Transcription
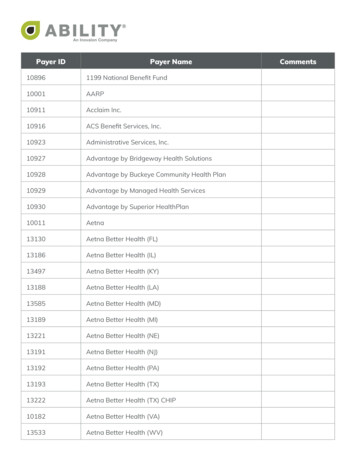
Health Plan/Payer List Availity Clearinghouse and Web PortalUpdated 10/07/2014AvailityP.O. Box 550857Jacksonville, FL 32255-0857
Health Plan/Payer ListAvaility Clearinghouse and Web PortalTable of ContentsNavigating the EDI Clearinghouse Health Plan Partners Section . . 3Availity’s NPI Options . .4Availity’s Electronic Data Interchange (EDI) Health Plans Partners. . . . .5 – 32Availity’s Electronic Remittance Advice (ERA) Health Plan Partners. .33 - 49Availity’s Business to Business (B2B) Health Plan Partners. 50Availity’s Web Portal Health Plan Partners. . . 51 – 54Workers’ Compensation Payer List . . .55 - 1382 of 138Visit our web site: www.availity.com
Health Plan/Payer ListAvaility Clearinghouse and Web PortalNavigating the EDI Clearinghouse Health Plan Partners SectionClaim Enrollment Required: Denotes payers that require enrollment for EDI claims submission (837P/I). See EDI Requirements for enrollment details.Government Payer: Denotes Government payers. May not be a direct connection to the government entity.Remit (835): Electronic remittance advice sent by payers to communicate adjudication results and payment information for submitted claims. Receiving remits generally requires additional enrollment. Please enroll with Availity first. Please see the Electronic Remittance Advice (ERA) Health Plan Partners section of the list for registration details.NPI Option: The NPI is a unique identification number for covered health care providers. Availity is making every effort to confirm and communicate the status of our connected payers. For a detailed explanation of our NPI options please see page 4 of this document.(EDI) Electronic Data Interchange: Customers create batch transactions in their own practice management system (PMS) or hospital information system (HIS) and upload them to Availity. This functionality can be transparent to the end user if their system vendor offers a seamless solution. Availity also offers end users the ability to log onto the portal to upload batches directly. A list of vendor partners is available on the Availity web site.(B2B) Business to Business: Customers submit transactions in real-time or near real-time using their own practice management system (PMS) or hospital information system (HIS),often using the vendor’s user interface. A list of vendors that support this level of integration is available on the Availity web site. Please see Availity's B2B specification document for additional information.Premium ( ):The “ ” in the Premium column indicates that the payer requires enrollment in Availity Advanced Clearinghouse if the provider is based in Texas. Please click thelink for more information: f9mqcevwphcu/?name AAC Provider FAQ - TX.pdf3 of 138Visit our web site: www.availity.com
Health Plan/Payer ListAvaility Clearinghouse and Web PortalAvaility’s NPI OptionsOption 1Option 2Option 3Legacy ID RequiredDual IDNPI per MandateNPI allowedLegacy identifier required Allows all of the following scenarios: NPI only Legacy identifier only NPI and Legacy identifiersNPI required as Primary Identifier.Tax ID required as a secondary identifier on claims in 2010AA or 2010AB.Only specific non-Legacy qualifiers allowed as secondary identifiers in certainprovider loops. 4 Option 3 plus: Any other secondary identifiers as allowed in the Implementation Guide will also beaccepted.Option 4NPI per Mandate. Legacy ID alsoallowed.4* Option 3 plus: Tax IDs (EI, SY, TJ) as allowed in the Implementation Guide will also be acceptedas secondary identifiers.#4 Option 3 plus: Location Numbers (LU) as allowed in the Implementation Guide will also beaccepted as secondary identifiers.*A legacy identifier is any identifier that payers used to identify a provider as a health care provider before the NPI mandate. Legacy identifiersinclude OSCAR, NSC, PINs, UPINs, Blue Cross provider numbers, and other payer-designated identifiers.( ) Indicates the payer has requested a front-end taxonomy code edit.4 of 138Visit our web site: www.availity.com
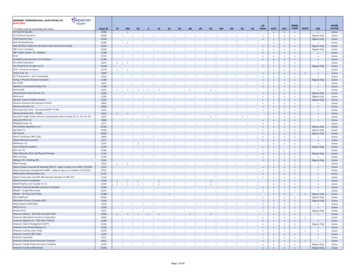
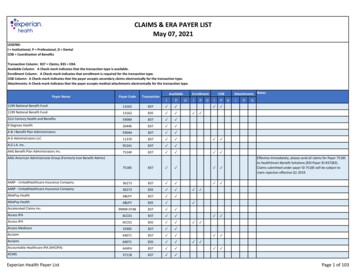
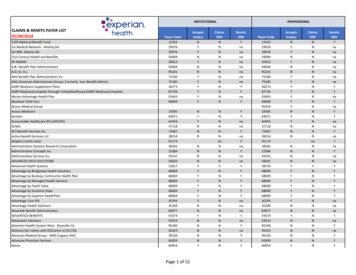
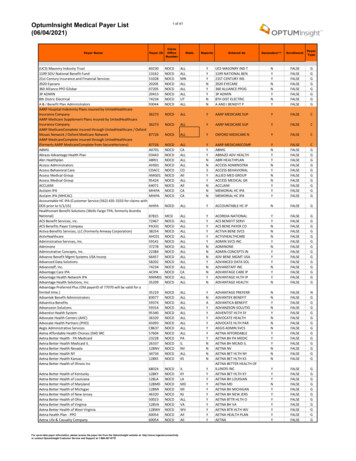
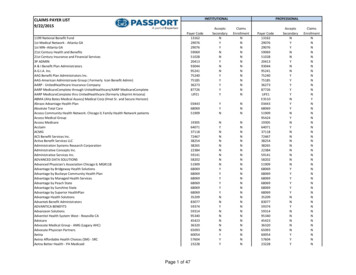
NPI OptionPayer NameRemit (835)Payer IDClaim Enroll RequiredPremiumGovernment Payer*Availity's Electronic Data Interchange (EDI) Health Plan PartnersProfessionalClaim (837)InstitutionalClaim 209770705937425133953406509336320650931199 NATIONAL BENEFIT FUNDA & I BENEFIT PLAN ADMINISTRATORSABC HEALTH PLANABSOLUTE TOTAL CAREACCESS ADMINISTRATORACCLAIMACMGACORDIA NATIONALACS CONSULTING SERVICES, INCACTIVA BENEFIT SERVICES, LLCACTIVE CARE (UCS)ADMINISTRATIVE CONCEPTS, INCADMINISTRATIVE SERVICESADMINISTRATIVE SYSTEMS RESEARCH CORPORATION - ASRADMINONEADVANCED DATA SOLUTIONS, INCADVANCED PHYSICIAN ASSN. (CHICAGO)ADVANTAGE HEALTH SOLUTIONADVANTAGE PREFERRED PLUSADVANTICAADVANTRA/HLTH AMERICA INCADVENTIST HEALTH SYSTEM WEST - ROSEVILLE, CAADVOCATE HEALTH PARTNERSADVOCATE MEDICAL GROUPADVOCATE PHYSICIAN PARTNERS 26337AETNA - ILLINOIS MEDICAID2xx 60054AETNA AFFORDABLE HEALTH CHOICES (SM) - SRC2xx 23225AETNA BETTER HEALTH CONNECTICUT MEDICAID2xx50023AETNA BETTER HEALTH OF OHIO2xx 60054AETNA INSURANCE COMPANY2xx 38692AETNA TX MEDICAID & CHIP2xx13334AFFINITY HEALTH xxxxxxxx2xx13550AFTRA HEALTH FUNDAGENCY SERVICES, INC.ALAMEDA ALLIANCE FOR HEALTHALASKA CHILDREN’S SERVICES, INC.ALASKA ELECTRICAL HEALTH & WELFARE FUNDALASKA LABORERS CONSTRUCTION INDUSTRY TRUSTALASKA PIPE TRADERS LOCAL 375ALASKA UNITED FOOD & COMMERCIAL WORKERS HEALTH & WELFARETRUSTALICARE2xxPRINTALL HEALTH PLAN PRINT (PRINT TO 5261A070125133AMAIA13550680696806968069ALLCARE HEALTH PLANALLEGIANCE BENEFIT PLANALLIANCE - ALPHA CARE GOLDALLIANCE HEALTHPLANS OF WISCONSINALLIANCE PPO, INC.ALLIANT HEALTH PLANS (GEORGIA)ALLIED ADMINISTRATORS (S.F., CA)ALLIED BENEFITS SYSTEMSALPHA DATA SYSTEMSALTA BATES MEDICAL GROUPALTA HEALTH STRATEGIESAMA INSURANCE AGENCYAMALGAMATED LIFEAMBETTER FROM BUCKEYE COMMUNITY HEALTH PLANAMBETTER FROM COORDINATED CAREAMBETTER FROM CELTICARE HEALTH xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxEligibility &Benefits(270)ClaimStatus(276)Auth &Referral(278)Additional Informationpayer ID 68055 may also be usedformerly Advocate Health CentersEDI submitters located in the IL, NM, OK, OR, TX, and WA regions require Advanced Clearinghouseenrollment for this payer. Please contact your practice management vendor oradvancedclearinghouse@availity.com for further details.EDI submitters located in the IL, NM, OK, OR, TX, and WA regions require Advanced Clearinghouseenrollment for this payer. Please contact your practice management vendor oradvancedclearinghouse@availity.com for further details.EDI submitters located in the IL, NM, OK, OR, TX, and WA regions require Advanced Clearinghouseenrollment for this payer. Please contact your practice management vendor oradvancedclearinghouse@availity.com for further details.EDI submitters located in the IL, NM, OK, OR, TX, and WA regions require Advanced Clearinghouseenrollment for this payer. Please contact your practice management vendor oradvancedclearinghouse@availity.com for further details.EDI submitters located in the IL, NM, OK, OR, TX, and WA regions require Advanced Clearinghouseenrollment for this payer. Please contact your practice management vendor oradvancedclearinghouse@availity.com for further details.When submitting to this payer ID please ensure the following: The claim is for a Medicaid, Child HealthPlus, or Family Health Plus member and the subscriber ID is as printed on Member's ID CardPlease contact Anet Quiambao at 510.747.6153 to join Alameda Alliance's EDI networkTo enroll for All Health Plan Print (Print To Paper), please complete and submit the APP SubmitterInformation and Enrollment Packet. Please note that claims cannot be converted to paper for payerswith the state code of SC or MN.APP Submitter Information and Enrollment PacketEffective 8/1/2012, formerly known as Mid Rogue Oregon Health Plan
NPI r NameRemit (835)Payer IDClaim Enroll RequiredPremiumGovernment Payer*Availity's Electronic Data Interchange (EDI) Health Plan PartnersProfessionalClaim (837)InstitutionalClaim 6323037222487996653085AMBETTER FROM MAGNOLIA HEALTHAMBETTER FROM MANAGED HEALTH SERVICESAMBETTER FROM PEACH STATE HEALTH PLANAMBETTER FROM SUNSHINE HEALTHAMBETTER FROM SUPERIOR HEALTHAMBETTER OF ARKANSASAMERIBEN SOLUTIONS, INC.AMERICAN ADMINISTRATIVE GROUP - AAGAMERICAN ADMINISTRATIVE GROUP - AAG (FORMERLY GALLAGHERBENEFITS)AMERICAN BEHAVIORALAMERICAN BENEFIT PLAN ADMINISTRATORSAMERICAN CHIROPRACTIC NETWORKAMERICAN CHIROPRACTIC NETWORK (PAN)AMERICAN CHIROPRACTIC NETWORK IPA OF N.Y.AMERICAN COMMERCIAL BARGE LINESAMERICAN FAMILY INSURANCE CO.AMERICAN FIDELITY ASSURANCE COMPANYAMERICAN FOUNDERS LIFE INSURANCE CO.AMERICAN GENERALAMERICAN HEALTHCARE ALLIANCEAMERICAN IMAGING MANAGEMENTAMERICAN INSURANCE COMPANY OF TEXASAMERICAN LIFECAREAMERICAN NATIONAL INSURANCE COAMERICAN POSTAL WORKERS UNIONAMERICAN REPUBLICAMERICAN REPUBLIC INSURANCEAMERICAN WORKER HEALTH PLUSAMERICA'S 1ST CHOICE - SOUTH CAROLINAAMERICA'S CHOICE HEALTHPLANS/NMAAMERICA'S PPO (ARAZ)AMERICHOICE OF NEW JERSEY (MEDICAID NJ)AMERICHOICE OF NEW JERSEY PERSONAL CARE PLUS (MEDICARE)AMERICHOICE OF NEW YORK (MEDICAID NY)AMERICHOICE OF NEW YORK PERSONAL CARE PLUS (MEDICARE)AMERICHOICE OF PENNSYLVANIA MEDICAID/CHIPAMERICHOICE OF PENNSYLVANIA PERSONAL CARE PLUS (MEDICARE)AMERIGROUPAMERIHEALTH ADMINISTRATORSAMERIHEALTH HMO NEW JERSEY AND DELAWAREAMERIHEALTH MERCY HEALTH PLANAMIDA CAREANCHOR BENEFIT CONSULTING, INC86062ANCILLARY BENEFIT SYSTEMS/ARIZONA FOUNDATION FOR MEDICAL CARE2xx47198ANTHEM CA3xx00050ANTHEM CO3xx00060ANTHEM CT3x00130ANTHEM IN300630ANTHEM IN300160ANTHEM KY300660ANTHEM KY337283xClaimStatus(276)Auth &Referral(278)Additional ty &Benefits(270)This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).
NPI OptionPayer NameRemit (835)Payer IDClaim Enroll RequiredPremiumGovernment Payer*Availity's Electronic Data Interchange (EDI) Health Plan PartnersProfessionalClaim (837)00180ANTHEM ME300680ANTHEM ME3x00241ANTHEM MO3x00270ANTHEM NH300770ANTHEM NH3x00265ANTHEM NV3x00332ANTHEM OH300834ANTHEM OH3x00423ANTHEM VA3x00450ANTHEM WI300950ANTHEM SRM1ATPA13632639065APEX BENEFIT SERVICESAPS HEALTHCARE, INC.ARCADIAN MGMT SERVICESARIZONA FOUNDATION FOR MEDICAL CAREARIZONA PHYSICIANS IPAARIZONA PRIORITY CARE PLUSARKANSAS BEST CORPORATION - CHOICE BENEFITSARKANSAS MANAGED CARE ORG (AMCO)ARNETT HEALTH PLANSASRM CORP (NJ)ASSOCIATED THIRD PARTY ADMINISTRATIONASSOCIATES FOR HEALTH CARE, INCASSURANT HEALTH2242222224222xxxxxxxxxxxxxASNTHASSURANT HEALTH RE-PRICING VIA 59372809113646045592755927465026SX145ASSURED BENEFITS ADMINISTRATORSASURIS NORTHWEST HEALTHATHENS AREA HEALTH PLANATLANTIS HEALTH PLANATLAS LIFE INSURANCE COMPANYATRIO HEALTH PLANAUSTIN REGIONAL CLINIC EMPLOYEE BENEFIT PLANAUTOMATED BENEFIT SERVICES (ABS)AUTOMATED GROUP ADMINISTRATION, INC.AUTOMOTIVE MACHINISTS LOCAL 289 HEALTH & WELFARE FUNDAVERA HEALTHAVMED ENCOUNTERSAVMED, INC.BAPTIST HEALTH SOUTH FLORIDABANNER HEALTH aim (837)Eligibility &Benefits(270)ClaimStatus(276)Auth &Referral(278)This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).This payer accepts EDI batch claims via the Availity portal only. To do so, log in to the Availity portal(www.availity.com), and then click EDI File Management Send and Receive EDI Files. After selectingyour organization, click SendFiles. For further assistance, click Help at the top of the portal page orcontact Availity Client Services (1.800.282.4548).xxxxxxxxxxxxxxxxxUse payer ID ASNTH to submit professional or institutional Assurant Health claims to be routed forHealthSpan Re-Pricing. Use existing Payer IDs for claims for Assurant Health lines of business withoutre-pricing.xxxxxxxxxxEffective 8/20/12, payer ID 95440 will no longer be valid. Please use payer ID 87726.xxxxAdditional Informationxx
Remit (835)NPI Option Claim Enroll RequiredPremiumGovernment Payer*Availity's Electronic Data Interchange (EDI) Health Plan PartnersProfessionalClaim (837)4120406941491534332495377BASIC PLUSBAY BRIDGE ADMINISTRATORS LLCBCI ADMINISTRATORS, INC.BEACON HEALTH STRATEGIESBEECH STREET CORPORATION22222xxxxxxxxxx60054BELL 137308BENEFIT ADMINISTRATIVE SERVICES (BAS)BENEFIT ADMINISTRATIVE SYSTEMSBENEFIT CONCEPTSBENEFIT COORDINATORS CORPORATION (PITTSBURGH, PA)BENEFIT MANAGEMENT SERVICES (BMS)BENEFIT MANAGEMENT SYSTEMS,INCBENEFIT PLAN ADMINISTRATORS (ROANOKE, VA)BENEFIT PLAN ADMINISTRATORS, CO (EAU CLAIRE, WI)BENEFIT PLANNERS, INC.BENEFIT SYSTEMS & SERVICES, INC (BSSI)BENEFIT TRUST LIFEBEST LIFE & HEALTH INSURANCE CO.BETTER HEALTH OF FLORIDABETTER HEALTH PLANS, INC.BIENVIVIR SENIOR HEALTH PLANBIG LOTS ASSOCIATES BENEFIT PLANSBLOCK VISION OF TEXASBLOCK VISION, INCBLUE BELL BENEFITS xxxxxxx00610BLUECROSS (BC) IDx2x00520BLUECROSS BLUESHIELD (BCBS) ARx4 x53589BLUECROSS BLUESHIELD (BCBS) AZ4*x00101BLUECROSS BLUESHIELD (BCBS) GA300601BLUECROSS BLUESHIELD (BCBS) GA00621BLUECROSS BLUESHIELD (BCBS)
Updated 10/07/2014. Availity. P.O. Box 550857. Jacksonville, FL 32255-0857. Health Plan/