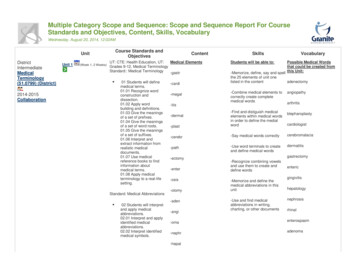
Transcription
HAI, NHSN and VBP:What’s New and What You Need To KnowChristine Martini-Bailey RN, BSN, CSSGBDirector, Quality Improvement and Patient SafetyHealth Services Advisory Group (HSAG)April 27, 2017
Objectives Review the 2017 updates to NationalHealthcare Safety Network (NHSN) PatientSafety Component for Healthcare AssociatedInfections (HAI) Understand the changes in NHSN due to there-baselining Identify the impact of NHSN re-baselining onthe Centers for Medicare & Medicaid Services(CMS) Value-Based Purchasing (VBP)2
2017 NHSN Patient SafetyComponent Updates3
Updates to Organisms ListsUpdates and additions to: NHSN All Organism list NHSN Mucosal Barrier list NHSN Common Commensal listComplete lists available from the Centers for Disease Control and Prevention /clabsi/index.html(Under Supporting Materials section)4
Flow Diagram—Event Determination5Source: CDC, available at https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual current.pdf
Building Blocks of NHSN Patient ComponentSurveillance Definitions*See SSI surveillance protocol See LabID and VAEsurveillance protocolsN/A Not applicableSSI Surgical Site infectionVAE ventilator-associated pneumonia /pcsmanual current.pdf
Transfer RuleIf the date of the event is the day oftransfer/discharge, or the next day, the infection isattributed to the transferring location.7
Endocarditis (ENDO) Extended Infection Window Period (IWP)– 21 days– 10 days before diagnostic test– 10 days after the diagnostic test Extended Repeat Infection Timeframe (RIT)– Duration of admission Extended ENDO Secondary Bloodstream Infection(BSI) Attribution Period to the ENDO IWP andremaining duration of the admission for theorganism that is used to meet the ENDO criterion8
GIT (GI Tract) Criterion 2c Modification Patient has at least two of the following signs orsymptoms compatible with infection of the organ ortissue involved: fever ( 38 C), nausea, pain ortenderness, odynophagia or dysphagia And at least one of the following:– Organisms identified from blood by a culture or non-culturebased microbiologic testing method which is performed forpurposes of clinical diagnosis or treatment. The organism(s)identified in the blood must contain at least one MBIorganism: See Appendix A of the BSI protocol.– AND– Imagining test evidence suggestive of gastrointestinalinfection, which if equivocal is supported byclinical correlation.9MBI mucosal barrier injury
Other Definitional Changes for 2017ORAL—Added back to criterion 3a, “from mucosalscrapings or exudate”3. Patient has at least one of the following signs orsymptoms with no other recognized cause: ulceration,raised white patches on inflamed mucosa, or plaques onoral mucosaAnd at least one of the following:a. Virus identified from mucosal scraping or excaudateby a culture or non-culture based microbiologic testingmethod which is performed for purposes of clinicaldiagnosis or treatment.10
Other Definitional Changes for 2017LUNG, SA, and NEC-provided guidance to allowclinical correlation to be used in cases whereimaging tests are equivocal for infection. (LUNG 3) Patient has imaging test evidence ofabscess or infection (excludes imaging testevidence of pneumonia) which if equivocal issupported by clinical correlation (i.e., physiciandocumentation of antimicrobial treatment forlung infection).11SA Spinal abscess without meningitisNEC Necrotizing enterocolitis
Pathogen Assignment Additional eligible pathogens identified withina RIT are added to the event. Pathogen exclusions for specific infectiondefinitions (ex. UTI, PNEU) also apply tosecondary BSI pathogen assignment.– Excluded pathogens must be attributed to anotherprimary site-specific BSI. A BSI pathogen may be reported for morethan one infection source.12UTI urinary tract infectionPNEU pneumoccal
Central Line-Associated Bloodstream Infection(CLABSI) ChangesMBI Exclusion All facility types Exclude MBI-laboratory confirmedbloodstream infections (LCBIs)Resources: MBI-LCBIs ources/mbianalysis.pdf Summary Data Line urces/summarylinelist.pdf13Source: CDC, available at seline-sirchanges-applicable-to-cms-qrp.pdf
Surgical Site Infection (SSI) ChangesSSI Exclusions Acute care hospitals American Society of Anesthesiologists(ASA) missing BMI: If BMI 60 or BMI 12 Gender is missing or gender is “O” Medical affiliation is missing/incomplete (annual survey) Bed number missing (annual survey) Present at time of surgery (PATOS) Age 109 years Procedure duration outliers Closure technique missingBMI body mass index14Source: CDC, available at selinesir-changes-applicable-to-cms-qrp.pdf
SSI Changes (cont.)Resources Exclusion sources/ssi-sir tips.pdf Line List of resources/faq-procedure-line-list.pdf Analyzing Procedure Closure esources/proceduresclosuretechnique.pdf15
Tools Available Electronic HAI Present on Admission (POA)Worksheet Generator– Requires user to ensure infection criterion are met andto enter correct dates– Generates worksheet with IWP, DOE, RIT, 2nd BSIAttribution Period– Located under “Supporting Materials”– Does not store information or send information to NHSN16Source: CDC, available at https://www.cdc.gov/nhsn/poa/index.html
American Journal of Infection Control NHSNCase-Study Series Additional educational tool Quarterly publication Addresses common surveillance scenarios– CLABSI, CAUTI, VAE, SSI, MDRO/CDI Test your knowledge Quiz and answers via web link17CAUTI catheter-associated urinary tract infectionsMDRO/CDI multidrug-resistant organism & Clostridium difficile infection
Complete List Revisions18Source: CDC, available at y-2017-revisions.pdf
NHSN Changes and Re-baseline19
NHSN v8.6—Re-baseline Highlights Baseline 2 “New Standard Population” Significant changes with definitions and decreased incidenceof HAIs Used calendar year (CY) 2015 in-plan data as baseline No more “pooled means” New predictive/risk models– Multivariable Logistic Regression Models (risk-adjustment)– Negative Binomial Regression (probability)– Logistic Regression (predictive) Standard Infection Ratios (SIRs) for Critical AccessHospitals (CAHs) More SIRs for long-term acute care hospitals (LTACH) andInpatient Rehabilitation Facilities (IRFs)20
Baseline ProgressionOriginal National Baseline DataAcute CareHospitals (ACH)Long-term AcuteCare Hospitals(LTACH)InpatientRehabilitationFacilities CAUTIs2009201320132015SSIs2006–2008NoneNone2015 (ACH only)Hospital-onset C.difficile2010–2011NoneNone2015Hospital-onset MRSAbacteremia2010–2011NoneNone2015HAI TypeVAE2015MBI2015StandardizedUtilization Ratio (SUR)(all device types)21New—No Previous National Baseline Data2015MRSA Methicillin-resistant Staphylococcus aureus
Measures By FacilityHAIACHsCAHsLTACHsIRFsCLASBI (non-MBI) Central Line SUR MBI CAUTI Urinary Catheter SUR VAE Ventilator SUR “All SSI” Models—Adults “All SSI” Models—Peds “Complex A/R” Models—Adults “Complex A/R” Models—Peds “Complex 30-day” Models—Adults (COLO and HYST) MRSA Bacteremia LabID CDI LabID 22COLO ColonHYST HysterectomyA/R Admission/ReadmissionSeparatefromACHs
SSI SIR Model Review All SSI SIR Model––––Inpatient onlySuperficial, deep and organ/space SSIPrimary incision (superficial and deep)On admission, readmission and post-discharge Complex A/R SSI Model (CDC HAI Progress Report)– Inpatient only– Only deep and organ/space SSI– On admission, readmission to facility Complex 30-Day SSI Model (CMS SSI Reporting)– In plan, Inpatient Colo and Hyster– Deep incisional primary and organ/space– Within 30 days of procedure23
Impacting SIRs Annual Survey CDI Test Type Other Potential Risk Factors:– Facility bed size– Medical school affiliation– Status as a cancer hospital– Intensive care unit (ICU) location– Pediatric location24
Risk VariablesFactorCLABSICLABSI (NICU)CAUTIVAECDIMRSACDC Location Facility Type Medical SchoolAffiliation InpatientQuarterly COPrevalence Rate CDI Test Type Birthweight Length of Stay Reporting fromED/Obs LocationsFacility BedsizeICU Beds25
Risk Variables (cont.)FactorCOLOHYST Age ASA Score BMI Closure technique Diabetes Gender Cancer HospitalPatient Level Factors26
SIR Reference27Source: CDC, available at /nhsn-sir-guide.pdf
New Locations AddedCan now produce SIRs for the below units:IMPORTANT REMINDER!Mandatory CMS Reporting: All Critical Care All Medical Wards All Surgical Wards All Medical/Surgical Wards28CMS Value Based Purchasing FY 2018: All Critical CareCMS Value Based Purchasing FY 2019: All Critical Care Med, Surg, Med-Surg Wards
Standardized Utilization RatioComingSoon Summarized risk-adjusted measure Focuses on device use Uses multivariable logistic regression modelsSUR # observed device days# predicted device days Predicted number 1 1 is higher utilization 1 is lower utilization29
Implications To DataCAUTI – Example 1Baseline 1:Year# CAUTI# predSIRP-value95% CICath Days2015710.4010.6730.29310.294,1.3315,996New Baseline 2:Year# CAUTI# predSIRP-value95% CICath Days201572.5232.7740.01931.213, 5.4885,99630
Implications To DataCAUTI – Example 2Baseline 1:Year# CAUTI# predSIRP-value95% CICath Days20153060.6500.495 0.00010.340, 0.69716,963Year# CAUTI# predSIRP-value95% CICath Days20153026.7721.1210.52180.770, 1.58016,963New Baseline 2:31
Baseline By YearCan use beginning CY* 2015Do NOT use after CY 2016Only UseBaseline 2CY 2017and beyond*Calendar Year32
NHSN Changes and CMS33
Re-baseline SIRs Shared with CMSHospital I HysterSSI Colon*Please note: this table does not include Healthcare Provider (HCP) Flu, as it is notimpacted by the re-baseline.34
The Old and New—What is CMS Seeing?Baseline 1Baseline 2CMS will receive 6 quarters of data under Baseline 2.35
Hospital CompareHospital Compare—Will use NHSN Baseline 2“ data included in the December 2016 Quality Net Preview Reports willbe calculated using the updated 2015 baseline and risk models.”The Centers for Disease fication-ssi.pdf36
Value-Based PurchasingDomain I: PSI 90 Composite–15%FY 2018 and FY 2019 VBP37Safety25%25%25%25%––––––––PSI 3: Pressure UlcersPSI 6: Iatrogenic PneumothoraxPSI 7: CLABSI*PSI 8: Post-Op Hip FxPSI 12: VTE/PEPSI 13:Post-op SepsisPSI 14: Wound DehiscencePSI 15: Accidental PunctureDomain II: HAI (NHSN)–85%––––––CLABSI*CAUTISSI HysterectomySSI ColonMRSA BacteremiaCDI
VBP Program Thresholds:Safety DomainNHSNRe-baselineMeasureVBP FY 2017(Data CY 2015)VBP FY 2018(Data CY 2016)VBP FY 2019(Data CY I0.7500.8050.924MRSA0.7990.7670.854SSI Hyster0.6980.7100.762SSI Colon0.7510.82440.7830.7779360.5773210.774058PSI 9038*Note: FY2019 CAUTI and CLABSI CC and MS Wards
VBP and NHSN Baselines139Payment YearNHSN Baseline UsedFY 2018 VBPCY 2016 DataNHSN Baseline 1FY 2019 VBPCY 2017 DataNHSN Baseline 2
Reminder: CMS IPPS Reports “Snapshot” of what is beingsubmitted on your behalf to CMS Validation of your submission Only proof your data was enteredprior to the deadline Means to verify data accuracy Every submission, every time40CRITICAL
Important Reminders:CMS HAI Data41
Every Journey Begins With a Good Map!Accurate mapping is criticalAvoids incorrectreporting to tionsDescriptions current.pdfx
How Mapping Can Impact Your SIRsUnit TypeIN:ACUTE:CC:ONC MCritical Care Medical OncologyIN:ACUTE:CC:MCritical Care MedicalPredicted CLABSI41Observed CLABSI33SIR0.753.0CAD*(Threshold: 0.369) 1.24 2.6Correctly Map First: Improve Second!43*Cumulative Attributable Difference (CAD)
Mapping Re-evaluate at least annually– Location– Patient mix– Acuity Any changes in location– If just move a unit, you can remain.– If patient mix or acuity changes, you must map a new unit. Any changes in patient mix– Type of patient– Acuity of patients 80/20 rule– At least 80 percent of a particular patient type Virtual Units– When you don’t have 80 percent to map to a particular unit type, but enoughpatients to skew your predicted number of infections– Example: a medical ward that routinely has a significant number of oncologypatients44Source: CDC, available onsdescriptions current.pdf
NHSN Data Transition45
Review: Baseline By Year Baseline 1 (old): Valid through CY 2016 data Baseline 2 (new): Valid beginning CY 2015 data CY 2017 and beyond, ONLY use Baseline 2 (new)46
SIR ConfusionFY 2018 VBPCY 2016Baseline 1? ?47
Trending Data You cannot continue trending from Baseline 1 into Baseline 2.48
IncorrectNew Baseline49Cannot continuetrending beyond CY 2016
Correct OptionCommunity Memorial HospitalTrended CAUTI SIR2.5Baseline 1NHSNRe-baselineBaseline 22SIR1.510.502012201320142015Calendar Year50201620172018
Another OptionNOTE: FY2018/CY2016 data will be calculated using Baseline 1.Producing 2016 data using Baseline 2, while valid, may cause some confusion.51
Accessing Baseline Set 1 Reports“Old” Baseline ReportsBaseline Set 152
Data ReportingFacts:1. For CY 2016 data, facilities will have more than one“accurate” SIR.2. VBP will use Baseline 1 and CY 2016 data.3. Hospital Compare will use Baseline 2 and CY 2016 data.4. You can go back to CY 2015 data using Baseline 2 fortrending purposes.5. Select a baseline for internal reporting and stick to it forCY 2016 data.6. Only use Baseline 2 for CY 2017 data and beyond.53
Questions?Christine Martini-Bailey, RN, BSN, CSSGBDirector, Quality Improvement and Patient Safetycbailey@hsag.com 614.307.293654
This material was prepared by Health Services Advisory Group, the Medicare QualityImprovement Organization for Arizona, California, Florida, Ohio, and the U.S. VirginIslands, under contract with the Centers for Medicare & Medicaid Services (CMS), anagency of the U.S. Department of Health and Human Services. The contentspresented do not necessarily reflect CMS policy.Publication No. QN-11SOW-D.1-04122017-0155
VBP Program Thresholds: Safety Domain 38 Measure VBP FY 2017 (Data CY 2015) VBP FY 2018 (Data CY 2016) VBP FY 2019 (Data CY 2017) CAUTI 0.845 0.906 0.822* CLABSI 0.457 0.369 0.860* CDI 0.750 0.805 0.924 MRSA 0.799 0.767 0.854 SSI Hyster 0.698 0.710 0.762 SSI Colon 0.751 0.8244 0.783 PSI 90 0.777936 0.577321 0.774058 NHSNFile Size: 2MB