Amyloid deposits in thyroid Amyloid protein deposits Calcitonin peptide Appearance of amyloid on biopsyNephron/WikipediaMEN SyndromesAnaplastic CarcinomaMultiple Endocrine NeoplasiaUndifferentiated Carcinoma Occurs in elderly Highly malignant - invades local tissues Gene mutations that run in families Cause multiple endocrine tumors MEN 2A and 2B associated with medullary carcinoma Caused by RET oncogene mutation Some patients have elective thyroidectomyDysphagia (esophagus)Hoarseness (recurrent laryngeal nerve)Dyspnea (trachea)Don’t confuse with Riedel’s (“rock hard” thyroid/young pt) Poor prognosis Pathology: Undifferentiated cells No papilla, follicles, or amyloid19
Adrenal GlandsAdrenal Glands Located above kidneys Arteries: Suprarenal arteries Left and right Superior, inferior, middle Veins:Adrenal Glands Left adrenal renal vein IVC Right adrenal IVCJason Ryan, MD, MPHWikipedia /Public DomainCortex and MedullaSignal Transmission Cortex: Three groups of hormones Mineralocorticoids (aldosterone)Glucocorticoids (cortisol)Androgens (testosterone)Derived from mesoderm Medulla Epinephrine and norepinephrine Sympathetic nervous system control Derived from neural crestOpenStax College/WikipediaUse with permission, Katzung BG, Basic and Clinical Pharmacology, 10th ed. New York, McGraw Hill, 2007MineralocorticoidsCollecting DuctLumen (Urine) Most important is aldosterone Key effects on kidney function Release controlled by RAA systemAldosterone Renin-angiotensin-aldosterone Increase Na /Water resorption Promote K /H excretionAldosteroneCorticosteroneK Principal CellNa AldosteroneH2OIntercalated CellAldosterone11-deoxycorticosterone20H ATPNa K Interstitium/Blood
Adrenal AndrogensCortisol Small contribution to androgen production in males 50% androgens for females Clinical relevance: congenital adrenal hyperplasia Major glucocorticoid Synthesized by adrenal cortex Binds to intracellular receptors (cytosol) Glucocorticoid receptor (GR) Over/underproduction abnormal sexual development Production stimulated by ACTH (like cortisol)Dehydroepiandrosterone(DHEA)Testosterone Translocates to nucleus Activates/suppresses gene transcriptionAndrostenedionePituitary-Adrenal AxisCircadian Rhythms Controls cortisol secretion Hypothalamus: CRH Serum cortisol highest early morning (about 6 AM) 10 to 20 mcg/dL Lowest one hour after sleep onset Corticotropin releasing hormone Paraventricular nucleus (PVN) Less than 5 mcg/dL Anterior pituitary: ACTH Testing rarely done with single blood test Adrenocorticotropic hormone Acts on adrenal gland cAMP/PKA 2nd messenger Adrenal: CortisolCortisolDrosenbach/WikipediaCortisol Binding Globulin Cortisol poorly soluble in plasma Most ( 90%) serum cortisol bound to CBG Levels estrogenCortisolHormone Effects Maintains blood pressureCortisol Effects on vascular smooth muscle Increases vascular sensitivity (α1) to norepi/epi NO mediated vasodilationCortisol cortisol: hypertension (Cushing’s disease) cortisol: hypotension (adrenal insufficiency)21
CortisolHormone Effects Suppresses immune system Sequester lymphocytes in spleen/nodesCortisolCortisol Inactivate NF-KB Reduce T and B cell levels in plasma Block neutrophil migration peripheral neutrophil count Mast cells: blocks histamine release eosinophil counts Basis for steroids as immunosuppressive drug therapyCorticosteroid DrugsCortisolEffectsCortisol More glucose produced by liver synthesis of glucose 6-phosphatase, PEPCK eMethylprednisoloneBetamethasoneCortisolEffects Activation of lipolysis in adipocytes free fatty acids total cholesterol, triglyceridesKey inflammatory transcription factorMediates response to TNF-αControls synthesis inflammatory mediatorsCOX-2, PLA2, LipoxygenaseCortisolCortisol Less glucose taken up peripherally (muscle, fat) Net results: serum glucose More glycogen storage in liver synthesis of glycogen isol Enhanced effects of glucagon, epinephrine Leads to insulin resistance Long term steroid use: diabetes Stimulate adipocyte growth Key effect: fat deposition22Cortisol
CortisolEffectsZones of the Adrenal GlandsCortisol Muscle atrophy Skin effects Blunted epidermal cell division in skin collagen, inhibition of fibroblasts Net effects: Thin skin, easy bruising, striae Bones: Inhibits osteoblasts Steroids osteopenia and osteoporosisJpogi/Wikipedia /Public DomainZones of the Adrenal GlandsZona GlomerulosaProgesteronePregnenoloneCholesterol3-β hydroxysteroidDehydrogenase21-α hydroxylase11-β hydroxylaseAldosteroneZona GlomerulosaPregnenoloneCholesterolAngiotensin II xycorticosteroneCorticosteroneZona Glomerulosa3-β erol21-α hydroxylaseDesmolase PregnenoloneAngiotensin II AldosteroneSynthase11-β icosterone3-β hydroxysteroidDehydrogenaseProgesterone21-α hydroxylase11-β hydroxylase11-deoxycorticosterone
Zona GlomerulosaPregnenoloneZona FasciculataProgesterone17-α hydroxylase3-β ikipedia /Public Domain17-HydroxypregnenoloneZona FasciculataZona ReticularisCortisol17-Hydroxyprogesterone21-α hydroxylase11-β 7, 20 lyase3-β DHEA)AndrostenedioneTestosteroneMatthew Colo/WikipediaKetoconazole Antifungal Blocks ergosterol synthesis in fungi Potent inhibitor of 17,20 lyase androstenedione/testosterone Key side effect: gynecomastia Also inhibits 17-alpha hydroxylase, desmolase Blocks cortisol synthesis Can be used to treat Cushing’s syndrome24
CAHCongenitalAdrenal HyperplasiaCAHCongenital Adrenal Hyperplasia Enzyme deficiency syndrome Loss of one of the four enzymes for cortisol synthesis 21-α hydroxylase11-β hydroxylase17-α hydroxylase3-β hydroxysteroid dehydrogenaseJason Ryan, MD, MPHCAHCongenital Adrenal HyperplasiaACTHAldosteroneMatthew Colo/WikipediaCAHLow CortisolCongenital Adrenal HyperplasiaSigns/Symptoms All result in low cortisol Stimulates ACTH release Can cause production of other hormones Hypoglycemia Nausea/vomiting Mineralocorticoids Androgens Cortisol ACTHAdrenalHyperplasia Non-cortisolhormone synthesis25CholesterolCortisolAndrogens page
This book of slides is intended as a companion to the videos for . Measure T4 or TSH from heel -stick blood specimens Thyroid Hormone CNS and Bone effects . Cold intolerance Weight gain with