Transcription
Health Insurance Exchange2020 Quality Rating SystemMeasure Technical SpecificationsSeptember 2019
THIS PAGE LEFT INTENTIONALLY BLANK.
Technical Assistance and Contact InformationTechnical Assistance and Contact InformationThe following links and contact information should be used to obtain additional details and technicalassistance related to the Quality Rating System (QRS) measure set for 2020.Website Links Centers for Medicare & Medicaid Services (CMS) Health Insurance Marketplace Quality Initiativeswebsite: es.html National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and InformationSet (HEDIS ) 1 Compliance AuditTM DISComplianceAuditProgram.aspxContact Information1 For questions regarding the QRS clinical measure specifications, please contact the appropriatemeasure steward:o NCQA for the HEDIS measures: via My.NCQA available at https://my.ncqa.orgo Pharmacy Quality Alliance (PQA) for the PQA measures: https://www.pqaalliance.org/QRS For questions regarding QRS survey measures, the QHP Enrollee Survey, or QRS requirements,please contact the Marketplace Service Desk (MSD) via email at CMS FEPS@cms.hhs.gov orvia phone at 1-855-CMS-1515 (1-855-267-1515). Reference the “Marketplace Quality Initiative(MQI)-QRS”.HEDIS is a registered trademark of the National Committee for Quality Assurance.i
THIS PAGE LEFT INTENTIONALLY BLANK.
Table of ContentsTable of Contents1Introduction .12QRS Measure Set .53QRS Clinical Measure Specifications .93.1 NCQA Measure Specifications .93.2 PQA Measure Specifications .1914QRS Survey Measure Specifications .203iii
THIS PAGE LEFT INTENTIONALLY BLANK.
1. Introduction1
THIS PAGE LEFT INTENTIONALLY BLANK.
1. IntroductionIntroductionDocument PurposeThis document includes the measure specifications and guidelines for data collection for the 2020 QualityRating System (QRS) measure set. Qualified Health Plan (QHP) issuers will need to reference this documentin order to collect and submit QRS measure data to the Centers for Medicare & Medicaid Services (CMS) inaccordance with the QRS 2020 requirements. The document specifically details the following: QRS measure set. This section includes a list of the QRS measures and a brief background on theQRS measure set. The QRS measure set is comprised of clinical quality measures, including theNational Committee for Quality Assurance (NCQA) Healthcare Effectiveness Information and DataSet (HEDIS) measures and Pharmacy Quality Alliance (PQA) measures. The measure set alsoincludes survey measures based on questions from the Qualified Health Plan Enrollee ExperienceSurvey (QHP Enrollee Survey). QRS clinical measure technical specifications. This section includes measure specifications and datacollection guidelines for NCQA’s HEDIS measures and the PQA measures in the QRS measure set.For the PQA measures, QHP issuers should refer to NCQA’s “General Guidelines for Data Collection”(see Section 3.1 for guidance related to data collection protocols, with the exception of a fewguidelines specific to the PQA measures as noted in Section 3.2). QRS survey measure technical specifications. This section includes descriptions for the surveymeasures in the QRS measure set that will be collected as part of the QHP Enrollee Survey.CMS anticipates updating this document on an annual basis to reflect any changes to the measure set,including changes to the measure specifications or data collection guidelines.BackgroundIn accordance with the requirements specified in the Quality Rating System and Qualified Health PlanEnrollee Experience Survey: Technical Guidance for 2020, QHP issuers that offered coverage through aHealth Insurance Exchange (Exchange) in the prior year are required to submit third-party validated QRSclinical measure data and QHP Enrollee Survey response data to CMS as a condition of certification. 2 CMSwill calculate the quality performance ratings for QHPs offered through all Exchanges, regardless of theExchange model. CMS will apply the QRS rating methodology to validated QRS clinical measure data and asubset of the QHP Enrollee Survey response data (QRS survey measures) to produce quality ratings on a 5star rating scale. 3 CMS will collect data and calculate quality ratings for each QHP issuer’s product type (e.g.,health maintenance organization [HMO]) within each state and apply these ratings to each product type’sQHPs in that State.245 CFR § 156.200(b)(5)(h); § 156.1120; and § 156.1125.The QHP Enrollee Survey includes a core question set that will be used to assess enrollee experience with health careservices. Specific questions are grouped to form survey measures that will be used in the QRS.33
THIS PAGE LEFT INTENTIONALLY BLANK.
2. QRS Measure Set5
THIS PAGE LEFT INTENTIONALLY BLANK.
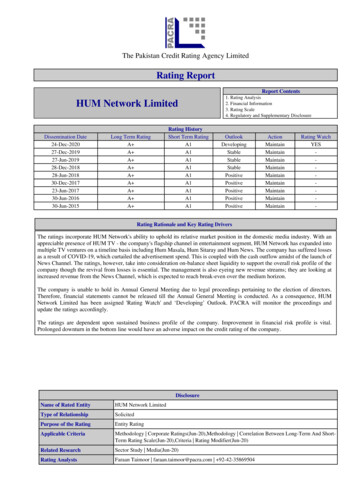
2. QRS Measure SetQRS Measure SetThe QRS measure set consists of measures that address areas of clinical quality management; enrolleeexperience; and plan efficiency, affordability, and management. Exhibit 1 includes the list of QRS measuresrequired for 2020.The measure set includes a subset of NCQA’s HEDIS measures and PQA measures. The survey measuresin the QRS measure set will be collected as part of the QHP Enrollee Survey, which is largely based on itemsfrom the Consumer Assessment of Healthcare Providers and Systems 4 (CAHPS ) surveys. For a crosswalkthat maps each QRS survey measure to the relevant QHP Enrollee Survey item(s), refer to QRS and QHPEnrollee Survey: Technical Guidance for 2020.Some measures have multiple indicators (or rates). QHP issuers are required to collect and submit validateddata for every indicator associated with a measure, unless a specific indicator is shown in parentheses next tothe measure, in which case only the indicator must be reported (e.g., for Childhood Immunization Status[Combination 3], only Combination 3 must be reported).Exhibit 1. 2020 QRS MeasuresMeasureStewardNational QualityForum (NQF) ID 5Adult BMI AssessmentNCQAN/AAnnual Dental VisitNCQA1388Antidepressant Medication ManagementNCQA0105Appropriate Testing for PharyngitisNCQA0002Appropriate Treatment for Upper Respiratory InfectionNCQA0069Avoidance of Antibiotic Treatment for Acute Bronchitis/BronchiolitisNCQA0058Breast Cancer ScreeningNCQA2372Cervical Cancer ScreeningNCQA0032Childhood Immunization Status (Combination 3)NCQA0038Chlamydia Screening in WomenNCQA0033Colorectal Cancer ScreeningNCQA0034Comprehensive Diabetes Care: Eye Exam (Retinal) PerformedNCQA0055Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control ( 8.0%)NCQA0575Comprehensive Diabetes Care: Medical Attention for NephropathyNCQA0062Controlling High Blood PressureNCQA0018Follow-Up After Hospitalization for Mental Illness (7-Day Follow-Up)NCQA0576Immunizations for Adolescents (Combination 2)NCQA1407Initiation and Engagement of Alcohol and Other Drug Dependence TreatmentNCQA0004Measure TitleQRS Clinical MeasuresInternational Normalized Ratio Monitoring for Individuals on WarfarinPQA0555Medication Management for People With Asthma (75% of Treatment Period)NCQA1799Plan All-Cause ReadmissionsNCQA1768Prenatal and Postpartum CareNCQA1517PQA0541Proportion of Days Covered4CAHPS is a registered trademark of the Agency for Healthcare Research and Quality. The surveys are available athttps://cahps.ahrq.gov.5 Definitions of NQF-endorsed measures can be found here: http://www.qualityforum.org/Home.aspx
2. QRS Measure SetMeasureStewardNational QualityForum (NQF) ID 5Use of Imaging Studies for Low Back PainNCQA0052Weight Assessment and Counseling for Nutrition and Physical Activity for Children andAdolescentsNCQA0024Well-Child Visits in the First 15 Months of Life (6 or More Visits)NCQA1392Well-Child Visits in the Third, Fourth, Fifth, and Sixth Years of LifeNCQA1516Access to CareAHRQ, CMS0006Access to InformationAHRQ, CMS0007Care CoordinationMeasure TitleQRS Survey MeasuresAHRQ, CMS0006Flu Vaccinations for Adults Ages 18-64NCQA0039Medical Assistance With Smoking and Tobacco Use CessationNCQA0027Plan AdministrationAHRQ,CMS 60006Rating of All Health CareAHRQ00067Rating of Health PlanAHRQ00067Rating of Personal DoctorAHRQ00067Rating of SpecialistAHRQ000676 Measureconsists of CAHPS survey items and a survey item developed for purposes of the QHP Enrollee Survey.8
3. QRS Clinical Measure Specifications3.1 NCQA Measure Specifications3.2 PQA Measure Specifications9
THIS PAGE LEFT INTENTIONALLY BLANK.
2020 HEDIS General Guidelinesfor the QRS MeasureTechnical Specifications11
HEDIS is a registered trademark of the National Committee for Quality Assurance (“NCQA”). The HEDIS measures andspecifications were developed by and are owned by NCQA. NCQA holds a copyright in these materials and may rescindor alter these materials at any time. Users of the HEDIS measures and specifications shall not have the right to alter,enhance or otherwise modify the HEDIS measures and specifications, and shall not disassemble, recompile or reverseengineer the HEDIS measures and specifications. Anyone desiring to use or reproduce the materials, subject to licenseduser restrictions, without modification for an internal non-commercial purpose may do so without obtaining any approvalfrom NCQA. Use of the Rules for Allowable Adjustments of HEDIS to make permitted adjustments of the materials doesnot constitute a modification. All other uses, including a commercial use, or any external reproduction, distribution andpublication must be approved by NCQA and are subject to a license at the discretion of NCQA.HEDIS measures and specifications are not clinical guidelines, do not establish a standard of medical care and have notbeen tested for all potential applications. The measures and specifications are provided “as is” without warranty of anykind. NCQA makes no representations, warranties or endorsements about the quality of any product, test or protocolidentified as numerator compliant or otherwise identified as meeting the requirements of a HEDIS measure orspecification. NCQA also makes no representations, warranties or endorsements about the quality of any organization orclinician who uses or reports performance measures. NCQA has no liability to anyone who relies on HEDIS measures andspecifications or data reflective of performance under such measures and specifications.A calculated measure result (a “rate”) from a HEDIS measure that has been certified via NCQA’s Measure CertificationProgramSM, and is based on unadjusted HEDIS specifications, may not be called a “Health Plan HEDIS rate” until it isaudited and designated reportable by an NCQA-Certified HEDIS Compliance Auditor. Until such time, applicable measurerates produced by [Product] shall be designated or referred to as “Unaudited Health Plan HEDIS Rates.”Limited proprietary coding is contained in the measure specifications for convenience. Users of the proprietary code setsshould obtain all necessary licenses from the owners of these code sets. NCQA disclaims all liability for use or accuracyof any coding contained in the specifications.The American Medical Association holds a copyright to the CPT codes contained in the measure specifications.The American Hospital Association holds a copyright to the Uniform Billing Codes (“UB”) contained in the measurespecifications. The UB Codes in the HEDIS specifications are included with the permission of the AHA. The UB Codescontained in the HEDIS specifications may be used by health plans and other health care delivery organizations for thepurpose of calculating and reporting HEDIS measure results or using HEDIS measure results for their internal qualityimprovement purposes. All other uses of the UB Codes require a license from the AHA. Anyone desiring to use the UBCodes in a commercial Product(s) to generate HEDIS results, or for any other commercial use, must obtain a commercialuse license directly from the AHA. To inquire about licensing, contact ub04@aha.org.Some measure specifications contain coding from LOINC (http://loinc.org). The LOINC table, LOINC codes, LOINCpanels and form file, LOINC linguistic variants file, LOINC/RSNA Radiology Playbook, and LOINC/IEEE Medical DeviceCode Mapping Table are copyright 1995–2019 Regenstrief Institute, Inc. and the Logical Observation Identifiers Namesand Codes (LOINC) Committee and are available at no cost under the license at http://loinc.org/terms-of-use.“SNOMED” and “SNOMED CT” are registered trademarks of the International Health Terminology StandardsDevelopment Organisation (IHTSDO).“HL7” is the registered trademark of Health Level Seven International.No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical,including photocopy, recording or any information storage and retrieval system, without the written permission of NCQA. 2019“SNOMED” and “SNOMED CT” are registered trademarks of the International Health Terminology StandardsDevelopment Organisation (IHTSDO).“HL7” is the registered trademark of Health Level Seven International.2019 by the National Committee for Quality Assurance1100 13th Street, NW, Third FloorWashington, DC 20005All rights reserved. Printed in the U.S.A.NCQA Customer Support: 888-275-7585NCQA Fax: 202-955-3599NCQA Website: www.ncqa.org12
Table of ContentsTable of ContentsOverview . 15HEDIS 2020 . 15How HEDIS Is Developed . 15What’s New in HEDIS for the Quality Rating System? . 15Additional Resources . 15Referring to HEDIS Measures and Rates . 16If You Have Questions About the Specifications . 17Reporting Hotline for Fraud and Misconduct . 17Reporting Data Errors to NCQA . 17General Guidelines for Data Collection. 19General Guidelines for Data Collection . 202020 HEDIS for QRS Data Collection . 20Definitions . 21The NCQA HEDIS Compliance Audit . 22For Performance Measures . 24In Which Reports Do Exchange Members Remain? . 25Note. 25Note. 26Membership Changes . 26Required Enrollment Periods and Benefits . 27HEDIS for QRS Data Submission and Reporting to NCQA . 28Data Collection Methods and Data Sources . 29Supplemental Data Definitions . 30Required Data Elements . 32Supplemental Data Timeline . 32Identifying and Validating Supplemental Data . 32HEDIS Coding Conventions. 37Guidelines for Calculations and Sampling . 41Guidelines for Calculations and Sampling. 42How to Use the Administrative Method. 42Guidelines for the Hybrid Method . 42Systematic Sampling Methodology . 46Complex Probability Sampling . 50Substituting Medical Records . 50Hybrid Method: Three Approaches . 51References . 51Guidelines for HEDIS Effectiveness of Care Measures . 53Guidelines for HEDIS Effectiveness of Care Measures . 54Description . 54Guidelines for HEDIS Access/Availability of Care Measures . 57Guidelines for HEDIS Access/Availability of Care Measures . 58Continuous Enrollment.
Sep 25, 2019 · QRS measure set. This section includes a list of the QRS measures and a brief background on the QRS measure set. The QRS measure set is comprised of clinical quality measures, including the National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Information and Data Set (HEDI