Transcription
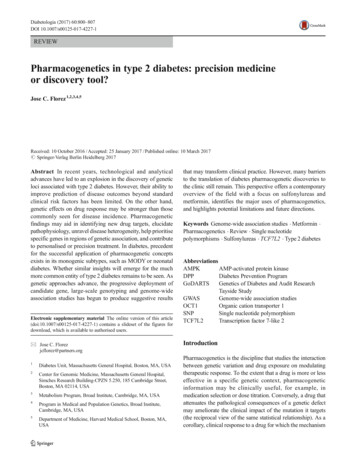
Diabetologia (2017) 60:800–807DOI 10.1007/s00125-017-4227-1REVIEWPharmacogenetics in type 2 diabetes: precision medicineor discovery tool?Jose C. Florez 1,2,3,4,5Received: 10 October 2016 / Accepted: 25 January 2017 / Published online: 10 March 2017# Springer-Verlag Berlin Heidelberg 2017Abstract In recent years, technological and analyticaladvances have led to an explosion in the discovery of geneticloci associated with type 2 diabetes. However, their ability toimprove prediction of disease outcomes beyond standardclinical risk factors has been limited. On the other hand,genetic effects on drug response may be stronger than thosecommonly seen for disease incidence. Pharmacogeneticfindings may aid in identifying new drug targets, elucidatepathophysiology, unravel disease heterogeneity, help prioritisespecific genes in regions of genetic association, and contributeto personalised or precision treatment. In diabetes, precedentfor the successful application of pharmacogenetic conceptsexists in its monogenic subtypes, such as MODY or neonataldiabetes. Whether similar insights will emerge for the muchmore common entity of type 2 diabetes remains to be seen. Asgenetic approaches advance, the progressive deployment ofcandidate gene, large-scale genotyping and genome-wideassociation studies has begun to produce suggestive resultsElectronic supplementary material The online version of this article(doi:10.1007/s00125-017-4227-1) contains a slideset of the figures fordownload, which is available to authorised users.* Jose C. Florezjcflorez@partners.org1Diabetes Unit, Massachusetts General Hospital, Boston, MA, USA2Center for Genomic Medicine, Massachusetts General Hospital,Simches Research Building-CPZN 5.250, 185 Cambridge Street,Boston, MA 02114, USA3Metabolism Program, Broad Institute, Cambridge, MA, USA4Program in Medical and Population Genetics, Broad Institute,Cambridge, MA, USA5Department of Medicine, Harvard Medical School, Boston, MA,USAthat may transform clinical practice. However, many barriersto the translation of diabetes pharmacogenetic discoveries tothe clinic still remain. This perspective offers a contemporaryoverview of the field with a focus on sulfonylureas andmetformin, identifies the major uses of pharmacogenetics,and highlights potential limitations and future directions.Keywords Genome-wide association studies . Metformin .Pharmacogenetics . Review . Single nucleotidepolymorphisms . Sulfonylureas . TCF7L2 . Type 2 diabetesAbbreviationsAMPKAMP-activated protein kinaseDPPDiabetes Prevention ProgramGoDARTSGenetics of Diabetes and Audit ResearchTayside StudyGWASGenome-wide association studiesOCT1Organic cation transporter 1SNPSingle nucleotide polymorphismTCF7L2Transcription factor 7-like 2IntroductionPharmacogenetics is the discipline that studies the interactionbetween genetic variation and drug exposure on modulatingtherapeutic response. To the extent that a drug is more or lesseffective in a specific genetic context, pharmacogeneticinformation may be clinically useful, for example, inmedication selection or dose titration. Conversely, a drug thatattenuates the pathological consequences of a genetic defectmay ameliorate the clinical impact of the mutation it targets(the reciprocal view of the same statistical relationship). As acorollary, clinical response to a drug for which the mechanism
Diabetologia (2017) 60:800–807801of action in carriers of a specific variant is known can also beinformative with regard to the function of the gene affected bythe variant [1].In recent years, pharmacogenetic studies have been greatlyfacilitated by the growing catalogue of human geneticvariation, as well as parallel technological advances thatenable the high-throughput generation of genetic data in largepopulations. These have taken the form of targetedexplorations of known genetic variants (e.g. in genes thatencode proteins known to affect the pharmacokinetic orpharmacodynamic properties of a given drug), or of agnosticsearches that query the entire genome to search for variantsthat influence drug response. Proof-of-concept approacheshave been immensely successful in oncology, where designdrugs have targeted unique somatic mutations that occur in thepatient’s tumour. Whether similar approaches are likely tosucceed for germline (inherited) genetic variation, particularlyfor complex polygenic diseases such as type 2 diabetes, is thetopic of this review.Multiple reports of associations between genetic variantsand drug response for any one of the 12 drug classes currentlyapproved for the treatment of type 2 diabetes have beenpublished [2–4], although the degree of confidence in thereported results varies greatly. To a large extent, this is dueto the limited sample sizes currently available for studies intonon-generic drugs, as most such studies are the province ofindividual pharmaceutical companies, and firm executivesmay be wary of limiting the marketability of a proprietarycompound by attaching a genetic indication. Similarly,successful pharmacogenetic approaches for targetidentification in the pursuit of drug discovery may remainprivate until the new drug is brought to market. Thus,academic investigators are often limited to working withgeneric drugs, and perturbation trials that use novel agentsare typically restricted to sample sizes that are too small togenerate robust statistical confidence. Nevertheless, thefollowing sections offer examples that illustrate how thesethree distinct approaches have been applied in type 2 diabetes.Goals of pharmacogenetic studiesPatient stratification: sulfonylureas in monogenicand polygenic diabetesBecause of the richness inherent to pharmacogenetic data andthe diverse perspectives from which they can be interpreted, itis crucial to clarify the purpose of each research exerciseupfront. Study design, analysis of results and biologicalinference may vary depending on the goals and hypothesesthat guide a given experiment. Pharmacogenetic studies maypursue one or several major objectives:1. Patient stratification Genetic information may be usedto define subgroups of individuals more or less likely toexperience clinical response to the drug in question, or todevelop side effects. This is the hope articulated by precisionmedicine, which aspires to administer the right medication tothe right patient at the right time.2. Target identification Genetic studies may help with thediscovery of novel drug targets that illuminate mechanisms ofaction and open new therapeutic avenues, particularly if theirscope is genome-wide and their approach is unbiased.3. Functional characterisation Drugs can also be used toperturb the human organism in vivo. If such a perturbationgenerates a physiological response that differs depending ongenetic variation at a specific locus, insights may be gainedwith respect to the mode of action of the gene product, or thecell type in which it is expressed. In this manner, pharmacogenetic experiments can offer proof-of-concept evidence thatimplicates a given gene in a molecular pathway andstrengthens the evidence suggesting that an observed association is causal.Neonatal diabetes: mutations in ABCC8 or KCNJ11The ability to clearly separate patients into respondersand non-responders is largely predicated on the magnitudeof the genetic effect on drug bioavailability or efficacy(pharmacokinetics and pharmacodynamics), or on the clinicalphenotype the drug is meant to correct. Therefore, monogenicsyndromes (where a single mutation has a strong effect onphenotype) constitute the natural theatre in which to attemptclinical validation. In diabetes, the cleanest example isprovided by neonatal diabetes caused by activating mutationsin the genes that encode the sulfonylurea receptor (ABCC8) orits associated ATP-dependent potassium channel (KCNJ11),which lie adjacent to each other in chromosome 11.Constitutively activating mutations that lead to hyperactivityof this complex impair the ability of beta cells to depolarise inresponse to a glucose stimulus, hindering insulin secretionand causing insulin insufficiency [5, 6]. The resultinghyperglycaemia is typically detected in the first year of lifeand must be distinguished from the autoimmune destructionof pancreatic beta cells that occurs in type 1 diabetes. Thoughvery early onset ( 6 months) and the absence ofautoantibodies favour the diagnosis of neonatal diabetes,genetic confirmation is typically required [7]. In many of thesecases, the genetic defect can be overcome by high doses of thevery same medication class (sulfonylureas) that targets thesulfonylurea receptor/potassium channel complex [6, 8].Patients with documented mutations in the relevant genescan be safely transitioned to an oral regimen and shed multiple
802daily insulin injections; their sustained improvement inglycaemic response demonstrates that the use ofpharmacogenetic information in patient care can improve notonly the quality of care but also the quality of life.Type 2 diabetes: polymorphisms in KCNJ11 and ABCC8Other variants at the KCNJ11–ABCC8 gene locus that haveweaker effects increase risk of common type 2 diabetes.The T allele at the common missense single nucleotidepolymorphism (SNP) rs5219 in KCNJ11, by which aglutamate becomes a lysine at position 23 (E23K), raises theodds of type 2 diabetes by 15% [9]. Carriers alsodemonstrate diminished insulin secretion in response to aglucose challenge, though not to the extent seen in neonataldiabetes [10]. However, the E23K polymorphism in KCNJ11is in near-complete linkage disequilibrium with anothermissense polymorphism in the adjacent gene ABCC8(rs757110), by which a serine becomes an alanine at position1369 of the sulfonylurea receptor (S1369A). As a result,virtually every carrier of the risk K allele at KCNJ11 carriesthe A allele at ABCC8, making it impossible to distinguish thesource of the association signal on purely genetic grounds[10]. To discriminate between the two variants experimentalmanipulation is required, as human genetic evolutionaryhistory has not separated them via recombination. Potassiumcurrents can be measured in vitro by patch-clamp techniquesapplied to human cells transfected with the recombinantconstruct; the activation of the potassium current aftergliclazide administration is diminished in cells transfectedwith the A1369/K23 haplotype, reflecting the human geneticdefect [11]. When the constructs are scrambled to generate thefour possible combinations at the two sites, the A1369/K23and A1369/E23 constructs display reduced conductance whencompared with the S1369/K23 and S1369/E23 constructs,demonstrating that, for gliclazide response, the likely culpritvariant is A1369 in ABCC8, and not K23 in KCNJ11.To take this finding into human populations, Chineseinvestigators tested two cohorts of participants with type 2diabetes of relatively recent onset [12]. All participantsresponded to gliclazide treatment by improvements in fastingglucose and HbA1c levels after 2 months, but carriers of theA1369 polymorphism had a significantly stronger response,with an additional improvement in fasting glucose of 0.67 mmol/l when compared with S1369 carriers, a findingthat is clinically significant. This result has been replicatedusing HbA1c as the response metric and KCNJ11 E23K asthe genetic marker [13]. It recapitulates the observation inneonatal diabetes and suggests that sulfonylureas can be usedto overcome genetic defects in their molecular target. A smallstudy did not reveal higher incidence of hypoglycaemiacaused by this heightened sensitivity [14]; whether differencesin medication potency could be addressed by simplyDiabetologia (2017) 60:800–807increasing the administered dose has not been tested.Similarly, it is entirely possible that preferential effectivenessof sulfonylureas may only manifest itself early in the diseasecourse, when beta cell function has not yet markedlydeteriorated. As discussed further (below), the particularmetabolic state of an individual may contribute additionalvariability to gene drug interactions.Target identification: the elusive molecular targetof metforminMetformin is the first-line agent in the treatment of type 2diabetes [15–17]. Because of its effectiveness, low cost andfavourable side effect profile, metformin is recommended asthe first choice by all professional organisations (in the absenceof contraindications) and is used in this manner by healthcarepractitioners worldwide [18]. Nevertheless, hyperglycaemiaeventually progresses in a substantial number of patients, necessitating the escalation of therapy [19]. Of particular concernare the number of young people who eventually fail metformin[20] and our inability to predict in whom metformin will besufficient.Molecular mechanisms of metformin actionDespite metformin being available for several decades and itswidespread use, the precise manner by which metformininhibits hepatic gluconeogenesis and improves insulinsensitivity has not been elucidated [21]. It has been shownto inhibit mitochondrial complex I [22, 23] and therebyactivate AMP-activated protein kinase (AMPK) [24, 25], butit is not clear if such activation is dependent on a direct interaction between metformin and mitochondrial proteins orAMPK, or if it occurs via the mediation of other signallingmolecules (Fig. 1). Recent loss-of-function experiments haveshown that AMPK is not essential for metformin activity [26],indicating that much remains to be clarified about metformin’smolecular interactions in the cell and its specific targets. Arecent study implicates cAMP signalling as a major target ofmetformin, but this is also likely to be caused by indirecteffects [27]. Such a gap in our knowledge has precluded thedevelopment of analogous therapies that might target therelevant pathways.The impact of genetic variants on metformin responseThe genetic parsing of metformin responders remainssimilarly underexplored [3, 28]. A few candidate gene studieshave attempted to identify genetic predictors of metforminresponse.
Diabetologia (2017) ondriaFBPasePKALipid and cleusLipogenic gene expressionGluconeogenesisComplex IGluconeogenic gene expressionPyruvateFig. 1 Proposed molecular mechanisms of the blood-glucose loweringaction of metformin. Metformin is transported into the hepatocyte byOCT1 and inhibits mitochondrial complex I via unknown mechanisms.As a result gluconeogenesis is impaired by: (1) decreased ATP andincreased AMP (direct inhibition caused by the energy/ATP deficit);and (2) increased AMP, which interferes with cAMP–protein kinase Asignalling, thus inhibiting fructose-1,6-bisphosphatase activity(a gluconeogenic enzyme). Increased AMP also leads to AMPKactivation, thus reducing lipid/cholesterol synthesis and promotingbeneficial long-term therapeutic effects. FBPase; fructose-1,6-bisphosphatase; OCT1, organic cation transporter 1; PKA, proteinkinase A. Figure redrawn from Rena et al [57], under the CreativeCommons Attribution 4.0 International (CC BY) 0)SLC22A1 In a small cohort, missense variants in the organiccation transporter 1 (OCT1, encoded by SLC22A1) wereassociated with a reduced response to metformin [29];subsequent follow-up in a large clinical retrospective cohortof patients with type 2 diabetes (the Genetics of Diabetes andAudit Research Tayside Study [GoDARTS]) failed to findsupport for such an association [30]. On the other hand, whencombined with drugs that impair OCT1 function, loss-offunction variants at this locus increase the incidence ofgastrointestinal side effects (Fig. 2) [31].SLC47A1 A pilot study in a small clinical retrospectivecohort from Rotterdam (the Netherlands) identified acommon polymorphism in the metformin transportermultidrug and toxin extrusion 1 (MATE1; encoded bySLC47A1, and responsible for disposing of metformin intobile and urine) as being associated with metforminr e s p o n s e in p a t i e n t s w i t h t y p e 2 d i a b e t e s [ 3 2 ] .Accordingly, we found supportive evidence for a varianthighly correlated with the index variant in the DiabetesDiabetes incidence(cases/100 person-years)Risk of gastrointestinal side effects(OR)125432108642100Placebo 1 RA 1 RA 1 RA 1 RAFig. 2 When combined with drugs that interfere with OCT1 function,risk alleles (RA) at OCT1 increase the incidence of gastrointestinal sideeffects. Such drugs include tricyclic antidepressants, citalopram,proton-pump inhibitors, non-dihydropyridine calcium channel blockers,doxazosin, spironolactone, clopidogrel, rosiglitazone, quinine, tramadoland codeine. Purple bars, without drugs; blue bars, with drug(s). Dataobtained from [31]MetforminLifestyleFig. 3 Illustration of a gene drug interaction. The genotype atSLC47A1 (SNP rs8065082) interacts with metformin in modulatingdiabetes incidence in DPP participants (pint 0.006). Genotypes: CC,red bars; CT, purple bars; TT, blue bars. Data obtained from [33];American Diabetes Association (Diabetes, American DiabetesAssociation [2010]). Copyright and all rights reserved. Material from thispublication has been used with the permission of American DiabetesAssociation
804Prevention Program (DPP), a randomised clinical trial thatallocated participants at high risk of developing diabetes toplacebo, lifestyle modification or metformin interventions(Fig. 3) [33]. This finding has been replicated in one smallcohort [34] but not in a large-scale meta-analysis [35]. Ashas been the case for many other phenotypes, candidategene studies have failed to produce a comprehensivepicture of the genetic determinants of metformin action.ATM Genome-wide association studies (GWAS) offer theopportunity to mine the entire genome for common variantsassociated with metformin response in an unbiased manner. Inthe first published GWAS for metformin response, theGoDARTS investigators analysed 705,125 SNPs in 1024individuals in their retrospective clinical database. FourteenSNPs in or near the gene encoding ataxia-telangiectasiamutated kinase (ATM) were associated with categoricalmetformin response (defined as HbA 1c reaching 7%[ 53 mmol/mol] within 18 months of starting therapy) atp 10 6. Consistent results were obtained for change inHbA1c as a quantitative trait. Replication was attained forthe top SNP (rs11212617) in 1783 additional GoDARTSparticipants and 1113 participants in the UK ProspectiveDiabetes Study (UKPDS) clinical trial [36], with joint analysisexceeding conventional genome-wide statistical significance(p 3 10 9). Although this association has been replicatedelsewhere [37], we have not found support for such anassociation in the DPP [38], using diabetes incidence orchange in quantitative glycaemic traits as endpoints.SLC2A2 Sample size is essential for genetic discovery. TheMetformin Genetics (MetGen) Consortium has recentlycoalesced to assemble the largest resource of samples withDNA and information relevant to metformin response [39];the majority of participants include patients with type 2diabetes who have received metformin in the course ofroutine clinical care, and for whom glycaemic profiles areavailable in the form of serial HbA1c measurements. In arecent report [40], the original genome-wide screen fromt h e p r e v io u s p u b l i c a t i o n w a s e x t e n d e d to 1 3 7 3participants, with suggestive association signals undergoing three replication stages totalling nearly 14,000participants. In this cohort, SNP rs8192675 in an intronof the gene SLC2A2 (encoding the glucose transporterGLUT2) was associated with reduction in HbA 1c atgenome-wide significance. This variant has both a primaryeffect on pre-metformin HbA 1c and an effect on posttreatment HbA 1c levels when adjusted for the baselinemeasurement. The same variant influences GLUT2expression in the human liver, the tissue in which it isprimarily expressed (though it is also present in beta cells)[41]. The genotype-driven difference approaches 0.33%,with 0.50% typically used as a marker of glycaemicDiabetologia (2017) 60:800–807response that merits regulatory approval for a new drug. Theeffect translates to a dose difference of 550 mg of metformin,again suggesting that perhaps differences in potency can becompensated by higher doses in the poorer responders.Similarly, we have not found evidence that this variant affectsthe ability of metformin to prevent diabetes in DPP participants with impaired glucose tolerance at baseline, indicatingthat perhaps genetic influences on drug response are alsodependent on the metabolic state of the individual, withdifferential interactions occurring at diverse stages of diseaseprogression. In this sense, pharmacogenetic findings fordiabetes treatment may not overlap perfectly with those fordiabetes prevention [42].Functional characterisation: TCF7L2and pharmacogenetics as a discovery toolThe end-result of a GWAS, per se, is the identification ofa genomic region harbouring a polymorphism in which agiven allele is seen more frequently in disease than inhealth. If it is not clear how the polymorphism in questionaffects the expression or function of a nearby gene, theassociation signal may fail to point to a specific gene. Outof several possible candidate genes, one may be favouredif its pattern of expression is most consistent with theobserved pharmacogenetic response (e.g. to an insulinsecretagogue but not to an insulin sensitiser). Even if agene is implicated via fine-mapping or expression studies,the mechanism by which changes in expression or function of its protein product cause type 2 diabetes is seldomobvious.A case in point is TCF7L2. Discovered in 2006 as agene containing a common intronic variant with arelatively strong effect on type 2 diabetes risk [43], it wasnot until 2010 that fine-mapping and functional studiesconclusively proved that the rs7903146 variant was causalin influencing TCF7L2 expression in islets [44], although arecent report suggests that it may act via another effectortranscript [45]. Physiological studies in the DPP firstdemonstrated that this type 2 diabetes-associated variantdiminishes beta cell function [46], but the precisemolecular mechanisms by which the protein encoded byTCF7L2 (transcription factor 7-like 2 [TCF7L2]) does sohave proven elusive. Depending on the experimentalmodel, TCF7L2 has been posited to influence beta cellproliferation early in development [47], proinsulinprocessing [48, 49], insulin vesicle docking [50] or incretinresponse [51, 52], although extra-pancreatic effects havealso been suggested recently [53]. Given its proposed rolein beta cell function, differential response to an insulinsecretagogue might be expected in carriers vis-à-vis noncarriers of the type 2 diabetes risk allele: whether the drug
Diabetologia (2017) 60:800–807805improves response in carriers of the risk allele depends onits point of entry into the insulin secretion pathway relativeto that of the gene. If the gene product acts downstream ofthe sulfonylurea receptor, for example, a sulfonylurea maystill encounter the genetic block in inducing insulin secretion and carriers would show a worse clinical response; onthe other hand, if the gene product acts upstream of thesulfonylurea receptor, a sulfonylurea drug may rescue theability of the beta cell to secrete insulin and carriers woulddisplay a greater benefit.The impact of sulfonylurea therapy by TCF7L2 genotypewas retrospectively examined in the GoDARTS cohort.Treatment with sulfonylurea was less likely to achieveglycaemic goals in carriers of the TCF7L2 risk genotype, aneffect not seen for metformin [54]. Similar effects were seen ina smaller cohort [55]. The tentative conclusion from thesestudies is that TCF7L2 impacts the insulin secretory pathwaydistal to the sulfonylurea receptor, as the drug seems lesseffective in risk allele carriers.However, an alternative explanation could be considered.If variants in TCF7L2 reduce beta cell mass through eitherdecreased proliferation or accelerated degeneration (leadingto lower insulin secretion, a high proinsulin: insulin ratioand diminished efficacy of incretins), when used in patientswith long-standing disease who have a reduced beta cell complement, sulfonylureas might be less effective; this differencewould not be seen in non-diabetic individuals. We have conducted the Study to Understand the Genetics of the AcuteResponse to Metformin and Glipizide in Humans (SUGARMGH), a pharmacogenetic resource in which 1000 participants who were naive to antihyperglycaemic medicationswere given a single dose of glipizide followed by a shortcourse of metformin, and glycaemic responses were measuredin the acute setting (Fig. 4) [56]. In addition, incretin hormones were measured after an OGTT. This cohort replicatesthe known association of the T risk allele at TCF7L2rs7903146 with fasting glucose, and can be used to ascertainParticipantsn 1000Naive to diabetesmedicationsTargeted individuals athigher riskDay 1whether the differentially worse response to sulfonylureas in Tallele carriers with chronic type 2 diabetes observed by theGoDARTS investigators holds in the acute setting.Preliminary results suggest that this is not the case, againindicating that the metabolic state of the individual along thepath of disease progression may modulate pharmacogeneticresponses. On the other hand, indirect evidence confirms thepotential role of incretin resistance in T allele carriers. Takentogether, these findings do confirm that TCF7L2 exerts itseffect on type 2 diabetes risk via its action on the beta cell,possibly by modulating incretin sensitivity (J.C. Florez,unpublished observations).ConclusionsIn pharmacogenetic studies, investigators should clarify apriori what the purpose of the research is, be it patient stratification, target identification or functional characterisation.Monogenic diabetes (neonatal diabetes and MODY) providesproof-of-concept that genetic information can guide therapy.Effect sizes in type 2 diabetes are much smaller but could beclinically meaningful, particularly if aggregated in genetic riskscores; whether this leads to a wider dosing range vs alternative drug choices needs to be tested. Furthermore, determinants of response may be contingent on the metabolic/disease state of the individual or on their developmental stage.As an approach to discovery, agnostic genome-wide studiescan help identify drug targets and modulators of drugresponse; additional benefits include the potential to assesslikelihood of side effects and estimate heritability wherefamily studies are unavailable or impractical. Given the smalleffects observed, whether genetic information improvesclinical outcomes and is cost-effective needs to be studied:the strategy will only be viable if comprehensive genotypingfor all clinically actionable variants is done prospectively bystreamlining testing on a single, once-in-a-lifetime chip.Days 6 and 7Day 8Vital signsMetformin orally (500 mg)Fourth dose of metforminDNA sampleTwice daily75g OGTTGlipizide orally (5 mg), withsubsequent measurement ofglucose, insulin and glucagon at 0, 30, 60, 90, 120, 180and 240 minThree dosesGlucose, insulin and incretinmeasurements over 2 hFood logFig. 4 Design of the Study to Understand the Genetics of the Acute Response to Metformin and Glipizide in Humans (SUGAR-MGH) [56]
806Diabetologia (2017) 60:800–807Funding JCF is supported by an unrestricted Massachusetts GeneralHospital Research Scholar Award. Parts of this work are supported byNIH/NIDDK R01 DK072041, NIH/NIDDK U01 DK105554, NIH/NIGMSR01 GM117163, NIH/NIDDK R01 DK105154, and NIH/NIDDK K24DK110550.16.Duality of interest JCF has received consulting honoraria from Merckand from Boehringer-Ingelheim.17.Contribution statement JCF is the sole contributor to this 4.15.Florez JC (2013) Pharmacogenetic perturbations in humans as atool to generate mechanistic insight. Diabetes 62:3019–3021Maruthur NM, Gribble MO, Bennett WL et al (2014) The pharmacogenetics of type 2 diabetes: a systematic review. Diabetes Care37:876–886Huang C, Florez JC (2011) Pharmacogenetics in type 2 diabetes:potential implications for clinical practice. Genome Med 3:76Zhou K, Pedersen HK, Dawed AY, Pearson ER (2016)Pharmacogenomics in diabetes mellitus: insights into drug actionand drug discovery. Nat Rev Endocrinol 12:337–346Gloyn AL, Pearson ER, Antcliff JF et al (2004) Activating mutations in the gene encoding the ATP-sensitive potassium-channelsubunit Kir6.2 and permanent neonatal diabetes. N Engl J Med350:1838–1849Babenko AP, Polak M, Cave H et al (2006) Activating mutations inthe ABCC8 gene in neonatal diabetes mellitus. N Engl J Med 355:456–466Greeley SA, Naylor RN, Philipson LH, Bell GI (2011) Neonataldiabetes: an expanding list of genes allows for improved diagnosisand treatment. Curr Diab Rep 11:519–532Pearson ER, Flechtner I, Njolstad PR et al (2006) Switching frominsulin to oral sulfonylureas in patients with diabetes due to Kir6.2mutations. N Engl J Med 355:467–477Gloyn AL, Weedon MN, Owen KR et al (2003) Large-scale association studies of variants in genes encoding the pancreatic β-cellKATP channel subunits Kir6.2 (KCNJ11) and SUR1 (ABCC8) confirm that the KCNJ11 E23K variant is associated with type 2 diabetes. Diabetes 52:568–572Florez JC, Burtt N, de Bakker PI et al (2004) Haplotype structureand genotype-phenotype correlations of the sulfonylurea receptorand the islet ATP-sensitive potassium channel gene region.Diabetes 53:1360–1368Hamming KS, Soliman D, Matemisz LC et al (2009) Coexpressionof the type 2 diabetes susceptibility gene variants KCNJ11 E23Kand ABCC8 S1369A alter the ATP and sulfonylurea sensitivities ofthe ATP-sensitive K channel. D
Type 2 diabetes: polymorphisms in KCNJ11 and ABCC8 Other variants at the KCNJ11–ABCC8 gene locus that have weaker effects increase risk of common type 2 diabetes. The T allele at the common missense single nucleotide polymorphism (SNP) rs5219 inKCNJ11,bywhicha glu