Transcription
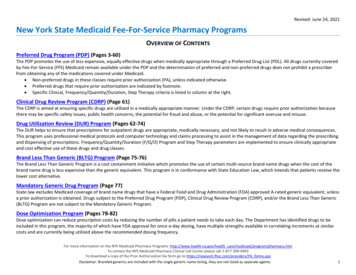
Revised: June 24, 2021New York State Medicaid Fee-For-Service Pharmacy ProgramsOVERVIEW OF CONTENTSPreferred Drug Program (PDP) (Pages 3-60)The PDP promotes the use of less expensive, equally effective drugs when medically appropriate through a Preferred Drug List (PDL). All drugs currently coveredby Fee-For-Service (FFS) Medicaid remain available under the PDP and the determination of preferred and non-preferred drugs does not prohibit a prescriberfrom obtaining any of the medications covered under Medicaid. Non-preferred drugs in these classes require prior authorization (PA), unless indicated otherwise. Preferred drugs that require prior authorization are indicated by footnote. Specific Clinical, Frequency/Quantity/Duration, Step Therapy criteria is listed in column at the right.Clinical Drug Review Program (CDRP) (Page 61)The CDRP is aimed at ensuring specific drugs are utilized in a medically appropriate manner. Under the CDRP, certain drugs require prior authorization becausethere may be specific safety issues, public health concerns, the potential for fraud and abuse, or the potential for significant overuse and misuse.Drug Utilization Review (DUR) Program (Pages 62-74)The DUR helps to ensure that prescriptions for outpatient drugs are appropriate, medically necessary, and not likely to result in adverse medical consequences.This program uses professional medical protocols and computer technology and claims processing to assist in the management of data regarding the prescribingand dispensing of prescriptions. Frequency/Quantity/Duration (F/Q/D) Program and Step Therapy parameters are implemented to ensure clinically appropriateand cost effective use of these drugs and drug classes.Brand Less Than Generic (BLTG) Program (Page 75-76)The Brand Less Than Generic Program is a cost containment initiative which promotes the use of certain multi-source brand name drugs when the cost of thebrand name drug is less expensive than the generic equivalent. This program is in conformance with State Education Law, which intends that patients receive thelower cost alternative.Mandatory Generic Drug Program (Page 77)State law excludes Medicaid coverage of brand name drugs that have a Federal Food and Drug Administration (FDA) approved A-rated generic equivalent, unlessa prior authorization is obtained. Drugs subject to the Preferred Drug Program (PDP), Clinical Drug Review Program (CDRP), and/or the Brand Less Than Generic(BLTG) Program are not subject to the Mandatory Generic Program.Dose Optimization Program (Pages 78-82)Dose optimization can reduce prescription costs by reducing the number of pills a patient needs to take each day. The Department has identified drugs to beincluded in this program, the majority of which have FDA approval for once-a-day dosing, have multiple strengths available in correlating increments at similarcosts and are currently being utilized above the recommended dosing frequency.For more information on the NYS Medicaid Pharmacy Programs: http://www.health.ny.gov/health care/medicaid/program/pharmacy.htmTo contact the NYS Medicaid Pharmacy Clinical Call Center please call 1-877-309-9493To download a copy of the Prior Authorization fax form go to https://newyork.fhsc.com/providers/PA forms.aspDisclaimer: Branded generics are included with the single generic name listing, they are not listed as separate agents.1
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPREFERRED DRUG LIST – TABLE OF CONTENTSI. ANALGESICS . 3II. ANTI-INFECTIVES. 8III. CARDIOVASCULAR . 12IV. CENTRAL NERVOUS SYSTEM . 18V. DERMATOLOGIC AGENTS . 28VI. ENDOCRINE AND METABOLIC AGENTS . 34VII. GASTROINTESTINAL . 40VIII. HEMATOLOGICAL AGENTS . 43IX. IMMUNOLOGIC AGENTS . 45X. MISCELLANEOUS AGENTS . 46XI. MUSCULOSKELETAL AGENTS . 47XII. OPHTHALMICS . 48XIII. OTICS. 52XIV. RENAL AND GENITOURINARY . 53XV. RESPIRATORY . 55XVI. SUBSTANCE USE DISORDER AGENTS . 612
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersI. AnalgesicsNon-Steroidal Anti-Inflammatory Drugs (NSAIDS)diclofenac 1% topical gelibuprofen Rx (tablet)ibuprofen OTC (susp)indomethacinketorolacmeloxicam (tablet)naproxen (tablet)naproxen ECpiroxicamsulindac1 Preferred as of 04/22/20212 Non-Preferred as of 04/22/2021Arthrotec CLINICAL CRITERIA (CC)Cambia Celebrex (celecoxib) – one of the following criteria will not require PACelebrex CC Over the age of 65 yearscelecoxib CC Concurrent use of an anticoagulant agentDaypro History of GI Bleed/Ulcer or Peptic Ulcer Diseasediclofenac epolamine (generic forFlector)diclofenac/misoprostoldiclofenac potassiumdiclofenac sodiumdiclofenac sodium ERdiclofenac topical solndiflunisalDuexis etodolacetodolac ERFeldene fenoprofenFlector patchFlurbiprofenibuprofen Rx (susp)Indocin indomethacin ERketoprofenketoprofen ERketorolac nasal spray (gen Sprix )Licart meclofenamatemefenamic acidmeloxicam (capsules) (gen Vivlodex )Mobic nabumetoneNalfon Standard PA fax form: https://newyork.fhsc.com/downloads/providers/NYRx PDP PA Fax Standardized.pdf3
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersI. AnalgesicsNaprelan naproxen (susp)naproxen CRnaproxen-esomeprazolenaproxen sodiumoxaprozinPennsaid Qmiiz ODT Relafen DSSprix Tivorbex tolmetinVimovo Vivlodex Voltaren GelZipsor Zorvolex Opioids – Long-Acting CC, F/Q/Dbuprenorphine patchesfentanyl patch (12 mcg, 25 mcg, 50 mcg,75 mcg, 100 mcg)morphine sulfate ER (tablet))1 Preferred as of 04/22/20212 Non-Preferred as of 04/22/2021Arymo ERBelbuca Butrans Conzip STDuragesic fentanyl patch (37.5 mcg, 62.5 mcg,87.5 mcg)hydrocodone ERhydromorphone ERHysingla ERKadian Morphabond ERmorphine ER (capsule) (generic forAvinza)morphine ER (capsule) (generic forKadian)CLINICAL CRITERIA (CC) * Limited to a total of 4 opioid prescriptions every 30 days; Exemption fordiagnosis of cancer or sickle cell disease PA required for initiation of opioid therapy for patients on established opioiddependence therapy PA required for use if 90 MME (MME morphine milligram equivalents) ofopioid per day for management of non-acute pain (pain lasting 7 days) PA required for initiation of long-acting opioid therapy in opioid-naïvepatients. PA required for any additional long-acting opioid prescription for patientscurrently on long-acting opioid therapy. PA required for initiation of opioid therapy in patients currently onbenzodiazepine therapy PA required for any codeine- or tramadol-containing products in pts 12 yrsSTEP THERAPY (ST)Standard PA fax form: https://newyork.fhsc.com/downloads/providers/NYRx PDP PA Fax Standardized.pdf4
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersI. AnalgesicsMS Contin Nucynta ER SToxycodone EROxycontin oxymorphone ERtramadol ER STXtampza ERZohydro ERNucynta ER (tapentadol ER): Trial with tapentadol IR before tapentadol ER forpatients who are naïve to a long-acting opioidTramadol ER (tramadol naïve patients): Attempt treatment with IR formulationsbefore the following ER formulations: Conzip , tramadol ER 1 Preferred as of 04/22/20212 Non-Preferred as of 04/22/2021FREQUENCY/QUANTITY/DURATION (F/Q/D) *Belbuca (buprenorphine)Maximum 2 units per dayButrans (buprenorphine)Maximum 4 patches per 28 daysNucynta ER (tapentadol ER):Maximum 2 units per dayNucynta ER (tapentadol ER):Maximum daily dose of tapentadol IR and tapentadol ER formulations if usedin combination should not exceed 500mg/dayTramadol ER (Conzip ):Maximum 30 tablets dispensed as a 30-day supplyZohydro ER (hydrocodone ER):Maximum 2 units per day, 60 units per 30 daysHysingla ER (hydrocodone ER):Maximum 1 unit per day; 30 units per 30 daysHydromorphone ER, oxymorphone ER:Maximum 4 units per day, 120 units per 30 daysOxycodone ER (Xtampza ER):Maximum 2 units per day, 60 units per 30 days. Not to exceed a total dailydose of 160 mg or its equivalentFentanyl transdermal patch (Duragesic ):Maximum 10 patches per 30 days; maximum 100 mcg/hr (over a 72-hourdosing interval)Morphine ER (excluding MS Contin products):Maximum 2 units per day, 60 units per 30 daysStandard PA fax form: https://newyork.fhsc.com/downloads/providers/NYRx PDP PA Fax Standardized.pdf5
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersI. Analgesics Morphine ER (MS Contin and Arymo ER 15 mg, 30 mg, 60 mg only): Maximum 3 units per day, 90 units per 30 days Morphine ER (MS Contin 100 mg only): Maximum 4 units per day, up to 3 times a day, maximum 120 units per 30days Morphine ER (MS Contin 200 mg only): Maximum 2 units per day, maximum 60 units per 30 days For Non-opioid Pain management alternatives please visit:https://health.ny.gov/health care/medicaid/program/opioid management/docs/non opioid alternatives to pain management.pdfThe quantity limits listed are systematically converted into Morphine MilligramEquivalents (MME) for the purpose of prospective drug utilization review/clinicalediting.*Exemption from requirements for diagnosis of cancer, sickle cell disease, or hospicecare.Opioids – Short-Acting CCbutalbital / APAP / caffeine / codeine F/Q/Dcodeine F/Q/Dcodeine / APAP F/Q/Dhydrocodone / APAP F/Q/Dhydrocodone / ibuprofen F/Q/DLortab (elixir) F/Q/Dmorphine IR F/Q/Doxycodone / APAP F/Q/Dtramadol F/Q/D1 Preferred as of 04/22/20212 Non-Preferred as of 04/22/2021Apadaz F/Q/DCLINICAL CRITERIA (CC) *benzhydrocone / APAP F/Q/D Limited to a total of 4 opioid prescriptions every 30 days.butalbital compound/ codeine F/Q/D Initial prescription for opioid-naïve patients limited to a 7-day supply.butorphanol nasal spray PA required for initiation of opioid therapy for patients on established opioiddihydrocodeine / APAP / caffeine F/Q/Ddependence therapy.Dilaudid F/Q/D PA required for use if 90 MME of opioid per day for management of nonFiorinal / codeine F/Q/Dacute pain ( 7 days)hydromorphone F/Q/D Exception for diagnosis of cancer or sickle cell disease, or hospice programlevorphanol PA is required for opioid-naïve patients for prescription requests 50 MME permeperidineday.Nalocet ST, F/Q/DNucynta PA required for continuation of opioid therapy beyond an initial 7-day supplyOxaydo in patients established on gabapentin or pregabalinoxycodone F/Q/D PA required for initiation of opioid therapy in patients currently onoxycodone / aspirin F/Q/Dbenzodiazepine therapyoxycodone / ibuprofen F/Q/D PA required for any codeine- or tramadol-containing products in pts 12 yrsoxymorphone F/Q/DSTEP THERAPY (ST)Standard PA fax form: https://newyork.fhsc.com/downloads/providers/NYRx PDP PA Fax Standardized.pdf6
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersI. Analgesicspentazocine / naloxonePercocet F/Q/DPrimlev F/Q/DRoxicodone F/Q/Dtramadol / APAP F/Q/DUltracet F/Q/DUltram Nucynta (tapentadol IR) – Trial with tramadol and 1 preferred opioid beforetapentadol immediate-release (IR)FREQUENCY/QUANTITY/DURATION (F/Q/D)Quantity Limits: Apadaz (benzhydrocodone/APAP): Maximum 12 units per day Nucynta (tapentadol IR): Maximum 6 units per day; 180 units per 30 days Nucynta (tapentadol IR): Maximum daily dose of tapentadol IR and tapentadol ER formulations usedin combination not to exceed 500 mg/day tramadol – Maximum 400 mg per day Morphine and congeners immediate-release (IR) non-combination products(codeine, hydromorphone, morphine, oxycodone, oxymorphone): Maximum 6 units per day, 180 units per 30 daysAdditional/alternate parameters: To be applied to patients without a documentedcancer or sickle cell diagnosis. Morphine and congeners immediate-release (IR) combination productsmaximum recommended: acetaminophen (4 grams) aspirin (4 grams) ibuprofen (3.2 grams) or the FDA-approved maximum opioid dosage as listed in the PI, whichever islessDuration Limits:1 Preferred as of 04/22/20212 Non-Preferred as of 04/22/2021Standard PA fax form: https://newyork.fhsc.com/downloads/providers/NYRx PDP PA Fax Standardized.pdf7
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersI. Analgesics 90 days for patients without a diagnosis of cancer or sickle-cell disease.For Non-opioid Pain management alternatives please visit:https://health.ny.gov/health care/medicaid/program/opioid management/docs/non opioid alternatives to pain management.pdfThe quantity limits listed are systematically converted into morphine milligramequivalents (MME) for the purpose of prospective drug utilization review/clinicalediting.*Exemptions from requirements for diagnosis of cancer, sickle cell disease, or hospicecarePreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersII. Anti-InfectivesAntibiotics – Inhaled CC, F/Q/DBethkis BLTGCayston Kitabis Pak BLTGCLINICAL CRITERIA (CC)TOBI Podhaler Confirm diagnosis of FDA-approved or compendia-supported indicationTOBI (solution)tobramycin (generic for Bethkis , FREQUENCY/QUANTITY/DURATION (F/Q/D) Aztreonam (Cayston)Kitabis , Tobi ) solution 3 ampules (3 mL) per day 84 ampules (84 mL) per 56 day regimen (28 days on, 28 days off) Tobramycin inhalation solution (Bethkis, TOBI, Kitabis Pak) 2 ampules (8 mL Bethkis, 10 mL TOBI, Kitabis Pak) per day 56 ampules (224 mL Bethkis, 280 mL TOBI, Kitabis Pak) per 56 day regimen (28 days on-28days off) Tobramycin capsules with inhalation powder (TOBI Podhaler) 8 capsules per day 224 capsules per 56 day regimen (28 days on-28 days off)Anti-Fungals – Oral for Onychomycosisgriseofulvin (suspension andultramicronized)terbinafine (tablet)1 Preferred as of 04/22/20212 Non-Preferred as of 04/22/2021griseofulvin (tablet)itraconazoleitraconazole solution (generic forSporanox)Sporanox Standard PA fax form: https://newyork.fhsc.com/downloads/providers/NYRx PDP PA Fax Standardized.pdf8
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersII. Anti-InfectivesAnti-Virals – OralacyclovirvalacyclovirfamciclovirValtrex Zovirax Cephalosporins – Third GenerationcefdinircefiximecefpodoximeSuprax Fluoroquinolones – Oralciprofloxacin (suspension, tablet) Baxdela Cipro (suspension, tablet)levofloxacin (tablet)levofloxacin (solution)moxifloxacinofloxacin (tablet)Hepatitis B Agentsadefovir dipivoxilBaraclude (solution)entecavirEpivir-HBV (solution)lamivudine HBV1 Preferred as of 04/22/20212 Non-Preferred as of 04/22/2021Baraclude (tablet)Epivir-HBV (tablet)Hepsera Vemlidy Standard PA fax form: https://newyork.fhsc.com/downloads/providers/NYRx PDP PA Fax Standardized.pdf9
Revised: June 24, 2021NYS Medicaid Fee-For-Service Preferred Drug ListPreferred DrugsNon-Preferred DrugsPrior Authorization/Coverage ParametersII. Anti-InfectivesHepatitis C Agents – Injectable F/Q/DPegasys PegIntron NoneFREQUENCY/QUANTITY/DURATION (F/Q/D) PA required for the initial 14 weeks therapy to determine appropriate duration of therapybased on genotype, prior treatment and response, presence of cirrhosis, and HIVcoinfection. Further documentation required for continuation of therapy at weeks 14 and 26. After 12 weeks of therapy, obtain a quantitative HCV RNA. Continuation is supported ifundetectable HCV RNA or at least a 2 log decrease compared to baseline. After 24 weeks of therapy obtain a HCV RNA. Continuation for genotype 1 and 4 issupported if undetectable HCV RNA. Maximum duration of 48 weeks for: Treatment-naïve patients or prior relapsers with cirrhosis and HIV co-infection Prior non-responders (including prior partial and null responders) with or without cirrhosisand with or without HIV co-infectionHepatitis C Agents – Direct Acting AntiviralsCC, F/Q/DMavyret ribavirinsofosbuvir/velpatasvir CC, F/Q/D(generic for Epclusa )Vosevi CC, F/Q/D1 Preferred as of 04/22/20212 Non-Preferred as of 04/22/2021CC, F/Q/DEpclusa Harvoni CC, F/Q/Dledipasvir/sofosbuvir CC, F/Q/D(generic for Harvoni )Sovaldi CC, F/Q/DViekira Pak CC, F/Q/DZepatier CC, F/Q/DCLINICAL CRITERIA (CC) Confirm diagnosis of FDA-approved or compendia-supported indication For patients being retreated require confirmation of patient readiness and adherence Evaluation by using scales or assessment tools readily to determine a patient’s readiness toinitiate HCV treatment, specifically drug and alcohol abuse potential. Assessment tools are availableto healthcare practitioners at: ing-toolsOR https://prepc.org/.The Hepatitis C Worksheet can be accessed Rx PDP PA Worksheet Prescribers HepC.docxStandard PA fax form: https://newyork.fhsc.com/downloads/providers/NY
Revised: April 22, 2021 NYS Medicaid Fee-For-Service Preferred Drug List 1 Preferred as of 04/22/2021