Transcription
2021 VIRTUALCONFERENCEWhat EVERY Therapist Should KnowInsurance and Telehealth BillingwithBarbara Griswold, LMFTAuthor, Navigating the InsuranceMaze: The Therapist’s CompleteGuide to Working With Insurance-And Whether You ShouldWe will go fast! Follow-up questions?May 15, 2021theinsurancemaze.com/CAMFTCase ExampleYour om2A Diagnosis From the DSM-5Oldcode Use ICD-10 codes Get DSM-5 for diagnostic criteria But came out in 2013 -- someICD-10codediagnosis codes out of date! Why you should use icd10data.comtheinsurancemaze.com3
StartingTherapywithDorothy Why – if you are a network provider -- youshould call the plan NOW Not calling first may be provider’s biggestmistaketheinsurancemaze.com6
Don’t Get Burned!Barb’s 3 Axioms of Healthy Distrust1. Don’t trust Dorothy’s insurance card2. Don’t trust her plan’s website3. Don’t trust Dorothy You need to ask morequestions, get moreinfo Tip: Submit claimsearly and oftentheinsurancemaze.com7To Get Paid, YouDon’t Need MagicRuby SlippersGet my worksheet“Checking Coverage:12 Essential Questions”to check coverage for office visits and telehealthat theinsurancemaze.com/CAMFTBonus: “11 Progress Notes Requirements”8Behind the Curtain: What CoverageMight Dorothy Have?Employee AssistanceProgram (EAP) Employer benefit foremployees and family Usually limited FREE sessions Ct. must get preauthorizationand see a network therapist What’s great about EAPtheinsurancemaze.com9
What Coverage Might Dorothy Have?HMO or EPO: Health Maintenance Organization or ExclusiveProvider Organization Only cover network providersPPO or POS: Preferred Provider Organization or Point ofService Plan Covers both in- and out of network (OON), but Dorothypays more if goes OON Plans may cap reimbursement for OON providers, i.e.Allowed Amount/UCR (Usual, Customary, Reasonable Fee)theinsurancemaze.com10Your ChoicesNetwork Provider Sign panel contract Pro: Get referrals from plan Con: Must submit claims, acceptdiscountrate (varies by plan, CPT code,location, license)Out-of-Network (OON) Any therapist who did not sign a contract Pro: Can collect full fee (or slide fee) Con: no plan referrals, lose clients seeking networktherapist to lower their costs Ct pays you, you give superbill to client to submit to plan, ifhas OON benefitstheinsurancemaze.com11Don’t Let Dorothy Run Away:How You Can Keep Her(Even if You Are Not on Her Plan) Offer to contact the planUsing Checking CoverageHandout -- or at least urgeher to call -- if she has PPOor POS plan, to investigateOON coverage Single Case Agreementstheinsurancemaze.com12
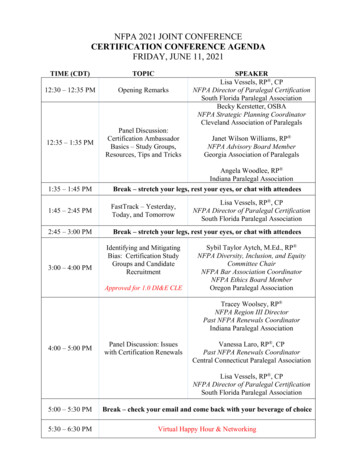
Joining Networks:Steps to Follow It takes time to join Go to plan websites andcall plans? Full? No such thing Send plan an “insuranceresume” and cover letter;what makes you stand out? For California folks: purchasemailing labels for 60 CA insurance plans/EAPs Choosing CPT Codes90791: diagnostic assessment/evaluation (first session)90832: individual therapy 30 min (16 – 37 mins)90834: individual therapy 45 min (38 – 52 mins)90837: individual therapy, 60 min (53 mins) Indiv. codes can include occasional “informants” Don’t use for ongoing couples/family work Client must be present for most/all of session90846: couples/family w/o client, 50 min (26 min)90847: couples/family therapy, 50 min (26 min)Video/phone: Usually add modifier 95 (GT maybe accepted); use Place of Service Code 0214Choosing CPT codes:You Don’t Need ToBe a Wizard Document actual (not scheduled) startand stop times in notes!!! (why?) Countonly therapy time, not waiting, scheduling, documenting Are sessions longer than 60 min. covered? See: theinsurancemaze.com/extendedsessions Avoid 90837 with United Behavioral Health/UHC/OPTUM For more info on CPT codes: Webinar -- “CPT Coding Tips:Maximize Reimbursement and Prevent Denials”theinsurancemaze.com15
Is Couples/Family Therapy Covered? Most plans cover if there’s a clientwith diagnosis (not Z-code only) Systems therapy approach fine Tip: When call plan, don’t ask ifcouples/family counseling covered-- ask if CPT 90847 is covered Check out my new webinar:“Couples Therapy: Billing,Documentation, and EthicalDilemmas”theinsurancemaze.com1616Will Sessions Be Limited?Usually not. Most clients have unlimitedsessions regardless of diagnosis BUT: Plans can still refuse to covervisits they feel are not “medicallynecessary” “Medical necessity reviews” used to limit sessions or notreimburse, even for out-of-network therapists Treatment plan and notes must address need for treatment See today’s freebie “11 Progress Notes Requirements” attheinsurancemaze.com/CAMFT See my Progress Notes webinar, Treatment Plan webinartheinsurancemaze.com17What Plans Look For: “Medical Necessity” DSM diagnosis more than a Z-code Adjustment Disorder usually covered Treatment seen as necessary, not just desired / supportive Treatment goals can’t be just personal growth, self-esteem,feeling awareness, sexual issues, career growth, bettercommunication/relationships, improved life satisfaction Symptoms impair work/school, relationships, health/sleep, Therapy goals: Mental health symptom reduction, reducingimpairmentSo: Can’t bill insurance if not “medically necessary”theinsurancemaze.com18
New Trend: Plans Are Knocking 79% of therapists reported records request/treatment reviewRemember: They are not YOUR Notes1. Administrative Records Requesta. Documentation Reviewb. Risk Adjustment/ACA(ex. Ciox, Inovalon, Datafied)2. Billing-Related3. Treatment Reviews (Clinical) Usually phoneIf you get a call from a plan, contact me or CAMFT!theinsurancemaze.com19Telehealth: Will PlansKeep Covering It? Vary by health plan/client account Need to keep checking Some plans basing expansion ofcoverage on U.S. Public HealthEmergency declaration, scheduled to expire July 19th, likely willbe extended until end of December 2021 (tinyurl.com/PHEapril) Many plans likely to stop covering phone Some have stopped covering out-of-network providers Some plans may insist you use their designated telehealthplatform/group (ex. Teledoc) to be reimbursed20Out-of-State Therapy Generally, must be licensed in statewhere client is at time of the session,unless you have permission from thatother state’s licensing board Client residence doesn’t matter Contact that state’s board to check rules: See CAMFT list MFT State LicensingBoards: https://tinyurl.com/StateBoards If YOU left the state, usually not an issue Also, contact malpractice carriertheinsurancemaze.com21
Questions?Visittheinsurancemaze.com/CAMFT Get handout: “Checking Coverage:12 Essential Questions” Get handout: “11 Progress NotesRequirements” Sign up for my email news Learn about other live & recordedclasses / CE and Legal & Ethicalcourses / Resourcestheinsurancemaze.com22Let Me Be Your Good Witch!Schedule a consultation atcalendly.com/barbgrisaround insurance, documentation,and practice-building questionsBarbara Griswold, LMFTPrivate Practice Coachingtheinsurancemaze.combarbgris@aol.com 408-985-084623
Insurance and Telehealth Billing CONFERENCE with Barbara Griswold, LMFT . If you get a call from a plan, contact me or CAMFT! 19 theinsurancemaze.com Telehealth: Will Plans Keep Covering It? . Also, contact malpractic