Transcription
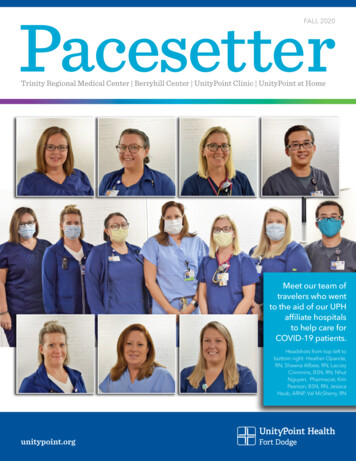
PacesetterFALL 2020Trinity Regional Medical Center Berryhill Center UnityPoint Clinic UnityPoint at HomeMeet our team oftravelers who wentto the aid of our UPHaffiliate hospitalsto help care forCOVID-19 patients.Headshots from top-left tobottom right: Heather Opande,RN, Shawna Allbee, RN, LacceyCrimmins, BSN, RN, NhutNguyen, Pharmacist, KimPearson, BSN, RN, JessicaHaub, ARNP, Val McSherry, RNunitypoint.org
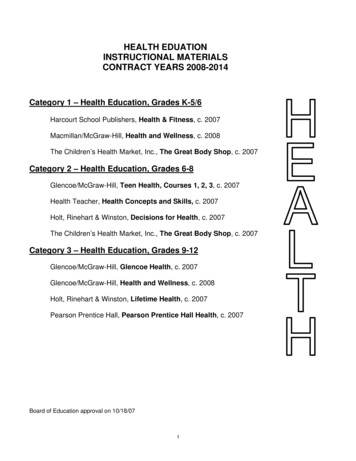
What’sInside3 New Providers4 Celebrating OurEmployees5 Meet CarolynElsberry, RN6 Nursing During COVID11Caring for the Heart12How Are YOU Doing?14 Us vs. COVID20 At Home Visits withYour Provider2022Wait in Your Own SpaceTaking BehavioralHealth Help to Thosein Crisis22When Reaction Turnsto Innovation 23Delivering KindnessPacesetterThe Pacesetter is published by UnityPointHealth – Fort Dodge Marketing andPublic Relations. All rights reserved:No part of this publication may bereproduced or transmitted in any waywithout written permission from TrinityMarketing and Public Relations.Copyright 2020 UnityPoint Health. AllRights Reserved. SM trademarks ofUnityPoint Health.Getting throughCOVID-19 togetherWhile this has been a difficultseason for all of us, as a leaderfor UnityPoint Health – FortDodge, I cannot begin toexpress the pride I feel for howour team has weathered thisstorm. It hasn’t been easy. Yet,our team continues to show-up,they willingly do whatever isneeded to be done, and they doit out of a desire to give the bestcare to our community. In fact,as you can see on this cover, wehave had many nurses travel tohelp other UnityPoint Healthhospitals to provide relief fortheir teams. Firefighters are notthe only ones who run into a fire.I firmly believe storms like this have the ability to make us better, and I knowthis to be true with our team. We quickly eliminated the ‘that can’t be done’philosophy, ‘to how do we make this happen?’ And when a process didn’tturn out as we hoped, we learned how to do it better. Our eyes have neverleft the goal of providing great patient care while keeping our team andpatients safe.Not everything came to a screeching halt during COVID. While it may haveslowed down some projects we were working on, we did our best to keepplans moving forward. Such as our new partnership with Blank Children’sHospital, we will have a full team here by the end of November. The newUnityPoint Clinic Express at the Corridor Plaza (former Crossroads Mall area)will open as soon as the construction is completed. Through our partnershipwith CNOS, we will also welcome Neurology services back to Fort Dodgetwo times a month in November. Additionally, we have some new mentalhealth services that you will read about in this issue.All these things mentioned are what helped me stay positive during thesedays when our world has changed so much. My prayer for you in the weeksand months to come is that you too are able to find the good. We are notfinished with COVID. Do not grow weary, take care of yourself and take careof each other. Wear your mask, social distance, stay home if you are ill andget your flu shot!! We are in this together.UnityPoint Health – Fort DodgeMarketing and Public Relations802 Kenyon Road Fort Dodge, IA 50501(515) 574-6517unitypoint.org/fortdodgeLeah Glasgo, President & Chief Executive OfficerUnityPoint Health – Fort Dodge001678a-10 10/20 CS
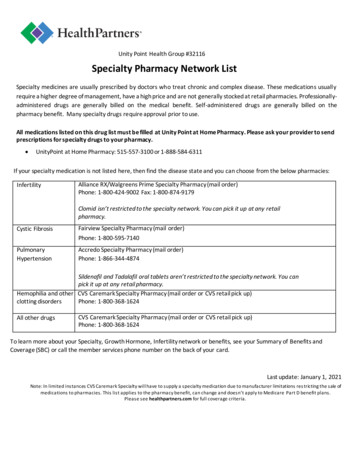
UnityPoint Health Proudly Welcomes Our Newest PhysiciansPrashantha Anand, MDSteven Stokesbary, MDCNOS/UnityPoint Clinic OrthopedicsDr. Anand received his medical degree at Government Medical Collegein India. He completed his residency at B.J. Medical College in Indiaand a fellowship at Duke University Medical Center in Durham, N.C.and Medstar Union Memorial Hospital in Baltimore, M.D. Dr. Anand isBoard Certified by the American Board of Clinical Orthopedic Surgery.CNOS/UnityPoint Clinic OrthopedicsDr. Stokesbary received his medical degree at University of IowaHospitals & Clinics. He completed his residency at the Universityof Missouri - School of Medicine and completed a fellowship atUniversity of Minnesota. Dr. Stokesbary is Board Certified by theAmerican Board of Orthopaedic Surgery.Travis Brownell, MDAlan Stone, MDTrinity Emergency DepartmentDr. Brownell received his medical degree at University of Iowa CarverCollege of Medicine. He completed his residency and a fellowship atthe University of Iowa. Dr. Brownell is Board Certified by the AmericanBoard of Emergency Medicine.Iowa RadiologyDr. Stone received his medical degree at Uniformed ServicesUniversity of the Health Sciences in Maryland. He is Board Certified inDiagnostic Radiology by the American Board of Radiology.Alex Cathey, MDEricha Worple, DOTrinity Hospital Medicine Medical DirectorDr. Cathey received his medical degree at University of North DakotaSchool of Medicine. He completed his residency in Internal Medicineat the University of Iowa in Des Moines. Dr. Cathey is Board Certifiedby the American Board of Internal Medicine.UnityPoint Clinic SurgeryDr. Worple received her medical degree at Des Moines University inIowa. She completed her residency with Geisinger Health System,P.A. Dr. Worple is Board Eligible for American Board of Surgery andAmerican Osteopathic Board of Surgery.-CMohit Chawla, MDIowa Heart CenterDr. Chawla received his medical degree at Indiana University Schoolof Medicine. He also completed his residency at Indiana UniversityMedical Center and a fellowship at Washington University and BarnesJewish Hospital in Missouri. Dr. Chawla is Board Certificated by theAmerican Board of Internal Medicine in Cardiovascular Disease andClinical Cardiac Electrophysiology.Welcome new providers toUnityPoint Health – Fort DodgeSabrina Martinez, MDUnityPoint Clinic Family Medicine - Buena Vista in Storm LakeDr. Martinez received her medical degree at University of WisconsinSchool of Medicine and Public Health. She completed her residencyat UnityPoint Health - Iowa Lutheran Hospital.Benjamin Paul, DOAlexAdam, ARNPUnityPoint ClinicPediatricsTonia Berry, ARNPUnityPoint ClinicFamily MedicineLake ViewAndrewDoster, CRNATrinity AnesthesiaErikaHarwood, ARNPUnityPoint Health atWork - Prestage &Float PoolAddieHinson, ARNPTrinity EmergencyDepartmentNicole Lee, ARNPUnityPoint ClinicFloat PoolJudyNelson, ARNPUnityPoint ClinicOccupationalMedicineErinPeterson, ARNPTrinity EmergencyDepartmentDelaneySchara, PA-CUnityPoint ClinicDermatologyDarleneTurner, ARNPUnityPoint ClinicPalliative MedicineUnityPoint Clinic Family Medicine - HumboldtDr. Paul received his medical degree at A.T. Still University inMissouri. He completed his residency at University of Minnesota inMankato. Dr. Paul is Board Certified through the American Board ofFamily Physicians.Sreenath Kodali, MDTrinity Cancer CenterDr. Kodali received his medical degree at Guntur Medical College inIndia. He completed his residency at Nassau University Medical Centerin New York and a fellowship at Stony Brook University in New York. Dr.Kodali is Board Certified by the American Board of Internal Medicineand Infectious Diseases Board Certified.Sumit Sehgal, MDIowa Heart CenterDr. Sehgal received his medical degree at Ross University School ofMedicine in Dominica. He completed his residency at University ofNevada School of Medicine in Nevada and a fellowship at Universityof Nevada Las Vegas School of Medicine in Nevada. Dr. Sehgal isBoard Certified in Electrocardiography, Nuclear Cardiology, Cardiac CT, and PeripheralVascular Ultrasound.Pacesetter Fall 2020 3
Celebrating Our EmployeesAt UnityPoint Health – Fort Dodge, we know it is our employees that are making a difference everyday in the lives of ourpatients and their families. We celebrate the following employee anniversaries from January through December.Employees With 25 Years of Service40 YearsToni JacksonKaren MarshSherry MolanderBrenda Thoma35 YearsDiane O'Connor30 YearsKaye BeckerJulie DreherCarolyn ElsberryJulie EwingBarbara McneilJulie MeulerKathy Moe25 YearsAlison BirkeySharon LandwehrChrista MartinJulie StumpfLawrence ThompsonTheresa Webster20 YearsJulie AndrewsBrian CerveneSheryl CloughNichole FeickertJulie FranklJolene HalliganDena HofbauerJennifer KolaciaCatherine LenschEmily MartinTrish MooreLori Strand15 YearsRoxanne AmhofCarol ArcherJessica BaileyAmber BarkhausMegan BluntLeah EslickTara EvansSuzanne FallonJeralyn FowlerJames GlassellCorey GleasonEric HageSadie HildrethJay HonomichlCarla LentschAndrea LewisEmily LynnSarah MarshMegan MasonAmber MickelsonMonica RadkeDoris TaetsTriny WallerDiane Walstrom4 UnityPoint Health – Fort Dodge unitypoint.org10 YearsMelissa AndersonDavid CallahanCarolyn GessnerAmy GocheeBrian MundtWanda NaslundKatelyn NehringTracy RichardsonGary SnookJan Westling5 YearsMiranda AndersenWhitney AndersenJames AugustineAnita Ayala-LindnerSamantha BaardsonLaura BalchNicole BartonAmber BeckerJill BontragerCurtis BowmanScott BuffingtonKaty BunstonHailey BuschTonya ButtzGina CarzoliJoy CharlsonTinahti ClarkAmanda ClowAmanda CrouseGale FisherKayla FrancisCaryl FuossTamara GieberAshley GreenKaren GroveKathy HauckTina HendricksonMegan Hicks5 Years (cont.)Ann JagelsKelsie JergensShelley JohansenClaire KingAndrea KrogTara LagerLaura LansingMakinzie LarsonAmanda LyonKylie MaurerDoris McburneyBarbara MeinersCheyenne MillerTina ObergCarolyn OlsonErin OlsonTiffany PhillipsMolly PipalRonald PoldervaartJodi ReekersKayla RittsJerry RobinsonJennifer RoeAntoinette SchoonoverDena SheffieldHeather ShowersKayli StumpfJennifer TelschawAmanda ThummaErica TrustyCindy WeflenTamara WilliamsSarah WrightElizabeth Wygle
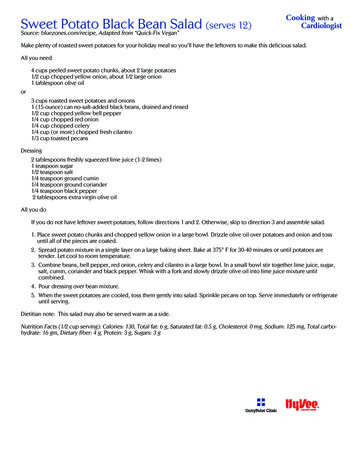
EMPLOYEE SPOTLIGHTCarolyn Elsberry, RN, SurgeryMeet Carolyn Elsberry, RNFor 30 years, Carolyn Elsberry has been a part of the Trinityteam. She began her career in Patient Registration and aftera couple years moved to an administrative assistant in thesurgical unit. It was here that co-workers encouraged her togo back to school.“I wanted to better myself,” shares Carolyn. “There was anurse shortage at the time and the surgical nurses all kepttelling me I should go back to school to be a nurse.”“Being part of that unit, I witnessed how nurses interactedwith their patients and the difference they were making. Itmade me realize I wanted a different career path that wasmore hands on with people. I could see their importancewith helping patients with their healthcare decisions – and Iwanted to be a part of that kind of care.”Through the LINC program (Ladders in Nursing Careers),Carolyn was able to continue to work at Trinity while she wentto school and raise three small children.In 1998, Carolyn changed her badge title to RN and workedfor three years in Acute Care until becoming a surgical nurse.“At the time I completed school there weren’t any openingsin surgery, but I will never regret the experience I hadworking on the patient floor. I believe it helped me be a morewell rounded nurse to be a part of the patients' care on thatside of surgery.”Carolyn shares the best part of being a nurse is having theopportunity to be part of their healthcare team and making adifference in their care. She loves the challenges of workingin the OR, stating, “With all the versatility of specialties thatpractice here, every day is different and every day you learnsomething new.”She also continues to appreciate the support her teamprovides, “My co-workers are more than co-workers. We aremore like family. Everyone is there when you need them andalways step up during difficult times.”“Those were interesting days,” admits Carolyn. It wasthe support and encouragement of her co-workers that kepther going.Pacesetter Fall 2020 5
Valerie Mcsherry, RNIt’s a virus, it’s scary,but we have to do whatwe have to do to takecare of these people.6 UnityPoint Health – Fort Dodge unitypoint.org
Laccey Crimmins, BSN, RNHeidi Lennon with fellow nurses on Acute Care, Whitney Andersen and Shelby BartlettNursing During COVIDA few years from now, students entering the healthcare world will look back and study how our worlddealt with the COVID-19 global pandemic. By then,hopefully, we will know most of the unknowns we are stilldealing with today; the science, what we got right, whatwe miscalculated, and what we learned. There will bemedical journals and scientific explorations of the virus,but what these records may not capture is the courageand teamwork of millions of health care workers andhow they poured themselves into caring for the criticallyill during one of the scariest times of our generation.“When COVID first came out and got to the U.S., I wasterrified. Lots of anxiety, lots of the unknown. Whowas going to take care of all these patients? Who wasgoing to help with all this stuff? And how fast it wasdeveloping,” shares Valerie (Val) Mcsherry, RN, a 15-yearveteran with UnityPoint Health – Trinity Regional MedicalCenter. Her concerns were valid. However, Val alsostates, “It’s a virus, it’s scary, but we have to do what wehave to do to take care of these people.”When COVID-19 started to hit the news in early 2020,initially it seemed to be a crazy thing just happeningChina. But then it began to spread through Europeand soon it hit the west coast of the United States, andthen this scary life-threatening virus became real. Tomake matters worse, the media was all over the placewith information from a man-made deadly virus withintentional spread to just another influenza virus beinghyped-up by the press. Regardless, we knew one thing –COVID-19 was in the U.S. and more than likely, we wouldsee it.I knew I would care for them atsome point. I was nervous aboutit, but I know these people needcare too, just like anybody else.“At first I was thinking, I don't know really what to thinkof it because I haven't dealt with it,” states LacceyCrimmins, BSN, RN, and working on her masters to bea nurse practitioner. “After talking with family workingin New York and Washington state, I kind of was like,'Gosh!' They were telling me, 'We just can't keep up.We can't keep up. People are really sick.' Then you startseeing the CDC and doctors and news coverage andthey're saying the same thing. And I'm like, 'This is bad.Hopefully it doesn't come here because we're rural,we're not nine million people in Iowa, we're three millionpeople.' So, when they started canceling school anddoing all of that stuff around here, I knew this is serious.”Most health care workers in middle America werePacesetter Fall 2020 7
experiencing the same concerns, including Trinity’sHeidi Lennon, Acute Care, RN, states, “I knew I wouldcare for them at some point. I was nervous about it, but Iknow these people need care too, just like anybody else.I'm not going to say, ‘No, I can't do that,’ just becauseof what they have. That's not me. I'm going to take careof them regardless.” And that’s how our nurses anddoctors faced it – head on.So how do you prepare for the unknown? From newsreports across the ocean, the virus spread easily andrapidly with no known cure. Unfortunately, one ‘known’would stand out to the United States, gross amounts ofpersonal protective equipment (PPE) was a must to keepcaregivers safe and the majority of our supplies camefrom China.In order to compensate for the possible shortageof PPE, as well as what types of PPE offered the bestprotection for frontline staff, leading scientists within theCDC, WHO, as well as state and local healthcare officialswere constantly evaluating and analyzing data aboutthe virus and providing recommendations. As fast as thevirus moved, so did the guidelines.“It seemed like things were changing on a daily orsometimes hourly basis of what precautions weneeded to take, what we were watching for, what wewere screening for,” explains Diane Walstrom, RN, withTrinity for 13 years. “Our manager would meet with ussometimes several times a day just to update everyoneon what was going on and the changes, making surethat we all had our PPE.” The team would also get countsof how many gowns, gloves and masks they had onhand. Which Diane admits, prior to COVID-19 they hadall taken for granted always having enough PPE and nowthey were much more aware of the needto conserve.I feel like we werevery well prepared.The rapidly changing environment seemed like awhirlwind for the healthcare industry, the benefit ofliving in rural America, we were allowed time to prepareas best we could before any positive patients enteredour facility. As Diane shares, “I feel like we were verywell prepared. Much more than on the coast because8 Mcsherry,UnityPointRNHealth – Fort Dodge unitypoint.orgValeriewe had all this extra time to talk about it, and plan forit, and train. We had time to make sure that we wereputting our gowns on correctly and taking our gownsoff correctly and touching things correctly so that weweren't spreading things to other people.”Even though it wasn't until early March that ourcommunity officially started to close business doors andsending people home to work, our health care team inpartnership with Public Health officials, had the foresightto start planning for a possible pandemic all the wayback into late January. This gift of time helped our keyteam players to become familiar with evolving guidanceand resources necessary to care for patients suspectedor positive for COVID-19. It also allowed staff to practice,plan, and talk through management of patients. Whenthe first patient was admitted, our team was able tosafely care for that patient because of the planning andtraining done with frontline staff.They're just like any otherpatient. They need care, andonce you get in there and youstart taking care of them, allthose feelings disappear.While all training beforehand made our team wellprepared, nothing can ever replace actual experience.“I put my PAPR on and made sure I had everythingconnected and gowned up, garbed up,” states HeidiLennon. “When I started walking down the hall, I got alittle nervous. I could kind of feel my anxiety rise a littlebit and started sweating. But I mean, they're just like anyother patient. They need care, and once you get in thereand you start taking care of them, all those feelingsdisappear. You're not worried about that anymore. Youhave your appropriate gear on. You know you have whatyou need. Just take care of your patients, just like youwould any other patient.”“The first time I went in the room, I guess I was justdouble checking to make sure my gear was on rightand I was sealed, my mask was sealed,” states LacceyCrimmins sharing the same emotions, “I had my eyeshield and my two pairs of gloves and walking in there I didn't feel bad for myself, I felt bad for the patient.Especially when none of the patients can see what
Diane Walstrom, RNyou're saying. It's hard to hear. It's a barrier on top ofbeing sick and not feeling good. So, I felt worse for mypatient than I did for myself,” she continues, “I reallydidn't think about, I wasn't really scared like, ‘I'm goingto get it!’ I just kept thinking, ‘I hope my patient can hearme okay. I hope they can understand what I'm saying.’I guess I was worried more about that than the virus atthe time. And maybe it was me distracting myself, but Ifelt safe. I felt like I had all the gear I needed, and I wasprotected.”Diane also shared about the morning of her firstexperience, “I had actually known prior to coming towork that day that I was probably going to be takingcare of a COVID positive patient. I received a messagetelling me what department to work in, and I knew thatif that department was open, that meant I was probablygoing to have a positive patient. I remember leavingfor work that day being a little more apprehensive thanwhat I normally am. We had possible patients, but noone actually positive. And I was just so nervous for mypatient. We're being told that these people are verysick, that they can decline and become much sicker veryquickly. So, how sick is this patient going to be? Whatam I going to have to do? And then that extra concernof knowing what am I doing, am I using my proper PPE?How protective am I? Which I'm always conscious ofthat, but not to this extent.”I do remember just spendinga little extra time with thekids that morning.She continues, “I will say, I did stop and hug my kidsa little longer that day and give them a couple extrakisses. Because I know what we hear in healthcare, andthe percentage of nurses and doctors that are gettingPacesetter Fall 2020 9
this and hospitalized with this. I do remember justspending a little extra time with the kids that morning,just thinking if something should happen, I may be faraway for a few weeks.”Just like many frontline team members, Val stayed awayfrom family members to keep them safe, “I haven'tspent time with my family since the beginning of Marchbecause I have an unhealthy mother and I have a littlebaby niece. So, it's sad. But I know that staying awayfrom them as much as I can is the right thing to do.”But it wasn’t just their own personal struggles dealingwith the virus and keeping their families safe as theycared for COVID patients. Frontline staff would soonfind themselves replacing the family members of theirpatients when all visitors were restricted for all patients.“With patients not being able to have family visit, you tryto be more like a family member to them,” states Heidi.“You stay with them longer. You talk with them more.You make sure they're comfortable, have what theyneed. Just empathize with them. I mean, this is scaryfor them, and a lot of them are really sick. They declinepretty quickly. So, you just try to be with them as muchas you can and make sure they have what they need.Keep them calm. Try and listen to their fears, listen totheir concerns, and just be there for them.”“Sometimes it's kind of being pulled in multipledirections that we're not used to because we're usedto having family members here to hold their hand andgive them a hug,” further explains Diane. “I also feelsad that they don't have their family members here todo that. I have had my own family that has been in thehospital, and that have been in care centers, I know I'mvery appreciative of the nurses that are there doing whatI want to do. I love that part of it, that I'm able to givethat to my patients. But at the same time, it's probablythe hardest thing that we have to go through is tellingpeople that they can't have their loved ones here or thatthey can't be here with their loved one.”Keeping family members at home in the loop is alsoa crucial part of patient care includes Val, “Your verypatient with the patients and you sit down, and you talk.And with the family members we do the same thing. Youtalk to them on the phone. Some phone conversationscould last a really long time, which is something wewouldn't normally do because we're so busy. But in thistime, we know that we have to take the extra time tomake them feel more comfortable with what's going onat the hospital and that they're in good hands with us.”10 UnityPoint Health – Fort Dodge unitypoint.orgEven though it hasbeen extremelydifficult for bothpatients and familiesnot to be able to betogether, today’stechnology hasalso filled a gap. “Iguess the biggestthing I've done tohelp my patients ishelping them utilizetechnology to connectValerie Mcsherry, RNwith their families.It is really nice having social media, iPads, Zoom, andFaceTime. I feel that if loved ones can see each otherand speak to each other, that's so much more reassuringthan just talking on the phone,” explains Laccey.Although presently, COVID-19 is still very much withus and number of cases are still emerging our teamremains hopeful. Some cases have been intenselydifficult, and some have been extremely gratifying.“One of our patients that recovered from COVID wason the ventilator for at least two weeks,” states Val. “Thepatient was then extubated and was doing pretty well.I went into the room to help get the patient up for thevery first time. The patient smiled at me when I walkedinto the room and I said, ‘Do you remember me?’ Andthe patient shook their head, yes. And I thought, ‘wow’because when people are on the ventilators, you neverexpect them to remember you or remember thingsyou say, because they're either sedated or somewhatsedated. So that was really neat.”All our nurses will agree, being a part of a patient’scare is an honor. It’s also extremely gratifying to watcha patient to go from very sick to getting well, it’s oneof the main reasons they became a nurse. Their hopeis that one day we will no longer be dealing with thispandemic, but until then, Heidi reminds us, “Take care ofyourselves. If you have a cough, don't go out. Wear yourmasks in public. Just be safe.”
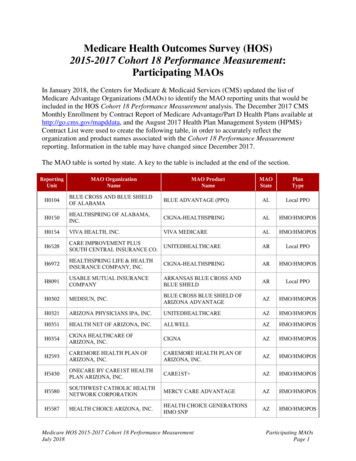
Caring for the HeartEarly this fall we had a surprise visitor at the TrinityEmergency Department, a grateful patient returnedto thank our team for saving their life. The patient hadawakened with chest pain, came in to get checked-outand then proceeded to code in the ER. The patientattributed their life-saving experience to the skills andexpertise of the team. Little did that patient know,they were correct in their assertation of our team,about the same time Trinity was being informed oftwo prestigious recognitions concerning our heartprogram.First, Trinity received the American College ofCardiology’s NCDR Chest Pain – MI Registry PlatinumPerformance Achievement Award for2020. Trinity is one of only 140 hospitals2020nationwide to receive the honor. TheChest Pain – MIaward signifies that Trinity has reached anRegistryaggressive goal of treating these patientsto standard levels of care as outlined bythe American College of Cardiology/American Heart Association clinical guidelines andrecommendations. To receive the Chest Pain – MIRegistry Platinum Performance Achievement Award,Trinity has demonstrated sustained achievement inthe Chest Pain – MI Registry for two consecutive years(2018 and 2019), and performed at the highest levelfor specific performance measures.Then we also learned that Trinity earnedthe Mission: Lifeline Gold Plus ReceivingAchievement Award. This award is achievedby meeting specific criteria and standardsof performance for quick and appropriatetreatment through emergency proceduresto re-establish blood flow to blockedarteries in heart attack patients. The American HeartAssociation’s Mission: Lifeline program’s goal is tolessen system barriers to quick treatment for heartattacks, from the time the 9-1-1 call is placed, to EMStransport and continuing throughout the individual’shospital stay and discharge.As Leah Glasgo, UnityPoint Health – Fort DodgePresident and CEO states, “Trinity is extremelyhonored to be among the nation’s top performinghospitals for caring for heart attack patients. Theseawards recognize our commitment to and successin implementing a higher standard of care for heartattack patients.”For over 20 years, Trinity and Iowa Heart Center haveworked closely together to develop the award-winningheart program. Its takes full teamwork from the FortDoge Fire Department EMS team, to the ER, Cath Laband then the Cardiac Rehab team to ensure each MIpatient receives quality expedient care and the followup rehab and education to help keep patients on theright track.“While being honored among the nation’s topperforming hospitals for caring for heart attacks isvery exciting,” Leah continues, “What really gets usexcited is seeing how we’re affecting lives and keepingcare close to home. It takes seamless coordination toensure each patient gets the appropriate level of careat the right time and place, and we know every secondcounts - especially when it comes to emergencies likeheart attacks. As Dr. Cookman always reminds us,‘Time is muscle,’ and Trinity’s team is providing thatfast high level of care.”Above Left: Trinity's ER plays a key role in ensuring heart attack patients get to the cath lab as quickly as possible. Above Right: Trinity's heart team includes everyone from Iowa Heart, TCVLand Rehab. Everyone's expertise plays a key role in helping heart patients have the best outcome.Pacesetter Fall 2020 11
How are YOU doing?With Jennifer Pullen, LMHC, UnityPoint Health – Berryhill CenterOne day you are feeling fine and good about life,then you watch the news or take a stroll through socialmedia and your heart rate starts to rush with anxiety.That feeling of being ‘ok’ can easily get replaced witha sadness about life and our world. The one thing youneed to know, you are not alone in feeling this way.“COVID burn out - it’s real and it is affecting everyoneon some level,” states Jennifer Pullen, LMHC, ClinicalManager, Berryhill Center. What was to be a two week‘flattening of the curve’ has turned into months ofuncertainty around everything we call normal. Thatuncertainty is causing stress, and anxiety for eventhe most even keeled people. According to a studyperformed in June by the CDC, over 40% of thosesurveyed said they had experienced a mental orbehavioral health condition related to the coronavirusepidemic.While none of us wants this current state to be our newnormal, somehow, at least for a while longer, we need tofind a way to be okay with this new normal.“Dealing with all that we have over the past few monthsis a lot like dealing with grief,” explains Jennifer. “The fivestages of grief are denial, anger, bargaining, depressionand then acceptance. I know I can look back personallyand see many of these emotions I’ve been dealing with inmy own personal life. When some of our health experts12 UnityPoint Health – Fort Dodge unitypoint.orgsuggested early in March that we would still be dealingwith COVID in the fall, I was totally in denial. I was angrywhen I couldn’t spend Easter with my extended family asI always have. I was depressed when I watched my ownchildren suffering because they couldn’t be with theirfriends. As much I as want this all to be over, I know thatfor my own mental health and for that of my family's, Ineed to accept the current status quo and do what I canmake the best of it and find new ways of doing
Prashantha Anand, MD CNOS/UnityPoint Clinic Orthopedics . David Callahan Carolyn Gessner Amy Gochee Brian Mundt Wanda Naslund Katelyn Nehring Tracy Richardson Gary Snook Jan Westling . Tamara Gieber Ashley Green Karen Grove Kathy Hauc