Transcription
Perinatal Oral Health Update:Clinical Guidelines & Best PracticesIrene V. Hilton DDS, MPH, FACDSan Francisco Department Public HealthClinical Instructor, School of Medicine, University of California San FranciscoClinical Instructor, School of Dentistry, University of California San FranciscoOctober 19, 2015Irene.Hilton@sfdph.org
Objectives Understand effect of maternal oral health onfamilies Describe why pregnancy provides opportunityto provide oral health interventions for women Learn elements of clinical prevention andtreatment guidelines for pregnant women
I am comfortable performing a routinesurgical extraction of #30 on a 19 y/owoman with controlled diabetes who is 39weeks pregnant and Rx’ing Tylenol # 3 foranalgesia post-operatively.A. No problemB. I have concerns
Impact of Maternal Oral Healthon FamiliesPeriodontitis &Pregnancy Outcomes
Disease Response toBacterial ighTNFαIL-6IL-1βIFN-gPGE2MMPs
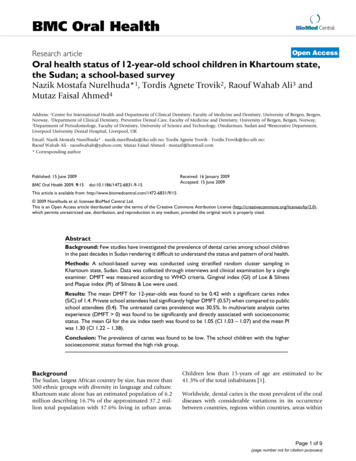
Meta-Analysis of Associations(Matevosyan, 2011) 125 studies between 1998-2010 Maternal periodontal disease remainsassociated with adverse perinataloutcomes (APO)– Preclampsia– Prematurity
Meta-Analysis of ClinicalIntervention Trials Journal American Dental Association– 2010 Dec 141(12): 1423-1434 British Medical Journal– 2010 Dec 29;341:c7017 Journal of Clinical Periodontology– 2011 Oct 38(10):902-14 No effect on adverse birth outcomes
Routine Dental Treatment Safe Intervention studies show routine dentaltreatment of periodontitis is safe duringpregnancy Other routine dental care/proceduresalso safe (Michalowicz et al, 2008)
Microbiome- The Latest The ecological community ofmicroorganisms that share our bodyspace (Lederberg and McCray, 2001) Human body is inhabited by at least 10times more bacteria than the number ofhuman cells
HumanMicrobiomeProjectHHUse new technology to sample andanalyze the genome of microbesfrom five sites on the human bodyDetermine whether there areassociations between changes inthe microbiome and health/ disease5 year projectNIH HMP Working Group et al., "The NIHHuman Microbiome Project.", Genome Res,2009 Oct 9;19(12):2317-23Slides from Kjersti Aagard, Baylor
Microbiome ModelsSlides from Kjersti Aagard, BaylorThe HMP Consortium, Nature (2012). The HMPConsortium, Nature (2012). Aagaard et. al., PLoS One(2012). Aagaard et al., FASEB J (2012), Riehle et al.,BMC Bioinformatics (2012), Ganu et al, Am J Perinatol(2012), Bader & Ganu et al, in preparation (2013), Ma etal., in review FASEB (2013)
Distribution by Body Site GI tract (29%) Oral (26%)– Human oral cavity is estimated to containmore than 750 bacterial species packed inbiofilms (Jenkinson and Lamont, 2005; Paster et al.,2006) Skin (21%) Nasal (14%) Urogenital (9%)NIH HMP Working Group et al. The NIH HumanMicrobiome Project., Genome Res, 2009 Oct 9;19(12):231723
Gram-negative Periodontitis Porphyromonas gingivalis- AD, APO, RAFusiform nucleatum- AD, APO, RA, IBD/CRCTannerella forsythia- AD, APO, RATreponema denticola- APO,Campylobacter rectus- APOPrevotella intermedia- AD, APO, RAPrevotella nigrescens- APOA. actinomycetemcomitans- ADHan YW, Wang X. Mobile microbiome: oralbacteria in extra-oral infections and inflammation.J Dent Res. 2013 Jun;92(6):485-91
Normal Perinatal Progression Normal parturition controlled by inflammatorysignaling Amniotic fluid levels of prostaglandin andinflammatory cytokines rise until inducesrupture of amniotic sac, uterine contraction,dilation and delivery Process can be modified by external stimuliinfection and inflammatory stressors
Etiology of Periodontitis Toxic products from bacteria in gingivalcrevice induce immune-systemmodulated processes that result indestruction of supporting bone An inflammatory process
Periodontitis & PregnancyMechanisms Direct: Periodontal bacteria & toxins cross theplacental barrier colonize feto-placental unit,trigger infection and/or inflammatoryresponse and pregnancy complications Indirect: Inflammatory cytokines andmediators produced at gingival level enterblood circulation and reach the feto-placentalunit and enhance/stimulate inflammatoryresponse (Madianos et al, 2013)
Periodontal Bacteria found inAmniotic Fluid Porphyromonas gingivalisFusiform nucleatumAggregatibacter actinomycetemcomitansBergeyella Periodontal pathogens detected in amniotic/fetoplacental tissues of women with normal pregnancies What factors determine whether translocation ofthese pathogens contributes to pregnancycomplications?
Impact of Maternal Oral Healthon FamiliesDental Caries
Strep Mutans Transmission
MomChild
Early Childhood Caries Disparities% 3-5 y/o Untreated DecayData Source: NHANES, 2009-2010, NCHS/CDC.
Maternal Influence Diet Level of home care Importance of primary teeth & oralhealth Genetic & transmissibility components
Pregnancy Presents anOpportunity Introduce risk reduction & selfmanagement strategies 2 for 1 Stabilize periodontal & caries status Frequent contact with health caredelivery system Higher interest in health May be only time have dental insurancecoverage
Clinical Interventions
Need For GuidelinesDental Providers Insufficient training combined with lackof experience treating pregnant womenin dental school Fear of malpractice suit if somethinggoes wrong with a patient’s pregnancy Concerns about the safety ofprocedures
Malpractice Myth TDIC- ten states & 17,000 insureddentists Reports one claim in the past 15 yearsblaming adverse birth outcome ondental treatment– No evidence for claim
Guidelines Everywhere New YorkCaliforniaWashingtonSouth CarolinaAmerican Academy of PediatricDentistry
2012 National Consensus Statement
2013 ACOG Committee OpinionOral Health Care During Pregnancy andThrough the Lifespan (August 2013)“Oral health is an important component ofgeneral health and should be maintained duringpregnancy.women should be routinelycounseled about the safety and importance oforal health care during pregnancy.’
Guidance for Prenatal Care HealthProfessionals
Role of Perinatal Provider Ask about and assess oral health Facilitate oral health examination byidentifying dental provider Facilitate treatment by providing writtenmedical clearance when indicated Ask if any concerns & address. Informdental care is safe and effective
Role of Dental Provider Deliver comprehensive diagnostic,preventive, restorative, and emergency care Pregnancy not a reason to defer routinedental care or treatment of problems For healthy pregnancies, not necessary tohave approval from the prenatal care providerfor routine dental careCDAF Evidence-based Guidelines, 2010
Pregnancy Gingivitis 80% of women 2nd-8th mo Preexisting gingivitismay predispose topregnancy gingivitisPhoto: Dr. Robert Johnson, Univ of WACDAF Evidence-based Guidelines, 2010
Pregnancy Granuloma(epulis or pregnancy tumor) Occurs in up to 5% ofwomen Single tumor-likegrowth (up to 2 cm) inan area of gingivitis orrecurrent irritation(usually maxillarybuccal anterior) Usually regressesspontaneously afterdeliveryPhoto: Dr. Robert Johnson, Univ of WA
Gastrointestinal: Impact on OralHealth At risk for acid-induced tooth erosionsecondary to vomiting Diet may increase in refinedcarbohydrates, increasing risk for cariesPhoto: Dr. Bea Gandera, Univ of WA
Consult Indicated Co-morbidities that may affect managementdiabetes, pulmonary issues, heart or valvulardisease, hypertension, bleeding disorders, orheparin-treated thrombophilia Nitrous oxide, IV sedation or generalanesthesia needed for dental treatment
Dentist’s Concerns forSurgical Intervention/treatment X-raysLocal anesthesiaMedicationsRestorative materialsNitrous oxidePerception of patient discomfort
Adverse Pregnancy Outcomes Risk of pregnancy loss before 20weeks-15-25%. Most are notpreventable. Risk of teratogenecity-up to 10 weeks.Rate of malformations-3 to 4%.
Is it Safe to Take X-rays? “No single diagnostic procedure resultsin a radiation dose significant enough tothreaten the well-being of thedeveloping embryo and fetus.” American College of Radiology
X-rays Use abdominal and thyroid shields ADA Guidelines-Number needed forcomplete clinical diagnosis (same asnon-pregnant) Image Gently Standard of care
Drugs in PregnancyPhysiological Considerations Changes in pulmonary, gastrointestinaland peripheral blood flow can alter drugabsorption Hepatic changes can alterbiotransformation of drugs by the liverand clearance Benefits vs. Risks “Old standbys” with long track records
Drugs in Pregnancy Study of W. VA pregnant women (Glover etal. 2003)– Average 1.14 prescription drugs, excludingvitamins and iron– Average of 2.95 over-the-counter drugs Tylenol, Tums, cough drops– Nearly half (45%) used herbal agents Peppermint, cranberry
FDA ClassificationA - controlled studies in humans havedemonstrated no fetal risks– very few such drugs - prenatal vitaminsB - animal studies indicate no fetal risksbut no human studies OR adverseeffects in animals but no well controlledhuman studies– PCN, cephalosporins, metronidazole,lidocaine, acetaminophen, CHX
FDA ClassificationC - no adequate studies either human or animalOR adverse fetal effects in animals but nohuman data– codeine, morphine, meperidine, beta blockers,heparin, acyclovir, indomethicin, naproxenD – evidence fetal risk but benefits outweigh risk– phenobarbital, phenytoin, valproic acid, lithiumX - proven fetal risk too great– isotretinoin and thalidomide
Local Anesthesia Standard lido w/ epi- Category B Articaine & mepivacaine- Category C Default to “old standbys”
Drugs in Pregnancy-Avoid NSAIDS (1st & 3rd)Erythromycin estolateTetracyclineAspirin (3rd)
Restorative Materials Amalgam– No evidence harmful effect in populationstudies and reviews (FDA 2009, CDC, NCI)– No additional risk if standard safe amalgampractices are used Resins– Short-term exposure associated withplacement has not been shown to havehealth risk; data lacking on effects of longterm exposures
Patient Comfort Head higher thanfeet Upper archtreatment early inpregnancy beforelower arch Morning orafternoonappointmentpreference Breaks
Supine Hypotensive SyndromeSymptoms:Signs: Drop in bloodpressure Bradycardia Possible loss ofconsciousnessSweatingNauseaWeaknessSense of lack of air
Postural Considerations IVC/aorticimpingement byweight of fetus 15-20% ofpregnancies Can start in 2nd butmax in 3rd trimester Turn on side torestore circulation
Self Management
Fluoride
Chlorhexidine Suppress s. mutans & periodontal pathogensNon-alcohol formulationPatients rinse prior to appointmentAfter birth- 1 week of CHX followed by 3weeks of OTC Fl rinse (Spolsky et al. CDA Journal 2007) Cost/insurance coverage
Patient Education Materials Literacy level Cultural appropriateness Keep materials brief Focus on how Mother’soral health affects baby
Conclusion Pregnant women are experiencing anormal biological state and ethicallydeserve the same level of care as anyother patient Evidence base shows appropriatedental care is necessary and safe
Our Goal
Malpractice Myth TDIC- ten states & 17,000 insured dentists Reports one claim in the past 15 years blaming adverse birth outcome on dental treatment . Cost/insurance coverage . Patient Education Materials Liter