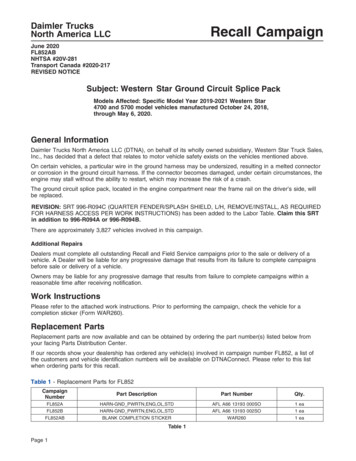
Transcription
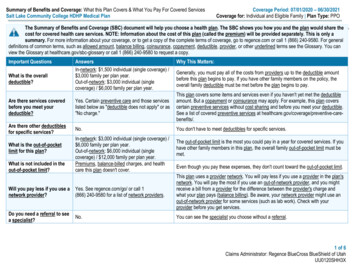
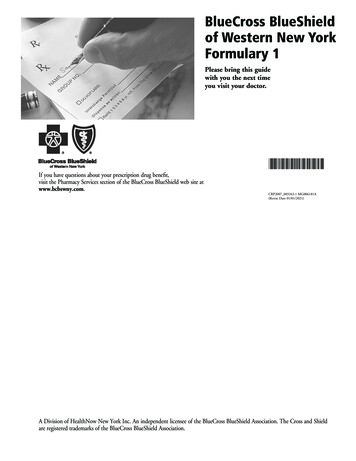
BlueCross BlueShieldof Western New YorkFormulary 1Please bring this guidewith you the next timeyou visit your doctor.If you have questions about your prescription drug benefit,visit the Pharmacy Services section of the BlueCross BlueShield web site atwww.bcbswny.com.CRP2007 003343.1 MG006181A(Revise Date 01/01/2021)A Division of HealthNow New York Inc. An independent licensee of the BlueCross BlueShield Association. The Cross and Shieldare registered trademarks of the BlueCross BlueShield Association.
TABLE OF CONTENTSIntroduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Understandingthe symbols usedthroughout this book . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Usingiiiiiithis formulary book to help contain costs . ivSave Money on Your Prescription Drugs. . . . . . . . . . . . . . . . .ivFinding Medications in the Guide . . . . . . . . . . . . . . . . . . . . . . . . vSection 1 — Therapeutic Drug Categories . . . . . . . . . .1Section II — Index. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8ii
The BlueCross BlueShield of Western New York Formulary 1 is a list of drugs to help guide physicians andpharmacists to select the medication that provides the appropriate treatment for the best price.IntroductionBlueCross Blue Shield of Western New York has established an independent committee of practicing physiciansand a pharmacist to help ensure that our formularies are medically sound and that they support your patients’health. This committee—called the Pharmacy and Therapeutics Committee—reviews and evaluates medicationson the formulary based on safety and efficacy to help maintain clinical integrity in all therapeutic categories.Understandingthe symbols used throughout this bookThroughout this book, you will see certain symbols that indicate a management program is in place for selectedmedications. The symbols are as follows: KeyP z u o step edit applies to this drug. Step therapy means that in order to receive the medicationAwith a step edit, a preferred medication must be tried first. Specific quantity limits apply. Quantity limits are in place to ensure members receive theappropriate amount of medication not to exceed the maximum allowable daily dosage ofmedication. Prior authorization required. Prior authorization (also referred to as coverage review)means that a healthcare professional must submit clinical documentation to obtainapproval for a member to receive the medication. Prior authorizations ensure medicationsare being used appropriately. Included in tablet-splitting program. The medication can be cut in half to obtain the dailydose of medication (i.e., 20mg daily of simvastatin can be obtained by 1/2 tablet ofsimvastatin 40mg). A member will receive a 1-month supply for half their regular 1-monthcopay. Access restricted to specialty pharmacy. Medications must be obtained through a specialtypharmacy. Custom Home Delivery. The medication should be obtained through the mail service pharmacy. The medication is subject to a retail refill allowance. Affordable Care Act (ACA) Preventive Drug. The medication is included on the ACAPreventive Drug List.iii
Usingthis formulary book to help contain costsMany employers, benefit sponsors, and individuals may use the formulary to help manage theoverall cost of providing prescription drug benefits. The formulary offers a wide range of outpatientmedications.Because there are over 40,000 Food and Drug Administration (FDA)-approved prescription drugs onthe market, not all tier 3 drugs can be listed in this formulary guide. We have included in this printedformulary guide the drugs that are most commonly prescribed for our members. If you have anyquestions regarding coverage of a drug, please call the customer service number on your card.Save Money on Your Prescription DrugsHere’s what you can do to save money:1. Bring this member guide to your doctor and review the cost-saving information below.2. Ask your doctor whether a drug listed in this guide is right for you.*Tier 1Tier 2Lowest cost to youTier 3Highest cost to youThe amount you pay for a drug is determined by which medication you purchase and to what tier itis assigned. Some drug plans exclude certain drugs or classes of drugs from coverage. Please check yourcontract or other plan documents if you have a question about your specific drug coverage.Please refer to your plan documents to confirm your cost share for diabetic drugs and supplies. Costshare may vary by plan.Affordable Care Act (ACA) Preventive Drug ListThe Affordable Care Act (ACA) Preventive Drug List consists of medications that may be covered at 0.They are not subject to any annual deductibles, coinsurance, or copayments. Please refer to your plandocuments to confirm if the ACA Preventive Drug List applies to you.We’ve noted any drugs on the ACA Preventive Drug List within this guide. Please consult the key onpage iii. This list is reviewed periodically and is subject to change.The presence of a drug on this list does not guarantee coverage. Drugs on this list may require priorauthorization, step-edits, and quantity limits. Restrictions may apply to certain brand-name ACAmedications with generic equivalents. Other restrictions may apply according to U.S. Preventive ServicesTask Force (USPSTF) recommendations, which define ACA coverage requirements. These restrictionsmay be based on age, dose, diagnosis, and others as recommended by USPSTF. Both prescription andover-the-counter (OTC) products are eligible to be covered when prescribed by a licensed health careprovider and require a valid prescription.* Some plan designs require that you use a Tier 1 generic drug if a generic is available.Disclaimer: The BlueCross BlueShield of Western New York Medication Guide is subject to change, as we regularly reviewmedications and existing therapies for inclusion in the BlueCross BlueShield of Western New York Formulary 1. The tierthat a medication is currently in may change during the effective dates of the guides due to generic availability.iv
Contraceptive Coverage under New York Insurance LawContraceptives (for members whose benefits align with contraceptive coverage requirements underNew York Insurance Law): All tier 1 contraceptives are covered at a 0 copayment. Brand-namecontraceptives without a generic equivalent are covered at a 0 copayment. Brand-name contraceptiveswith a generic equivalent are covered at the copayment based on your plan design unless deemedmedically necessary by the prescriber. The prescriber must designate “DAW” (Dispense as Written) onthe prescription in order for the brand-name contraceptive with a generic equivalent to be consideredmedically necessary and covered at a 0 copayment. Both prescription and over-the-counter (OTC)products are covered only when prescribed by a licensed health care provider and require a validprescription. Please refer to your plan documents to confirm your cost share for contraceptives. Costshare may vary by plan.Contraceptives may include implantable rods, intrauterine devices (IUD), shots/injections, oralcontraceptives, patches, vaginal contraceptive rings, diaphragms, sponges, cervical caps, femalecondoms, spermicides, and emergency contraceptives. Please see the “Women’s Health” section of thisguide for specific product examples.Custom Home Delivery: Members must obtain maintenance medications at mail-order after retail allowance isexhausted for members with Custom Home Delivery Benefit.Finding Medications in the GuideThis guide lists medications two different ways:Section 1: Alphabetically by drug category (such as Diabetes, Heart or Pain/Arthritis) Locate a category and drug on the guide and you will see the tier and copayment for thatdrug—Tier 1, Tier 2 or Tier 3—which determines your copayment. To determine if a drug isa generic or brand-name medication, look at the name of the drug. Generic medications arelower case (e.g., amoxicillin), and brand-name medications are capitalized (e.g., Advair).Section 2: Alphabetically by drug name. Use this list to find your drug.Questions? Please call Pharmacy Services at 1 800 939-3751 if you have any questions about theBlueCross BlueShield of Western New York Formulary 1. For the most up-to-date version of the Guide,visit the Pharmacy Services section of our web site at www.bcbswny.com.v
Section I — TherapeuticTIERTIERAllergy/Cough & ColdAntihistamines & draminehydroxyzine HClhydroxyzine oephedrineSemprex-DzoClarinex-Dzodesloratadine zGrastek zOdactra zOralair zPalforzia zRagwitekExpectorant & Cough n DMHycodanRondec DM/TRVituzMucolytic Agentsacetylcysteine inh soln.Nasal Medicationsazelastine nasal spraybudesonide nasal sprayClarisprayFlonase Allergy ReliefFlonase Sensimistzofluticasone nasal sprayipratropium nasal sprayzomometasone nasal sprayzNasacort Allergy 24HRRhinocort Allergytriamcinolone nasal sprayAtrovent Nasal SprayPzo Beconase AQDymistazoflunisolide nasal sprayPzo Nasacort AQPzo OmnarisPzo Qnasl zXhancePzo ZetonnaAlzheimer 111333333333donepezilergoloid mesylatesgalantaminegalantamine ERmemantinememantine ERrivastigminerivastigmine patchNamzaric111111112K-PhosAlkalinizerspotassium gicszoxybutyninzoxybutynin ERzOxytrol for er/KidneyAcidifiersdrug categories13111111ztolterodine ERztrospiumztrospium ERzMyrbetriqzToviazPzDetrolPzDetrol LAPzDitropan XLPzEnablexPzGelniquePzOxytrolPzSancturaPzSanctura XRCholinergic AgentsUrecholineMiscellaneous tithromboticsanagrelide aspirin 81mg OTC aspirin 325mg noxaparinfondaparinux tyBevyxxazoDurlazaInnohepzPradaxazSavaysaOther Blood Modifiersocilostazol deferasiroxpentoxifylline ztrientine zActimmune Aranesp LeukineoMiacalcin inj. Neulasta zPromacta Retacrit zRevlimid Strensiq Udenyca Zarxio Alprolix zCablivi deferiprone zDoptelet Eloctate zEndari Epogen Exjade Ferriprox Fulphila Granix Hemlibra Jadenu Jivi Mircera zMulpleta Neupogen Nivestym Omontys zOxbryta Procrit zTavalisse 33333333Alkylating Agentscyclophosphamide1Cancer DrugsKEY: P A step edit applies to this drug.z Specific Quantity Limits Apply. Prior Authorization Required.u Included in Tablet-Splitting metabolites capecitabinemercaptopurinemethotrexatePurixan zInqovi OnuregTrexall zXatmepHormones anastrozolebicalutamide exemestaneflutamide letrozole leuprolidemegestrolzo raloxifene tamoxifenFareston zNubeqaMiscellaneous zabiraterone acetate 250mg zerlotinibetoposide zeverolimus (generic Afinitor)hydroxyurea zimatinibnilutamide temozolomide zAlecensa zArcalyst zBosulif zCabometyx zCaprelsa zCometriq zCotellic zErivedge zFarydak zGilotrif Hycamtin capsule zIbrance zIclusig zImbruvica zInlyta Intron A zIressa zJakafi zLenvima zLonsurf zLynparzaLysodrenMatulane zMekinistMesnex zNexavar zNinlaro zOdomzo zPomalyst zSprycel Stivarga zSutent zSylatron zSynribo zTafinlar zTagrisso zTasigna Thalomid zTykerb zValchlor zVerzenio zVotrient zXalkori zXtandi zZelboraf zZolinza zZydelig zZykadia zZytiga 500mg Pz Afinitor 22222222222222233 z z z z z z z z Pz z z z Pz z z z z z z z z z z z z z z z z z z z z z 3313Please refer to your plan documents to confirm your costshare for diabetic drugs. Cost share may vary by plan.Antidiabetic Agents, InjectableBasaglarzBydureonzByettaHumalog insulinHumulin (all types)LantusLyumjevzOzempiczSoliqua pidraPFiaspPInsulin esibazXultophyAntidiabetic Agents, Glucose Elevating glipizide ERzglipizide/metforminglyburideglyburide micronizedmetformin Access restricted to specialty pharmacy.o Custom Home Delivery. ACA Preventive esimptaKisqaliKisqali Femara extaVitrakviVizimpro Xgeva zXospata zXpovio zYonsa zZejula Pz Zytiga 250mgRexinoids bexarotene Targretin gel2222222222222333333333333111111111
Section I — tive Agentsbacitracin ophthbacitracin/polymyxinciprofloxacin ophtherythromycin ophthgatifloxacingentamicin ophthmoxifloxacin 0.5% (generic Vigamox)neomycin/bacitracin/poly Bofloxacin ophthpolymyxin B/TMPsulfacetamide 10%tobramycin solnBesivanceMoxezaTobrex ointmentAzasiteCiloxanTobrex solutionAnti-inflammatoryfluorometholone ophthloteprednol etabonate suspprednisolone acetateprednisolone sod phosphateFML ForteFML S.O.P.Lotemax gel, ointmentPred MildFlarexMaxidexAnti-inflammatory/Anti-infective combinationsdexameth/neomycin/poly Bneomycin/bacitracin/poly B/HCsulfacetamide/prednisolone ophthtobramycin/dexamethTobradex ointmentTobradex STZyletMaxitrol ophthPred-GAntiviralzfamciclovir ophthtrifluridineBeta-Blockers (Eye)obetaxolol HClDiabetic SuppliesocarteololPlease refer to your plan documents to confirm your olevobunololcost share for diabetic supplies. Cost share may vary ometipranololby plan. Test strips other than OneTouch requireotimololprior authorization.oBetoptic-SoIstalolOneTouch Test StripsCarbonic Anhydrase InhibitorsPAccu-Chekodorzolamide 2% eye dropsPAscensia Breezeodorzolamide/timolol eye ocarpinePTRUEtestPhospholine nti-infective AgentsRestasisacetic acid otic1 zXiidraacetic acid/aluminum acetate1 zciprofloxacin otic1 zCequaofloxacin otic1 CystadropsDomeboro3 zOxervateXtoro3 PoRhopressaAnti-infective/Anti-inflammatory combinations zoRocklatanacetic acid HC otic1 Mydriaticsciprofloxacin/dexamethasone1atropine sulfate ophthneomycin/polymyxin/HC otic1homatropineCipro HC3tropicamideEyeNSAIDsbromfenacAntiallergy Agents (Eye)diclofenacazelastine ophth1flurbiprofen ophthcromolyn ophth1Ilevroolopatadine 0.2% drop1Nevanacolopatadine ophth1ProlensaAlomide2Acular PFAlrex2Bepreve2 Prostaglandin Analogues/Prostaminesketotifen opthalmic solution3bimatoprost 0.03%metformin ER (generic Glucophage XR) 1metformin/glyburide1metformin Glyxambi2zInvokamet2zInvokamet XR2zInvokana2zJanumet2zJanumet XR2zJanuvia2zJardiance2Jentadueto2zJentadueto XR2Juvisync2zRybelsus2zSynjardy2zSynjardy XR2Tradjenta2zTrijardy XR2zXigduo XR2 iglyze XR3Pz metformin ER (not generic Glucophage XR) EY: P A step edit applies to this drug.z Specific Quantity Limits Apply. Prior Authorization Required.u Included in Tablet-Splitting Programdrug categories (cont’d)olatanoprostoLumigan 0.01%oXelprosPIzbaPResculaPoTravatan Zotravoprost (generic Travatan onidineoAlphagan P 0.1% UpneeqVasoconstrictorsnaphazolinephenylephrine ophth333111111111111222333Goutz1111222233z zz zHeartallopurinolcolchicine (generic itigareDuzalloGloperbaZurampicAngiotensin Converting Enzyme prilotrandolapril zoEpaned zoQbrelisAngiotensin II Antagonistszoeprosartan anzovalsartanzoEdarbiPzPrexxartanAnti-Adrenergic Blockers Centrally Actingoclonidine, oral, ne zNortheraAnti-Adrenergic Blockers PeripheralodoxazosinoprazosinoterazosinoCardura enoneopropafenone SRoquinidine gluconatequinidine sulfate SRosotalolLanoxinoMultaqoNorpace CRAntilipidemicszuo atorvastatin 1111111111112231111ezetimibefenofibrate (generic)fenofibric acid, tabgemfibrozillovastatinniacin ERniacin IR 500mg tabletniacin (OTC)zoniacin/simvastatinzuo pravastatinzo rosuvastatinzuo simvastatinAdvicoroColestidFenofibrate 50mg, 150mg cap (brand) zKynamrooLipofeno Livalo zoPraluent zoRepathaVascepazo Altoprevzuo CrestorzEpanovazo Ezallorzoezetimibe-simvastatinFenofibrate 160mg tab (brand)zofenofibric acid, capsule DRzo fluvastatin zJuxtapidzuo Lescolzo Lescol XLzuo Lipitor zoNexlizet zoNexletolzNikitazomega-3 acid ethyl esterszOmtrygzuo Pravacholzuo Zocorzo ZypitamagBeta arvedilolocarvedilol ERolabetalolometoprololometoprolol mololoBystolicoInnopran XLHemangeolCalcium Channel Blockersoamlodipineocartia XTodiltia XTodiltiazemodiltiazem CD/SR/ER/XRofelodipine ERoisradipineonicardipineonifediac CConifedical XLonifedipineonifedipine SRonimodipineonisoldipineoverapamil/SRPzo ConjupriDynacirc/CRPKaterziazoNymalizeCombination azepril/HCTZzoooozuo oP Access restricted to specialty pharmacy.o Custom Home Delivery. ACA Preventive 111111111122311111111111111133331111111
Section I — ZByvalsonTekturna azolamide oCarospirMiscellaneous Cardiovascular Agentszoeplerenone zicatibantmidodrineoranolazine ER ztolvaptan zBerinert zCinryzezoEntresto zRuconest zSamsca 15mgPzConsensizoCorlanor zFirazyr zHaegardaoRanexa zSamsca 30mg zTakhzyroVecamyl zVyndaqel zVyndamaxPulmonary Arterial Hypertension zalyq zambrisentan zbosentan epoprostenol zsildenafil 20 mg tab ztadalafil (generic Adcirca) zAdempas zOpsumit zTracleer tab for susp zTyvaso zUptravi Pz Letairis Orenitram Pz Revatio Pz sildenafil suspension Pz Tracleer tab veletri Pz Ventavisdrug
The formulary offers a wide range of outpatient medications. Because there are over 40,000 Food and Drug Administration (FDA)-approved prescription drugs on the market, not all tier 3 drugs can be listed in this formulary guide. We have included in this printed formulary guide the