Transcription
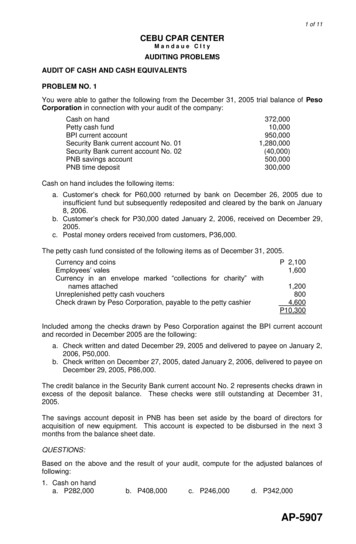
Healthcare and Life SciencesStrategies for Auditing & Improvingthe Charge Capture ProcessHCCA 2005 Compliance InstituteSheraton New OrleansApril 17th - 20th
About the PresenterRichard Williams & Matt JacksonRichard is a Senior Manager, and Matt is a Manager, in the Dallas office of Protiviti Inc., anInternal Audit and Independent Risk Consulting company that helps organizations identify,measure, and manage operational and technology related risks throughout systems andprocesses. Richard and Matt are key leaders in Protiviti's Healthcare Internal Audit andRevenue Assurance practices and have worked extensively with a number of providers inassessing and improving their revenue cycle operations and processes. They have alsoprovided numerous training and awareness sessions focusing on the provider revenue cycleand its impact on hospital operations.Richard received his MBA in Accounting and Information Systems and his Bachelors degreein Accounting. Matt received his Bachelors degrees in Management Information Systemsand Business Management. Richard and Matt are active members of the ProjectManagement Institute (PMI), Institute of Internal Auditors (IIA), Association of HealthcareInternal Auditors (AHIA), Healthcare Financial Management Association (HFMA), and theHealth Care Compliance Association (HCCA).2
Our Goals TodayThis session will focus on charge capture improvement efforts and provide a risk-basedapproach for successfully understanding, assessing, and improving charge captureprocesses in healthcare organizations.During this session, we will accomplish the following objectives: Obtain a basic understanding of the charge capture process and address thenecessity for conducting a charge capture audit. Provide a basic control framework as a baseline for identifying risks, developingcontrols, and enhancing key charge capture processes. Discuss a strategic approach for conducting a successful charge capture audit thatwill enable one to gain a thorough understanding of key charge capture processes,facilitate the understanding of key business processes and controls, and effectivelycommunicate key findings and recommendations with process owners and executivemanagement.3
Charge Capture OverviewChargeChargeCapture Capture l success is directly dependent upon accurately charging for servicesrendered. An effective charge capture program includes proper utilization ofcharge information, processes, and systems, and should be characteristic of thefollowing: Emphasizing equal importance of administrative responsibilities to that placed onpatient care Ensuring that all services rendered are captured and posted timely, accurately, andcompletely Establishing accountability for assigned responsibilities Performing overall monitoring to ensure that policies and procedures are followedconsistently Providing performance feedback Effectively implementing new pricing or charging methodologies4
Charge Capture Overview (cont’d)What are typical reasons for charge capture deficiencies? Charge capture activities are typically performed by care providersand are perceived as a lower priority administrative function. Because it is rarely explained, care providers do not understandthe risks associated and potential consequences for not capturingcharges timely, accurately, and completely. Charge capture responsibilities are extremely decentralizedacross organizations. Formal policies and consistency standards do not exist to provideorganizational guidance and baseline controls for charge postingand reconciliation functions. Different charge capture and charge entry systems are commonlyutilized. Monitoring and feedback reporting for each department’s chargeposting and reconciling responsibilities is inadequate. There is little to no coordination between departments or trainingfor those responsible for charge capture activities. In many departments, administrative assistants earning moderatewages are given responsibility for charge posting and reconcilingactivities.5
Charge Capture Overview (cont’d)What is the impact of deficient charge capture processes?Reimbursement Missed revenue opportunity Delayed payment; increased back-end rework Increased days in accounts receivable Inadequate data for contract negotiationRegulatory Compliance Expensive penalties Inaccurate billing leadingto payer denials Medicare inquiriesPatient Satisfaction Incorrectly billing orre-billing patients,leading to patientdissatisfactionAn effective charge capture audit is aimed atimproving and streamlining charge capture processesenabling the entity and providers to improve patientsatisfaction and enhance profitability, as well asproviding more effective communication andcorroboration between departmental areas.6
Charge Capture Control FrameworkDocumented Policies and ProceduresCharge Sheet Utilization¾ Ensure a reliable schedule, log-book, or otherreport/mechanism is established to documentall patients treated¾ All departments should have a charge sheet(manual or electronic) documenting allchargeable procedures and supplies¾ Confirm that patient account numbers inmedical record documentation andpatient labels match prior to treating the patient¾ Review completed charge sheets fordiscrepancies prior to posting¾ Identify and select correct accounts within thecharge posting systemDaily Reconciliation¾ Reconcile charge sheets to a schedule, logbook, or other report/mechanism to ensurecharges are captured for all patients treated¾ Reconcile charges posted in the chargeposting system (e.g., Departmental ChargeReport) to charge sheets to ensure accurateand complete entry of all charges¾ Review error reports and reconcile corrections¾ Charge sheets should be reviewed on a semiannual basis for completeness and update asneededCharge Entry¾ All charges should be posted the day service isrendered¾ Verify the patient account number prior toentering chargesEducation and TrainingMonitoring and FeedbackPatient Arrival at Department¾ Only enter charges that are documented on thecharge sheet¾ Visually inspect items entered into the systemfor accuracy prior to postingCDM and Charge Screen Updates7
Charge Capture Control Framework (cont’d)PatientArrival lePatientsTreatedReconcileChargesPostedReview /ReconcileApplicableReports1. Ensure a reliable schedule, log-book, or other report/mechanism is established to document allpatients treated This mechanism should accurately reflect all patients treated within each department to be utilizedin downstream reconciliation processes.2. Confirm that patient account numbers in medical record documentation andpatient labels match prior to treating the patient Account numbers on patient labels printed by departments should be matched to accountnumbers on face sheets/patient labels from Patient Access. If discrepancies are identified when confirming the patient accountnumber, Patient Access should be contacted for resolution.3. Identify and select the correct account when selecting patients inthe charge entry system/patient encounter screen Departments should use the “patient account number” identifiedin medical record documentation (e.g., face sheets, labels,physician orders) to accurately select the patient account whenselecting patients. Verify key patient data is correct (e.g., patient name, date of birth,date of service, etc.).8
Charge Capture Control Framework (cont’d)PatientArrival lePatientsTreatedReconcileChargesPostedReview /ReconcileApplicableReports1. Departments should utilize a charge sheet/order requisition documenting all chargeableprocedures, as well as those supplies departments are responsible for posting Charge sheets should be utilized by departments to ensure that all services rendered aredocumented for accurate charge posting. Departments should document all items/services providedthat are not already listed on the requisition. Charge sheets will also be utilized in downstream reconciliation processes.2. Visually inspect items indicated on the charge sheet for completeness prior to submitting forcharge entry Care providers should perform an inspection of items indicated on each charge sheet to ensure thatall services rendered were documented.3. Charge sheets/system charge selection screens should be reviewed, and updated as necessary,on a semiannual basis to ensure completeness and accuracy Any item not listed on the charge sheet/system charge selection screen should be added, and ifnecessary, updated in the Charge Description Master (CDM). Any charge item that is no longer provided should be deleted from the charge sheet/system chargeselection screen.9
Charge Capture Control Framework (cont’d)PatientArrival lePatientsTreatedReconcileChargesPostedReview /ReconcileApplicableReports1. All charges should be posted the day service is rendered Personnel should enter charges on the date of service or follow department guidelines/timeframesfor timely posting of charges. Any situations that arise inhibiting the posting of charges within the department guidelines/timeframesshould be communicated to the department Manager/Director.2. Personnel should verify the patient account number prior to enteringcharges Departments should utilize the patient account number in medical recorddocumentation (e.g., face sheets, labels, physician orders, etc.) to access thepatient account in the particular department system. Verify key patient data is correct (e.g., patient name, date of birth, dateof service, etc.) and, if discrepancies are identified, contact PatientAccess (or other responsible department) for resolution.10
Charge Capture Control Framework (cont’d)PatientArrival lePatientsTreatedReconcileChargesPostedReview /ReconcileApplicableReports1. Designate personnel responsible for reconciling charge sheets to a schedule, log-book, or otherreport/mechanism to ensure charges are captured for all patients treated Ensure a charge sheet has been completed for each patient treated. Tic marks and signatures should be noted on reconciliation work-papers confirming completion. Require a care provider to complete a replacement charge sheet (or enter charges in chargesystem, if applicable) using medical record documentation if a charge sheet/order requisition isidentified as missing. Complete this reconciliation no later than the day following thedate of charge entry, providing ample time for correction(s)prior to bill submission. Reconciliation work-papers should be maintained for a period ofat least 90 days. Department Managers/Directors should review reconciliationwork-papers periodically to ensure compliance with entitycharge capture standards.11
Charge Capture Control Framework (cont’d)PatientArrival lePatientsTreatedReconcileChargesPostedReview /ReconcileApplicableReports1. Designate personnel responsible for reconciling charges posted in the charge posting system tocharge sheets to ensure accurate and complete entry of all charges Any charges documented on the charge sheet that are not reflected in charge reports should benoted and posted. Tic marks and signatures should be noted on reconciliation work-papers confirming completion. Any suspected discrepancy, such as a charge omitted from a charge sheet,should be resolved by a care provider using medical record documentation. Complete this reconciliation no later than the day following the date of chargeentry, providing ample time for correction(s) prior to bill submission. Reconciliation work-papers should be maintained for a period of at least 90days. Department Managers/Directors should review reconciliation work-papersperiodically to ensure compliance with entity charge capture standards.12
Charge Capture Control Framework (cont’d)PatientArrival lePatientsTreatedReconcileChargesPostedReview /ReconcileApplicableReports1. Designate personnel responsible for reviewing error or late charge reports Review system interface reports to ensure all charges interface appropriately. Review late charge reports (e.g., reports showing charges that were entered after the bill wassubmitted) to identify and communicate improvement opportunities to the Manager/Director.2. Designate personnel responsible for reconciling corrections made in the system to errorsidentified on reconciliation work-papers to ensure all discrepancies were addressed Tic marks and signatures should be noted on reconciliation work-papers confirming correctionshave been completed. Complete reconciliation activities no later than the day followingdate of charge entry, providing ample time for correction(s) prior tobill submission. Reconciliation work-papers should be maintained for a period of atleast 90 days. Department Managers/Directors should review reconciliationwork-papers periodically to ensure compliance with entitycharge capture standards.13
Charge Capture Control Framework (cont’d)Other Considerations Price thresholds and materiality posting criteria - If your organization employs thisstrategy, ensure that all supplies and procedures in excess of the set materiality amount havea CDM number. Posting miscellaneous charges - If your organization utilizes different modules or screensfor posting miscellaneous charges, it is likely that fewer or different system controls will exist.Access to these screens should be closely monitored to ensure personnel are not using thesescreens for unintended purposes (e.g., corrections, movement of charges, normal posting ofitems listed on charge sheets, etc.). Departmental specific procedures - Each department should have specific proceduresdocumented that explain the standard process for capturing and entering charges for servicesrendered. These procedures should support entity-wide charge capture policies. Personnel back-ups - Each department should have properly trained back-ups for chargeposting and reconciliation activities. Formal CDM update process - Each department should be familiar and comply with theCDM update process. This process should be part of the entity-wide charge capture policyand should explicitly identify approval requirements. Quality assurance programs - Each entity should have a charge capture quality assuranceprogram whose primary responsibility is to monitor ongoing efforts, provide support, performperiodic testing, and develop/deliver education programs.14
Charge Capture Control Framework (cont’d)Quality Assurance and Ongoing SupportDevelop and MaintainHospital PolicyReview DepartmentalProceduresAudits ofProcesses/ProceduresEnsure Compliance withCDM Update ProcessMonitoring andPerformance FeedbackCharge CaptureQualityAssuranceTeamCommunication of IssuesAddress Charge CaptureConcerns and/or ChangesEducation and TrainingQuality assurance initiatives should include the following: Formalizing entity-wide policy standards that positively impact all departments andcoordinating periodic audits of departmental processes and tools to ensure compliance. Serving as a central point of contact for addressing departmental concerns and/ordesired changes within charge capture processes. Implementing a mechanism for communicating and resolving charge entrydiscrepancies identified by departments such as Patient Access, Patient Accounts,Decision Support, Compliance Office, etc. Coordinating the provision of monitoring and performance feedback reports for trendingand continuous identification of charge capture improvement opportunities. Investigating additional reports and charge entry screens to be utilized by departmentsfor charge posting and reconciling activities. Implementing a formal charge capture process education program.15
Auditing ApproachWhat should be the overall objective of a charge capture improvement audit? The primary objective is to evaluate the effectiveness of internal controls surroundingexisting charge capture functions and perform a high-level assessment of existing chargecapture monitoring, tracking, and reporting procedures to identify business process and/orsystem improvement opportunities within existing operations that, when implemented,would lead to enhanced profitability, cash flow, and compliance. Additional objectives are the overall enhancement of information required for billing andcollections processes, as well as the improvement in communication and collaborationbetween departments.What is involved in a charge capture improvement audit? It typically requires three days for three skilled resources to assess the averagedepartment. The timeframe required is contingent upon the type of departments includedwithin scope, as well as the number of personnel and skill-mix dedicated to the audit.Departments with a higher frequency of error may include: Angiography/Radiology Emergency Room Surgery/Anesthesia Recovery Intensive Care Unit/Critical Care Unit Pharmacy/Lab Birth Center/L&D It also involves assessing the department(s) or person(s) responsible for monitoring,tracking, and reporting to identify deficiencies or opportunities for improvement within thequality assurance functions related to charge capture processes.16
Auditing Approach (cont’d)How should the auditbe performed?This approach is basedon gaining anunderstanding of thebusiness as a means toidentify, source, andmeasure business risk atboth the organizationaland business processlevel.Quality and effectivecommunications are builtinto this methodologywith the goal of workingwith process owners as avalue-added service.Current sultsProcess AnalysisÐProcess AssuranceÐProcess ImprovementUnderstandthe ssMeasures &ControlsAnalyze RootCauses ofProcess &ControlDeficienciesThis approach is designed to analyze and respond to importantquestions, such as:What are thesignificantbusiness risks,both externaland internal,that impact theprocess?How and howwell are thoserisks beingmanaged andcontrolled?What keymeasures areused to monitorthe process?Are they theright ones?Are themeasures,and othermanagementinformationused,reliable?How efficientis the processin operation?How can theprocess beimproved tobring itsperformancecloser toleadingstandards?17
Auditing Approach (cont’d)Current State Assessment Review policies, procedures, and system application manual(s) related to chargecapture processes to gain an understanding of current formal processes andsystem functionality. Also, review documentation from prior reviews performed toidentify problematic areas to focus audit efforts.2Eye Center(Manual Lo g Book)Information faxed byphysician (if received) isused to pre-admitpatients. Patients arenot contactedPhysician Fa xSheets12Scheduling is contactedto schedule appointmentReservation Cards &Schedules34P re-certificati on i sattempted for OR andPSA surgeries onl yPatient Reps usereservation cards andschedules to contactpatients forpre-admissionMa in(LCI and ORSOS)A2MRI & Breast Center(MEDFAX)Was patientpre-admitted?A6YesPatient is directed totreatment area and signsconsents (some areasre-verify informati on)YesFace sheet prints inCase Coord., whichserves as notification tocontact payer for initialauthorizationReviewers areresponsible for o btainingadditional authorizationfor expired staysWas patientadmitted?7NoPatient exits/dischargesPati ent ArrivesNo5Patient informati on i sobtained and enteredi nto IMF Interview and observe key personnel responsible for specific charge captureprocesses including charge posting, charge reconciliation,
¾Review completed charge sheets for discrepancies prior to posting ¾Charge sheets should be reviewed on a semi-annual basis for completeness and update as needed Daily Reconciliation ¾Reconcile charge sheets to a schedule, log-book, or other report/mechanism to ensure charges are captured for all patients treated