Transcription
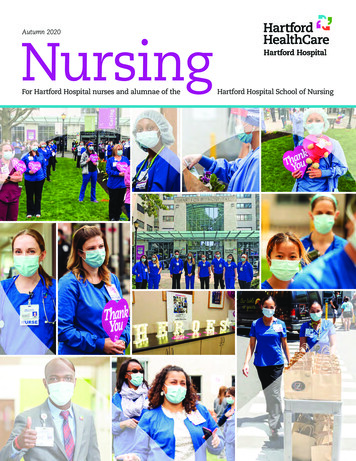
Autumn 2020NursingFor Hartford Hospital nurses and alumnae of theHartford Hospital School of Nursing
Contents1Messages From Executive Leadership2The SCIENCE Of NursingIncident Command Center Team Hit TheGround Running And Never Missed A Beat5The ADVOCACY Of NursingCommunication And Collaboration WithNursing Homes By Case Coordinators EasedTransitions During COVID7The SCIENCE Of NursingThinking Lean Outside The Box Makes The EDResponsive, Adaptable, And Innovative9The ART Of NursingRe-educated And Redeployed Nurses ‘Step Up’To COVID-19 Challenge11The SCIENCE Of NursingImproving Outcomes On The Front LineOf The Pandemic With Proning13The ETHICS Of NursingSix Advance Practice Professionals TalkAbout COVID15The ART Of NursingIOL: From The “CARES Unit” To A “COVIDIsolation Unit” For Behavioral Health PatientsIn Five DaysHartford Hospital’sNursing ProfessionalPractice Model17 Nursing News & Notes19A Message From The PresidentOf The Alumnae Association20Alumnae Spotlight21 A Look Back22 The PILLBOX Alumnae NewsNews And Photos From Our Graduates25 Alumnae CommentsThe Nursing Professional Practice Model wasdeveloped by nurses from across HartfordHospital. It is a visual representation of thescope of nursing practice and nursing’s role inenhancing the human health experience.25 In MemoriamAdvisory BoardCheryl Ficara, MS, RN, NEA-BCVice President, Patient Care ServicesHartford Region, Hartford HealthCareGail Nelson, MS, RN, NEA-BCNurse Director, Regulatory Readinessand Nursing OperationsNursingWriter/EditorPatricia MartinGail NelsonDesignerAlan ColavecchioPhotographyChris RakoczyPhotography CoordinatorKim PiresMary Jane Densmore, MS, BA, RNPresident, Alumnae Association of theHartford Hospital School of Nursing, HHSN ’69Patricia Andreana Ciarcia, MSN, RNExecutive Director of Alumnae Affairs,Alumnae Association of the Hartford HospitalSchool of Nursing, HHSN ’62Hartford Hospital Nursing is a publication of theHartford Hospital Department of Nursing andthe Alumnae Association of the Hartford HospitalSchool of NursingSend correspondence to:Hartford Hospital Nursing80 Seymour StreetHartford, CT 06102-5037Attention: Cheryl Ficara, MS, RN, NEA-BCVice President, Patient Care ServicesHartford Region, Hartford HealthCaree-mail: Cheryl.Ficara@hhchealth.orgAlumnae Association of theHartford Hospital School of Nursing560 Hudson StreetHartford, CT 06106Attention: Pat Ciarcia, MSN, RNExecutive Director of Alumnae Affairse-mail: patciarcia@snet.netTel: 860.563.2005On the cover: A collage of Hartford Hospital staff
Messages From Executive LeadershipDear Colleagues:The Year of the Nursehas been like no otheryear in our history.COVID-19 haschallenged us likenothing before it.Despite the barriers andhardships caused by thepandemic, I’m certainhistory will show thevirus was no match for the outstandingnurses at Hartford Hospital.Despite the uncertainty and ever-changingtwists and turns earlier this year, the resolve,resilience and expertise of the nurses hasbeen an example for us all. The greatercommunity took great solace and comfortin the grace exhibited by the nursingprofession. That appreciation was exhibitedthrough thousands of paper hearts tapedto windows, signs of gratitude placed onlawns and thoughtful donations deliveredto the hospital.The battle is not over and the threat loomsin the air as Connecticut works to retain itsposition as one of the safest states in thenation, recording low COVID numbers asother states struggle to contain the virus.We must maintain our resolve to keepCOVID at bay with attention to detail,patient care and healing, asserting the samemomentum as we did when the pandemicemerged and entered our communityuninvited. I know you’ll continue to set thebar very high in the coming months, leadingthe nursing community in the fight againstCOVID.I am so proud of the focus, expertise andagility of the nurses at Hartford Hospital.Day in and day out, you have shown theworld what it means to be a nurse. It is acalling and a gift, and we are all better for it.COVID-19 is arguably the greatest healthcarechallenge of our generation and prophetically ithappened during the Year of the Nurse.Throughout history, nurses have responded tothe needs of their communities. The 1918 flu, TB,polio, HIV-AIDS, smallpox, H1N1 and Ebola eachsaw nurses on the forefront of care. But thewidespread threat and spread of COVID-19 wasdifferent and the lifesaving work of nurses wasseen and appreciated like never before.During the pandemic, the role of nurses wasnot limited to the bedside and clinical areas atHartford Hospital. Consistent with our nursing Professional PracticeModel, nurses at Hartford Hospital never wavered from demonstratingthe elements of the model – science, advocacy, ethics and art ofnursing. Nurses were involved in emergency management, developingnew treatment protocols, redesigning units, and countless other facetsof the activation.Guided by the most current knowledge of the pandemic andprofessional nursing practice standards, nurses rapidly andcontinuously learned and adapted, initiating therapies such as highflow oxygen, proning and Remdesivir.All the while, you were human, too – balancing and navigatingpersonal stress. Many of you were immersed in home schooling,acquiring childcare and meeting the needs of your own families andloved ones. You were processing the uncertainty of the pandemic alongwith the rest of the nation at home – and at work.Every day you responded to the needs of our community and camein to work, leaving one crisis at home and heading into another. Yourattention to patient care was without equal. When patients wereisolated from their families, you were the conduit and lifeline betweenthe two, comforting and consoling both sides. You delivered care andcompassion to both the sick and the bereaved, making phone callsand facilitating FaceTime visits while administering vital medicalassistance.You are the standard bearers of Hartford Hospital, leading the chargeagainst an invisible foe. Your story will be told for generations to come.The knowledge, compassion and resilience you displayed will beremembered and revered. No doubt, you’ve inspired future generationsof nurses and entire communities, and for that you should be proud.I know I am.Thank you for your selfless contributions to our hospital andcommunity. Thank you for your work ethic and compassion. I aminspired and grateful beyond words.Sincerely,Bimal PatelPresident, Hartford RegionSenior Vice President, Hartford HealthCareCheryl Ficara, MS, RN, NEA-BCVice President, Patient Care ServicesHartford Region, Hartford HealthCareHARTFORD HOSPITAL NURSING / Autumn 20201
The SCIENCE Of NursingIncident Command Center Team Hit The Ground RunningAnd Never Missed A BeatHartford Hospital’s Incident Command TeamAt the beginning of the year, no one could have predicted we would be facing the extraordinary challenges ofa global pandemic the likes of which we’ve never seen before. As the threat of COVID-19 gripped the world, HartfordHospital was well prepared to respond to the crisis with the discipline, focus, and training of its Incident CommandCenter (ICC) team. COVID-19 was declared a pandemic by the World Health Association March 11th. On March 13,a national emergency was declared and soon after the U.S. government mandated that hospitals setup theiremergency management centers. The Hartford Hospital ICC team set up and began day-to-day coordinationfor the hospital.Hartford Hospital nurses with training in emergencypreparedness, serve as members of the IncidentCommand Center. They are an integral part of a multidisciplinary team prepared to provide leadership andcoordination of services in response to an emergency.The ICC team consists of 25 members who had beenworking together for more than a year before the COVIDcrisis. In March 2019, team members traveled toAnniston, Alabama, where they trained for a week atthe Federal Emergency Management Agency’s (FEMA)Center for Domestic Preparedness.FEMA was a bonding experience, and weekly meetingsbrought the team closer. “The team gelled and works sowell together,” said Valerie Neary, MSN, RN, NurseManager, Center 10. “We’re so compatible and capable.During the COVID emergency, we were doing what wewere trained to do, with good common sense. It wasimportant to stay cool, calm, and collected. We wereprepared to mobilize.”2HARTFORD HOSPITAL NURSING / Autumn 2020Margaret Hanbury, RN, MPA, CPHQ, Nurse Director,Quality and Safety Perioperative Services, echoed thesentiment. “Thank goodness for FEMA training. I cannotsay enough about what our team did. Everybody foundwhere they could best be supportive of the process andat the same time bolster each other’s spirits.”Kim Hayes, MS, RN, CNOR, Director of Nursing, Boneand Joint Institute, recalled, “At FEMA we had differentscenarios we were trained in—mass casualties, gasleaks, fire, etc. We were not expecting a pandemic thatwent on for months, but we did cover infectiousdiseases to some degree. A year later, we had a ‘trial byfire’ with COVID-19.”The ICC was instrumental in containing thecoronavirus, protecting patients and staff, and ensuringcapacity. It also provided centralized information aboutCOVID-19 and allowed the system to allocate resourcesand redeploy staff where they were needed the most. Inaddition, the team created and implemented plans for
patient intake, drive-through testing, PPE distributionand other critical processes.The command staff rotated their roles weekly,providing experience, training and flexibility within thegroup. Roles include incident commander, publicinformation, safety officer, operations section chief,planning, logistics, a liaison who interacts withresponding agencies, plus finance and medical technicalsection chiefs.Nurses filled key leadership positions in theemergency command center, leading the coordinatedresponse to patient care and hospital operations,monitoring outbreaks on the local, state and nationallevels and anticipating Hartford Hospital needs. Theyadvised the logistics team and supply chain management in areas including management of personalprotective equipment (PPE), testing supplies, employeescreening. They identified and anticipated additionalareas for care of deceased and temporary overflow, aswell as assessing personnel, space and equipmentneeds. In addition, nurses on the team facilitated staffassignments, PPE and equipment needed for specialprocedures including peri-operative and all surgicalprocedures adapting processes to maintain safety inhemodialysis. They supported the development andoperation of staff screening and designed, trainedand operationalized swabbing teams to ensurestandard quality.ICC nurses served as consultants to the developmentof alternate treatment areas at the CT ConventionCenter, Southern CT State University and Central CTState University. They reached out to nursing leaders,reached out to other hospitals, both within the systemand competitor agencies, to discuss mutual concerns,and to share and support as professional colleagues. Inaddition, nurses in the Command Center consulted withnational organizations including the Organization ofNurse Leaders and Emergency Nurses Association.“During COVID you had to respond and get thingsdone,” said Maria Tackett, RN, EdD, CEN, TCRN, CCRN-k,Nurse Director, Trauma & Professional Practice. “Thestructure and science of an ICC prevents chaos. It’sbased on the National Model of Incident Commandcreated after 9/11 with direction from FEMA andHomeland Security, with coordinated responses aroundthe country.”During the height of the pandemic, the ICC was inconstant contact, met formally twice a day, andreported to hospital staff via telephone conference callsat 8:15 am and 4 pm, with as many as 400 people on theline. In the morning, team members gave a report andthe incident commander would go over objectives andannounce the daily plan. In the afternoon, the teamreviewed the day and updated the staff on such thingsas the number of patients currently being treated, thenumber discharged, the number of deaths that occurred,continued on page 4Before the mask requirement,members of Incident Commandin a COVID-19 planningmeeting in early March 2020,left to right: Susanne Yeakel,MSN, RN, NEA-BC, CNML;Margaret Hanbury, RN, MPA,CPHQ; Jennifer Costanzo MA,CG (ASCP), DLM (ASCP);Giuseppe Mignosa, MBA, MT(ASCP); Valerie Neary, MSN, RN;Gervacio Pangilinan, MSHARTFORD HOSPITAL NURSING / Autumn 20203
Incident Command Center Team Hit The Ground RunningAnd Never Missed A Beatcontinued from page 3where patients were located and the levels of care, asbedside treatments. We would not have been able to dowell as COVID statistics within the state, the nation, andwhat we did without help from the Command Center inthe world. The conference calls were interactive, andgetting us additional, experienced support staff.”anyone with a question had the opportunity to ask it.When a patient had COVID or was suspected of beingDelivering the right care, in the right place at the rightCOVID positive, the nurses had to stay in a private roomtime, is a strategic priority to safe healthcare, evenwith them, with the door closed, throughout the fourduring a pandemic. Enhanced levels of coordinationhours of treatment. “The exposure to COVID is a lotwere required to ensure that all units could adjust togreater in that circumstance,” explained Ilchenko. “Butthe changing demands of patient care. In addition, allbecause PPE was used properly, our nurses were able toongoing vital services including emergency surgery andstay healthy—no one contracted the virus.”infusion, among many“We saved a lot of livesothers, called for continuouswith dialysis,” said Yeakel. “It“It’s great so many nurses arereevaluation, reliable interwas a big accomplishmentrepresented in the Command Center.departmentalthat not one single patientcommunication andwas denied dialysisThe life experience each nurse broughtseamless implementation oftreatment—we provided it toto the table allowed us to do someplans. One of the mostevery patient who needed it.”complex challenges was toDuring this “Year of thegreat things.”provide the continuousNurse,”RNs have been– Margaret Hanbury, RN, MPA, CPHQ, Nurse Director,availability of treatment forinstrumentalin dealingQuality and Safety Perioperative Servicespatients undergoing dialysis.with COVID. “It’s great soDialysis units across themany nurses arecountry were particularly challenged by COVID as therepresented in the Command Center,” said Margaretvirus affects the kidneys. The ICC played an integral roleHanbury, nurse director. “The life experience each nursein reassigning staff to the Hartford Hospital dialysisbrought to the table allowed us to do some greatunit, ensuring that every patient received the dialysisthings.”treatments they needed.“Our great-great-grandchildren will be learning about“Dialysis competency is vital,” said Susanne Yeakel,the COVID pandemic years from now,” says Yeakel. “It’sMSN, RN, NEA-BC, CNML, Nurse Director, Generalhard to imagine that we would ever face this in ourSurgery, Inpatient Rehab, Dialysis, Wound Care, Ostomylifetime, but nurses stepped up—and will continue toProgram. “During COVID, scheduling was a 24/7 program.”step up.”Jarrett Lautier, MSN, RN, Clinical Leader, InpatientThroughout Hartford Hospital’s history, nurses, alongDialysis, said, “Working through Susanne, I was able towith colleagues worldwide have responded to the needsget nurses from other areas of the hospital who hadof their communities. The 1918 flu, TB, polio, HIV-AIDS,some dialysis experience, give them a brief orientation,smallpox, H1N1, Ebola – whatever the threat may haveand get them up and working. It was impressive to seebeen, nurses have been in the forefront of the care andso many nurses wanting to help!”protecting of patients.The dialysis unit successfully responded to theThe pandemic serves as yet another time whenincreasing demands for treatment during the COVIDnurses at Hartford Hospital made visible the essentialcrisis. The unit has eight stations so patients withoutrelevance of their profession. “The Incident CommandCOVID could be dialyzed in the suite at the same time.Center is an example of nursing leadership at its finest,”In addition, there are six dialysis travel machines whichsays Cheryl Ficara, RN, MS, NEA-BC, HHC Regional Vicemade it possible for unstable or COVID positive patientsPresident, Patient Care Services, Hartford Region. “Theto be dialyzed at the bedside.participation of nurses and the voice of nurses from all“A large number of COVID patients had to be dialyzedlevels and specialties in the pandemic assured decisionat bedside so as not to infect other patients,” said Alexmaking from those professionals consistently andIlchenko, BSN, RN, Nurse Manager, Inpatient Dialysis.directly providing care to our patients and their“During COVID, there was a 260 percent increase infamilies. Nurses are uniquely qualified and positionedbedside treatments. Collaborating with a multiat the forefront to respond to any crisis to ensure safetydisciplinary team, we were able to designate a COVIDand quality for our patients and our communities.” positive shift allowing for a decrease in the number of4HARTFORD HOSPITAL NURSING / Autumn 2020
The ADVOCACY Of NursingCommunication And Collaboration With Nursing HomesBy Case Coordinators Eased Transitions During COVIDDuring normal times, HartfordHospital case coordinators play avital role in optimizing throughput.But when the COVID pandemicstruck, “They were exceptional,” saysCheryl Ficara, RN, MS, NEA-BC, HHCRegional Vice President, Patient CareServices, Hartford Region.Supported by administrativeassistants, case coordinators onevery hospital unit performassessments to identify patienttransition needs in order to leave thehospital. What are their post-acutecare needs? Can they go home? Dothey need home care services orsupport services, such as a visitingnurse, or do they need rehab? Or istheir hospital stay best followed byadmission into a nursing home orlong-term acute care hospital.”“It’s a very dynamic process,”says Beth Lawlor, RN, BSN, MS, CCM,NEA-BC, Nurse Director, CaseCoordination, Hartford Hospital.“The plans change constantly, withongoing assessments necessary toensure that the transition plancontinues to meet the patient’sneeds.“In collaboration with the patientand family, we work to develop thebest plan that meets the patient’spost-acute care needs early in thepatient’s hospitalization; every daywe review that plan for anynecessary modifications. During themorning nursing huddle, thoseplans are reviewed, and adjustedaccordingly, and then later in theday, the physicians, nurses, casecoordinators, and administrativeassistants get together to review thecurrent plan for transition for everypatient, to be sure we have the bestplan in motion.”Hartford Hospital saw its firstCOVID-19 patient on March 13th.One of many challenges thepandemic presented was the need tolimit the number of people on theunit to maintain social distancing.By the end of March the casecoordination administrativeassistants were moved off thenursing unit to a centralized area,and the RN Case Coordinatorsremained on the unit to facilitatepatient flow. With the number ofcases growing exponentially in ashort period of time, the casecoordinator, while still on thepatient care units, began to manageall transition planning activitiesthrough the primary nurse, and viaphone with patient and/or families(who were no longer allowed to visit).Every day, both the administrativeassistants and case coordinatorswere supported by their departmentleadership through daily roundingtouch points to discuss patient flowand identify the most challengingcases in order to facilitatethroughput on an ongoing basis.The biggest threat was thedifficulty in managing the output,and every day presented newchallenges to the front line casecoordinators. Even with the firstsu
of alternate treatment areas at the CT Convention Center, Southern CT State University and Central CT State University. They reached out to nursing leaders, reached out to other hospitals, both within the system and competitor agencies, to discuss mutual concerns, and to share and support as professional colleagues. In