Transcription
CHAPTER 2Medicaid Coverageof Dental Benefitsfor Adults
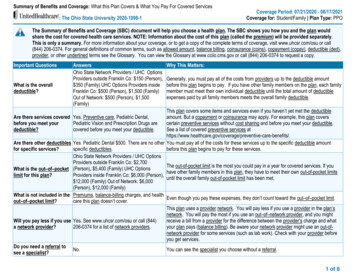
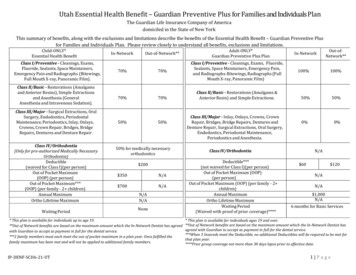
Chapter 2: Medicaid Coverage of Dental Benefits for AdultsMedicaid Coverage of Dental Benefits for AdultsKey Points Poor oral health is widespread among adults in the United States and especially affectsthose with low incomes.–– Adults with incomes below 100 percent of the federal poverty level (FPL) are three timesmore likely to have untreated dental caries—commonly known as cavities—than adultswith incomes above 400 percent FPL.–– Thirty-seven percent of adults age 65 and older with incomes below 100 percent FPLhad complete tooth loss compared to 16 percent of those with incomes at or above 200percent FPL. Individuals with a range of chronic conditions are more susceptible to oral disease.Oral disease can also exacerbate chronic disease symptoms. Poor oral health can limitcommunication, social interaction, and employability.Medicaid programs are required to cover dental services for children and youth under age21 but there are no minimum coverage requirements for adults. As a result, adult dentalbenefits vary widely across states. For example, as of February 2015:–– 19 states provided emergency-onlyadult dental benefits for non-pregnant,non-disabled adults;–– 27 states covered preventive services;–– 26 states covered restorative services;–– 19 states covered periodontal services; –– 25 states covered dentures;–– 25 states covered oral surgery;–– 2 states covered orthodontia; and–– 9 states placed an annual dollar limiton covered dental services.States change Medicaid coverage of adult dental benefits on a regular basis, cutting benefitswhen budgets are tight and expanding them when more funds are available.Initiatives to improve access to dental services include using mobile clinics and telehealthtechnologies, increasing the number of providers serving Medicaid enrollees, and fundingdemonstrations to encourage Medicaid enrollees to increase dental utilization. For example:–– In 2014, the Health Resources and Services Administration supported 238 school-basedhealth center oral health activities through capital grants.–– The National Health Service Corps and some states offer student loan repaymentassistance to dentists who commit to working in high-need, underserved, or rural areas.–– Minnesota and Alaska have amended state scope-of-practice laws to allow mid-leveldental practitioners to provide dental services.24June 2015
Chapter 2: Medicaid Coverage of Dental Benefits for AdultsCHAPTER 2:Medicaid Coverageof Dental Benefitsfor AdultsFederal law does not mandate any minimumrequirements for adult dental coverage underMedicaid, allowing states to decide whetheror not to provide such coverage. As with otheroptional Medicaid benefits for adults, statesthat cover dental services under Medicaid candefine the amount, duration, and scope of theservices covered. States often reduce or eliminateadult dental benefits in response to budgetdifficulties, and may restore benefits when thestate budget outlook improves (Lee et al. 2012,Gehshan et al. 2001). In contrast, the Early andPeriodic Screening, Diagnostic, and Treatment(EPSDT) benefit for children under age 21 enrolledin Medicaid, and the State Children’s HealthInsurance Program (CHIP) require states toprovide comprehensive dental services necessaryto prevent disease and promote oral health, restoreoral structures to health and function, and treatemergency conditions without caps or other limitsthat are unrelated to medical necessity (Cardwellet al. 2014, Kaiser 2012a).1This chapter examines dental benefits for adultsenrolled in Medicaid. We begin by examiningwhy oral health benefits are important for alladults, and particularly those with low incomes.We describe current Medicaid dental benefitsfor adults, noting differences for varioussubpopulations, and report on recent changes instate coverage policies. We present informationon the use of dental care by Medicaid enrollees aswell as state and community efforts to improveaccess to care in underserved areas.Report to Congress on Medicaid and CHIPThe Impact of PoorOral HealthPoor oral health affects a majority of adults inthe United States. Almost all (92 percent) adultsage 20 to 64 have had dental caries, commonlyreferred to as cavities, in their permanent teeth(NIDCR 2015). Of those with dental caries, adultswith incomes below 100 percent of the federalpoverty level (FPL) are more than three times aslikely to have untreated dental caries than adultswith incomes above 400 percent FPL (Kaiser2012b). Specifically, between 2005 and 2008, 42percent of adults age 20 to 64 with incomes below100 percent FPL had untreated dental caries,compared to 11 percent of those with incomesabove 400 percent FPL. Additionally, among adultsage 65 and older with incomes below 100 percentFPL, 37 percent were edentulous (meaning theyhad complete tooth loss), compared to just 16percent of those with incomes at or above 200percent FPL (Dye et al. 2012).Disparities also exist within racial and ethnicgroups and for older adults. Among adults age20 to 64 with incomes below 100 percent FPL,almost 53 percent of African American adults haduntreated dental caries, compared to 40 percentof non-Hispanic white adults in that incomerange (NCHS 2013). Additionally, 32 percent ofnon-Hispanic black adults age 65 and over wereedentulous, compared to 22 percent of nonHispanic white adults (Dye et al. 2012).Individuals with a range of chronic conditionsare more susceptible to oral disease, and in turn,oral disease can contribute to complicationsfrom these conditions and exacerbate theirsymptoms. Diseases of poor oral health includethe gum disease gingivitis and the gum infectionperiodontitis, which may involve all of the softtissue and bone supporting the teeth (Kaiser2012b). People with uncontrolled diabetesare more susceptible than their non-diabeticcounterparts to develop periodontal diseases,25
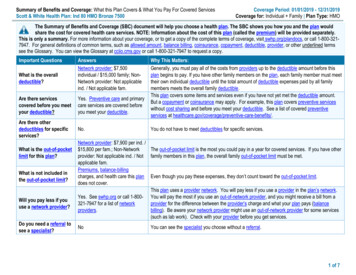
Chapter 2: Medicaid Coverage of Dental Benefits for Adultswhich can, in turn, adversely affect metaboliccontrol of diabetes (Nycz 2014, Kuo et al. 2008,Mealey 2006). Individuals with respiratoryinfections, such as pneumonia and exacerbatedchronic obstructive pulmonary disease, are morelikely than those without such infections to havepoor periodontal health, gingival inflammation, anddeeper pockets (deep spaces between the teethand gum tissue that provide a place for bacteriato live) (Kuo et al. 2008, Sharma and Shamsuddin2011). There is also evidence of a link betweenosteoporosis and tooth loss, although the causalrelationship is unclear (Inaba and Amano 2010,Kuo et al. 2008).have negative cosmetic consequences affecting aperson’s ability to communicate and limiting socialinteractions (USPHS 2000).Periodontal disease may also affect pregnancyoutcomes. There is an emerging consensusthat preventive dental care during pregnancy isdesirable (Boggess et al. 2013, Albert et al. 2011,Detman et al. 2010, Offenbacher et al. 2006). Somestudies show an association between maternalperiodontal disease and pregnancy complications,such as preterm labor or premature rupture ofmembranes, both major precursors to pretermbirths (Offenbacher et al. 2006, USPHS 2000).Research shows a possible association betweenpreterm birth, low birth weight, and poor oralhealth (Albert et al. 2011, Skelton et al. 2009).In 2014, 55 percent of firms in the United Statesoffered health benefits to their employees. Healthcoverage may be provided as part of a broaderplan that includes medical benefits or stand-alonecoverage (GAO 2010). Slightly more than half (53percent) of firms offering health benefits to theiremployees offer or contribute to a dental coveragebenefit for their employees that is separate fromany dental coverage the health plan may include.Firms with 200 or more employees are morelikely to offer or contribute to a separate dentalhealth benefit than smaller firms—88 percent and52 percent, respectively (Claxton et al. 2014).The specific dental benefits covered vary acrosssponsoring employers and plans.In addition to its association with serious medicalconditions, poor oral health can negatively affectindividuals in other ways. Untreated dentalconditions can lead to pain and tooth loss,jeopardizing employment and lowering qualityof life. For example, in fiscal year 2008, 52.5percent of U.S. Army recruits were classified asDental Fitness Classification 3, meaning thatthey were non-deployable without treatment forurgent conditions that likely would cause a dentalemergency within 12 months (Moss 2011). Sucha classification prohibits U.S. Army recruits fromserving in combat until their dental needs areaddressed. Pain affects everyday activities suchas speech, eating, and sleep, which may detersocialization and employment (Dubay et al. 2005,Kaiser 2012b). In addition, poor oral health can26Public and Private Coverageof Dental ServicesAccess to and use of dental care increases whena person has dental insurance benefits (Manskiet al. 2002). Dental benefits vary widely amongprivate and public payers, from comprehensive toemergency care only.Adult dental services are not included in the 10essential health benefits established in the PatientProtection and Affordable Care Act (ACA, P.L. 111148, as amended) that must be offered in healthplans in the individual and small group markets,whether inside or outside of the health insuranceexchanges. Consequently, adults purchasing anindividual plan or purchasing a small group planare not guaranteed dental coverage unless theyenroll in a stand-alone dental plan.Medicare provides limited dental benefits, payingonly for dental services that are an integral partof either a covered procedure or a procedure doneJune 2015
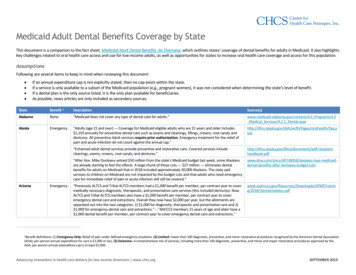
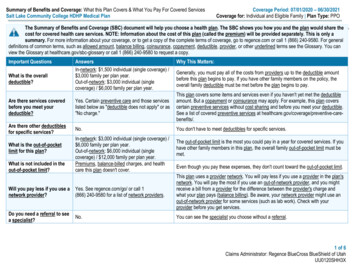
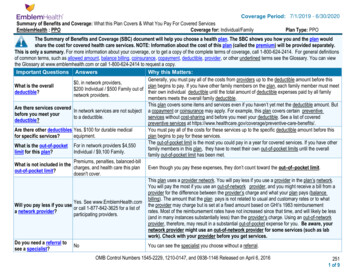
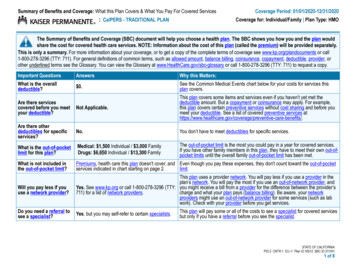
Chapter 2: Medicaid Coverage of Dental Benefits for Adultsin preparation for other covered treatment, forexample: reconstruction of the jaw followingaccidental injury;extractions done in preparation for radiationtreatment for neoplastic diseases involvingthe jaw;oral examinations, but not treatment,preceding kidney transplantation orheart valve replacement under certaincircumstances; andinpatient hospital services if the severity of adental procedure requires hospitalization inconnection with the provision of services foran underlying medical condition (CMS 2013).According to data from the 2012 MedicaidExpenditure Panel Survey (MEPS), people with lowincomes are less likely to have dental coveragethan those with higher incomes. Seventy-onepercent of those with incomes above 200 percentFPL have some level of coverage, compared to42 percent of those with incomes at or below100 percent FPL. Additionally, people with lowincomes who have dental coverage are more likelyto have public coverage than those with higherincomes. Of adults with incomes at or below100 percent FPL, 26 percent have public coverage,and 16 percent have private coverage. In contrast,2 percent of people with incomes above200 percent FPL have public coverage, while69 percent have private coverage (Rohde 2014).As discussed later in this chapter, coverage ishighly associated with use of services.Adult Dental Benefitsin MedicaidMedicaid programs vary in the dental servicesthey cover for adults (Table 2-1). Currently, 18states cover emergency services only. StatesReport to Congress on Medicaid and CHIPthat cover emergency services differ in how theydefine those services, although most includeemergency coverage of treatment for pain andinfection. Thirty-three states cover services beyondemergency services, but many impose annualdollar and service limits. These limits vary widelyamong states. Twenty-eight states cover preventiveservices such as oral examinations, teeth cleanings,fluoride application, and sealant application(painting a plastic material on to the chewingsurfaces of the back teeth to prevent decay).Many of the 26 states offering restorative servicesplace annual limits on the number of fillings orcrowns an enrollee can get, the types of crownsthat can be used on certain teeth, and how oftenroot canals can be performed. Most states thatcover oral surgery services include extractions,and some include jaw repair, removal of impactedteeth, or other surgical services. Most statescovering denture services offer replacementdentures every 5 to 10 years, but some offer onlyone set of dentures per lifetime.Many states place limits on the dental servicesthey will cover within a certain time frame. Ninestates have annual dollar limits, ranging from 500 to 2,500 a year (Table 2-2). Additionally,31 states place limits on the frequency of servicedelivery. As do many commercial dental benefitproviders, state Medicaid programs commonlylimit examinations and cleanings to one or twoper year. Connecticut and Illinois limit fillings toone per year, limit crowns to one per tooth everyfive years, and limit root canals to one per toothper lifetime. North Dakota, Rhode Island, andWashington limit root canals to front teeth only.Prior authorization is also commonly requiredfor many services, although not for emergencyservices. Detailed information on state coverageand limits can be found in Appendix 2A, Tables2A-1 and 2A-2.Some states have different Medicaid dentalcoverage policies for pregnant women and certaindisabled adults, sometimes using Section 1115demonstration waivers to cover dental services27
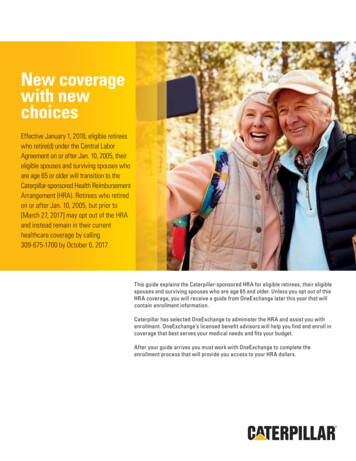
Chapter 2: Medicaid Coverage of Dental Benefits for AdultsTABLE 2-1. T ypes of Adult Dental Services Covered for Non-Pregnant, Non-Disabled Adults underMedicaid, 2015Type of serviceNumber ofstatesEmergency only18More extensive33Services typically includedEmergency extractions, other procedures for immediate pain reliefPreventive28Examinations, cleanings, and sometimes fluoride application or sealantsRestorative26Fillings, crowns, endodontic (root canal) therapyPeriodontal19Periodontal surgery, scaling, root planing (cleaning below the gum line)Dentures26Full and partial denturesOral surgery25Non-emergency extractions, other oral surgical proceduresOrthodontia2Braces, headgear, retainersNote: Federal Medicaid regulations define dental services as “diagnostic, preventive, or corrective procedures provided by or under thesupervision of a dentist in the practice of his profession, including the treatment of – (1) the teeth and associated structures of the oralcavity; and (2) disease, injury, or impairment that may affect the oral or general health of the recipient.” (42 CFR 440.100).Sources: MACPAC analysis of AHCCCS 2014, Alaska DHHS 2014, Amerigroup 2014, Anthem Blue Cross and Blue Shield 2014, BadgerCarePlus and Wisconsin Medicaid 2015, BadgerCare Plus and Wisconsin Medicaid 2013, Better Health Florida 2014, California Medi-CalDental Program 2015, Colorado DHCPF 2014, Commonwealth of Virginia DMAS 2012, Connecticut Dental Health Partnership 2013,DentaQuest of Illinois, LLC. 2014, DentaQuest, South Carolina Healthy Connections 2014, Florida AHCA 2011, Hawaii State Med-QuestDivision 2011, Holleman 2014, Idaho DHF 2015, Illinois DHFS 2014, Indiana Dental Association 2011, Indiana FSS 2014, Iowa DHS 2013,KanCare 2015, Kansas DHE 2015, 907 Ky. Admin. Regs. 1:026 (2012), Kentucky CHFS 2013, Maine Department of Health and HumanServices 2014, Maryland DHMH 2015, Maryland DHMH 2007, Massachusetts EOHHS 2014, 130 Mass. Code Regs. 420 (2014), MDWise2014, Michigan DCH 2014, Minnesota DHS 2014, Miss. Admin. Code 23-204:1 (2015), Missouri DSS 2013, MOHealthNet 2013, MontanaDPHHS 2015, Montana DPHHS 2013a, Montana DPHHS 2013b, Nebraska DHHS 2008, Nevada DHHS 2010, New Hampshire MedicaidProgram 2013, N.J. Admin. Code § 10:56-2.6 (2015), N.M. Admin. Code § 8.310.2.12(G) (2015), New York State Medicaid Program 2013,North Carolina DMA 2013, North Dakota DHS 2013, Ohio Department of Medicaid 2015, Okla. Admin. Code § 317:30-5-696 (2014), Or.Admin. R. 410-123 (2014), Oregon Health Plan 2012, Oregon Medicaid 2014, Peach State Health Plan 2013, Pa. Code § 55:1149.24(2015), Pennsylvania DPW 2014a, Pennsylvania DPW 2014b, Rhode Island DHS 2010, South Carolina Healthy Connections Choices 2015,South Dakota DSS 2015, South Dakota DSS 2015, State of Louisiana BHSF 2012, State of Louisiana DHH 2015, State of Missouri 2013,Texas HHSC 2015, Utah DMHF 2014, Vermont AHS 2014, Washington AppleHealth 2014, WellCare 2014, West Virginia BMS 2015, WestVirginia DHHR 2012, Wyoming Department of Health 2015, Xerox 2014. See Appendix 2A for additional details.for these populations (Silverman 2012). TheConsolidated Omnibus Budget Reconciliation Actof 1985 (COBRA, P.L. 99-272) granted states theoption of providing an enhanced benefit packageto pregnant women, and approximately half ofthe states use this authority to provide dentalbenefits (Johnson and Witgert 2010). Adults withdisabilities, who are more likely to have dentaldisease than non-disabled people, also receiveMedicaid dental benefits beyond their non-disabledcounterparts in some states (Waldman andPerlman 2012, McGinn-Shapiro 2008).28Adult dental benefits in Medicaid also vary instates that expanded adult Medicaid eligibilityunder the ACA. States that have chosen atraditional expansion, as laid out in the ACA, mustcreate an alternative benefit plan for their Medicaidexpansion population, which may be different fromwhat the base population receives (Chazin et al.2014, CMS 2014a). For example, North Dakota’salternative benefit plan limits dental coverage forthe Medicaid expansion population to emergencyonly coverage, while it provides additional dentalbenefits for non-expansion enrollees (CMS 2014b).States that choose to expand Medicaid using aJune 2015
Chapter 2: Medicaid Coverage of Dental Benefits for AdultsTABLE 2-2. M edicaid Dental Benefits for Non-Pregnant, Non-Disabled Adults by State, as ofFebruary 2015Dental services coveredStateTotalAlabamaEmergencyservices Preventive Restorative 8261926LimitsAnnual orAnnuallifetimeOralspendinglimits onsurgerylimitsservicesservices Orthodontia (dollars)2529311Alaska( 1,150)ArizonaArkansas( 500)California( 1,800)Colorado( 1,000)ConnecticutDelawareYesYesYesYes1District sissippiYes( 2,500)MissouriMontanaNebraskaNevada( 1,000)YesYesNew HampshireNew JerseyNew MexicoYesNew YorkYesNorth CarolinaYesNorth DakotaYesReport to Congress on Medicaid and CHIPYes29
Chapter 2: Medicaid Coverage of Dental Benefits for AdultsTABLE 2-2. (continued)Dental services coveredStateEmergencyservices Preventive Restorative itsAnnual orAnnuallifetimeOralspendinglimits onsurgerylimitsservicesservices Orthodontia ode IslandYesSouth CarolinaYes( 750)South DakotaTennessee( 1,000)2TexasUtahVermont( 510)YesVirginiaYesWashingtonYesWest VirginiaWisconsinWyomingYesYesNotes:1Alabama and Delaware classify themselves as offering no dental services, including no emergency services. However, emergencyservices related to oral health care may be covered under another benefit type. Alabama states that dental services are “any diagnostic,preventive, or corrective procedures administered by or under the direct supervision of a licensed dentist. Such services includetreatment of the teeth and the associated structures of the oral cavity, and of disease, injury, or impairment, which may affect the oralor general health of the individuals” (Alabama Medicaid 2015). Delaware states that dental services include “any services related to thedental treatment such as drugs, anesthetics, and use of operating/recovery room, etc.” (DHSS 2014).Tennessee covers emergency dental treatment only when “an adult enrollee presents to a hospital emergency department with adental problem,” in which case screening and treatment of the emergency medical condition identified in the screening are covered.Tennessee does not cover services to treat the origin of the emergency medical condition and does not cover any emergency services inany setting beyond the emergency department (TennCare 2014).2Sources: MACPAC analysis of AHCCCS 2014, Alaska DHHS 2014, Amerigroup 2014, Anthem Blue Cross and Blue Shield 2014, BadgerCarePlus and Wisconsin Medicaid 2015, BadgerCare Plus and Wisconsin Medicaid 2013, Better Health Florida 2014, California Medi-CalDental Program 2015, Colorado DHCPF 2014, Commonwealth of Virginia DMAS 2012, Connecticut Dental Health Partnership 2013,DentaQuest of Illinois, LLC. 2014, DentaQuest, South Carolina Healthy Connections 2014, Florida AHCA 2011, Hawaii State Med-QuestDivision 2011, Holleman 2014, Idaho DHF 2015, Illinois DHFS 2014, Indiana Dental Association 2011, Indiana FSS 2014, Iowa DHS 2013,KanCare 2015, Kansas DHE 2015, 907 Ky. Admin. Regs. 1:026 (2012), Kentucky CHFS 2013, Maine Department of Health and HumanServices 2014, Maryland DHMH 2015, Maryland DHMH 2007, Massachusetts EOHHS 2014, 130 Mass. Code Regs. 420 (2014), MDWise2014, Michigan DCH 2014, Minnesota DHS 2014, Miss. Admin. Code 23-204:1 (2015), Missouri DSS 2013, MOHealthNet 2013, MontanaDPHHS 2015, Montana DPHHS 2013a, Montana DPHHS 2013b, Nebraska DHHS 2008, Nevada DHHS 2010, New Hampshire MedicaidProgram 2013, N.J. Admin. Code § 10:56-2.6 (2015), N.M. Admin. Code § 8.310.2.12(G) (2015), New York State Medicaid Program 2013,North Carolina DMA 2013, North Dakota DHS 2013, Ohio Department of Medicaid 2015, Okla. Admin. Code § 317:30-5-696 (2014), Or.Admin. R. 410-123 (2014), Oregon Health Plan 2012, Oregon Medicaid 2014, Peach State Health Plan 2013, Pa. Code § 55:1149.24(2015), Pennsylvania DPW 2014a, Pennsylvania DPW 2014b, Rhode Island DHS 2010, South Carolina Healthy Connections Choices 2015,South Dakota DSS 2015, South Dakota DSS 2015, State of Louisiana BHSF 2012, State of Louisiana DHH 2015, State of Missouri 2013,Texas HHSC 2015, Utah DMHF 2014, Vermont AHS 2014, Washington AppleHealth 2014, WellCare 2014, West Virginia BMS 2015, WestVirginia DHHR 2012, Wyoming Department of Health 2015, Xerox 2014. See Appendix 2A for additional details.30June 2015
Chapter 2: Medicaid Coverage of Dental Benefits for AdultsFIGURE 2-1. Medicaid Dental Benefits for Non-Pregnant, Non-Disabled Adults, FLAKHIEmergency services only orno dental services covered (18)1 to 4 services (17)5 or more services (15)Note: Does not reflect differences in dental benefits that may be available to pregnant women, adults with disabilities, adults inthe Medicaid expansion population, or those enrolled in certain Medicaid managed care organizations.Source: MACPAC analysis of AHCCCS 2014, Alaska DHHS 2014, Amerigroup 2014, Anthem Blue Cross and Blue Shield 2014,BadgerCare Plus and Wisconsin Medicaid 2015, BadgerCare Plus and Wisconsin Medicaid 2013, Better Health Florida 2014,California Medi-Cal Dental Program 2015, Colorado DHCPF 2014, Commonwealth of Virginia DMAS 2012, Connecticut DentalHealth Partnership 2013, DentaQuest of Illinois, LLC. 2014, DentaQuest, South Carolina Healthy Connections 2014, Florida AHCA2011, Hawaii State Med-Quest Division 2011, Holleman 2014, Idaho DHF 2015, Illinois DHFS 2014, Indiana Dental Association2011, Indiana FSS 2014, Iowa DHS 2013, KanCare 2015, Kansas DHE 2015, 907 Ky. Admin. Regs. 1:026 (2012), Kentucky CHFS2013, Maine Department of Health and Human Services 2014, Maryland DHMH 2015, Maryland DHMH 2007, MassachusettsEOHHS 2014, 130 Mass. Code Regs. 420 (2014), MDWise 2014, Michigan DCH 2014, Minnesota DHS 2014, Miss. Admin. Code23-204:1 (2015), Missouri DSS 2013, MOHealthNet 2013, Montana DPHHS 2015, Montana DPHHS 2013a, Montana DPHHS2013b, Nebraska DHHS 2008, Nevada DHHS 2010, New Hampshire Medicaid Program 2013, N.J. Admin. Code § 10:56-2.6 (2015),N.M. Admin. Code § 8.310.2.12(G) (2015), New York State Medicaid Program 2013, North Carolina DMA 2013, North Dakota DHS2013, Ohio Department of Medicaid 2015, Okla. Admin. Code § 317:30-5-696 (2014), Or. Admin. R. 410-123 (2014), Oregon HealthPlan 2012, Oregon Medicaid 2014, Peach State Health Plan 2013, Pa. Code § 55:1149.24 (2015), Pennsylvania DPW 2014a,Pennsylvania DPW 2014b, Rhode Island DHS 2010, South Carolina Healthy Connections Choices 2015, South Dakota DSS 2015,South Dakota DSS 2015, State of Louisiana BHSF 2012, State of Louisiana DHH 2015, State of Missouri 2013, Texas HHSC 2015,Utah DMHF 2014, Vermont AHS 2014, Washington AppleHealth 2014, WellCare 2014, West Virginia BMS 2015, West VirginiaDHHR 2012, Wyoming Department of Health 2015, Xerox 2014. See Appendix 2A for additional details.Report to Congress on Medicaid and CHIP31
Chapter 2: Medicaid Coverage of Dental Benefits for Adultsdemonstration waiver can also create differentbenefits for the expansion population. Indianaexpanded Medicaid eligibility through a Section1115 demonstration waiver and opted to provideadditional adult dental benefits to enrollees whomake monthly contributions to a health savingsaccount (CMS 2015). Iowa also expanded througha Section 1115 demonstration waiver and optedto provide three tiers of dental benefits, allowingenrollees to gain access to additional benefits byreceiving periodic examinations (CMS 2014c).Adult dental benefits may also differ amongMedicaid managed care plans. Medicaid managedcare plans have the authority to apply any savingsthey realize through efficient management to theprovision of additional benefits to enrollees, forinstance, additional dental coverage for adultsthat goes beyond state requirements (Schneiderand Garfield 2002). In Florida, Georgia, Kansas,and Maryland, for example, Medicaid programsenroll a large number of beneficiaries in managedcare plans that provide adult dental benefits notavailable to beneficiaries enrolled in fee-for-serviceMedicaid (Yarbrough et al. 2014).Changes in adult dental benefit levelsunder MedicaidBecause adult dental benefits under Medicaid areoptional, many states make changes to benefits ona regular basis (Figure 2-2): 32Between 2003 and 2012, 20 states madeat least one large-scale change in dentalbenefits for non-pregnant, non-disabled adultMedicaid enrollees (for example, adding anadditional service to a program that waspreviously emergency services only), andnine of those states made two or morebenefit changes within that time period.Between 2003 and 2012, 32 benefit changeswere made among 20 states, with 10 statesmaking more than one change—14 of theseFIGURE 2-2. Changes in Medicaid Adult DentalBenefits by State, 2003–20122003 2004 2006 2008 2010 ConnecticutDelawareDistrict of kaNevadaNew HampshireNew JerseyNew MexicoNew YorkNorth CarolinaNorth DakotaOhioOklahomaOregonPennsylvaniaRhode IslandSouth CarolinaSouth est VirginiaWisconsinWyomingNo serviceEmergency onlyMore than emergencyNotes: Data were analyzed through 2012, the most recentyear for which data are available. The above illustration doesnot reflect additional dental benefits that may be availableto pregnant women or adults with disabilities. Variationexists in the type of and amount of benefits among states inthe category of “more than emergency services,” which caninclude anything from one service in one category to multipleservices in all service categories. Due to the scope of thiscategory, benefit changes can occur within the category.Additionally, states create their own definitions of emergencydental services, so some states that are listed in the “noservices” category may classify themselves as providing nodental benefits despite covering emergency dental services.Source: MACPAC analysis of Kaiser Family Foundation 2014.June 2015
Chapter 2: Medicaid Coverage of Dental Benefits for Adultschanges decreased dental benefits, and18 increased dental benefits. Between 2003 and 2012, 12 statesconsistently offered no benefits or emergencyservices only, and 19 states consistentlyoffered more than emergency services.The year 2010 marked the greatest largescale change—five states increased benefitsand six states decreased benefits.In 2012, no states increased benefits whilethree states decreased benefits.Examples of recent changes in several statesinclude the following: California eliminated coverage of nonemergency dental services for adults inMedi-Cal in 2009 (CHCF 2011). As of May1, 2014, many adult dental benefits wererestored for Medi-Cal enrollees, includingpreventive care, restorative care, periodontalservices, and dentures (California DentalAssociation 2014).In 2011, the Idaho legislature limitedMedicaid dental benefits for adults age 21and older to emergency services only (IdahoDepartment of Health and Welfare 2011;H.B. 260, 61st Leg., 1st Reg. (Idaho 2011)).In 2012, Illinois passed legislationrestricting dental services covered byMedicaid to emergency services only (S.B.2840, 97th Leg., 1st Reg. (Ill. 2012)). Thenin 2014, the legislature expanded servicescovered to include limited fillings, rootcanals, dentures, and oral surgery services(S.B. 741, 98th Leg., 1st Reg. (Ill. 2014)).In recent years South Carolina has coveredonly emergency dental services to adultMedicaid enrollees. On December 1, 2014,the state began covering cleanings, fillings,and extractions with a 750 per yearmaximum benefit (Holleman 2014).Report to Congress on Medicaid and CHIPUse of Dental ServicesMedicaid enrollees and individuals in other lowincome populations use dental services less oftenthan other health services. An analysis of data fromthe 2012 MEPS found that among adult Medicaidenrollees age 21 and older, 20 percent reported adental visit within the past year while 80 percentreported a visit to any other type of office-basedmedical p
age 20 to 64 have had dental caries, commonly referred to as cavities, in their permanent teeth (NIDCR 2015). Of those with dental caries, adults with incomes below 100 percent of the federal poverty level (FPL) are more than three times as likely to have untreated dental caries than