Transcription
Management of Anaemia in Primary Care PathwayDocument type:Clinical GuidelineVersion:1Author (name):Sharran Grey1, Helen Wright2, MuhammadAthar3Author (designation):1Principal Clinical Scientist/ Blood TransfusionClinical Lead, Bolton NHS FT2Demand Management Programme Lead ,NHSBolton Clinical Commissioning Group3General Practitioner Lead, Bolton ClinicalCommissioning GroupValidated byBolton CCG Demand management SteeringGroup1Bolton CCG Clinical Standards sfusionDate validated03.07.151, 21.08.152, 16.03.163Ratified by:Bolton CCG Clinical Standards BoardDate ratified:18.09.15Name of responsiblecommittee/individual:Trust Hospital Transfusion CommitteeName of Executive Lead (for policies only)Master Document Controller:Barbara ColmanDate uploaded to intranet:TBAKey wordsAnaemia, ironReview date:December 2017VersionDate1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 1 of 14
Version controlVersion1Type of ChangeNew guidelineDateRevisions from previous issuesNovember2015Not applicable.Equality ImpactBolton NHS Foundation Trust strives to ensure equality of opportunity for all service users, local people and the workforce. Asan employer and a provider of healthcare Bolton NHS FT aims to ensure that none are placed at a disadvantage as a result ofits policies and procedures. This document has therefore been equality impact assessed to ensure fairness and consistencyfor all those covered by it regardless of their individuality. The results are shown in the Equality Impact Assessment (EIA).ContentsPurpose and Scope of Document3Pathway for Management of Anaemia inPrimary Care4Monitoring and Compliance12Appendix - References12Equality Impact Assessment13VersionDate1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 2 of 14
Purpose and ScopeThe purpose of the pathway is to maximise identification, investigation and treatmentof anaemia in primary care, ensuring GP’s have appropriate diagnostic andtreatment guidance, and clear access to secondary care services and pathways(hosted on DXS Point-of-Care ). This is intended to avoid unnecessary outpatientreferrals and inpatient admissions, and to ensure patients referred for electivesurgery have their haemoglobin optimised. Avoidance of post-operative anaemiareduces the requirement for blood transfusion, reduces post-op morbidity and lengthof stay. Specifically, Iron Deficiency Anaemia (IDA) is classed as a chronicambulatory care sensitive condition (ACSC) and the active prevention of ACSCadmissions is the responsibility of the CCG.The pathway provides a framework for current best practice in anaemiamanagement and optimisation of patients for elective surgery, and has receivedexpert clinical review and approval by:Sharran Grey (Principal Clinical Scientist/Blood Transfusion Clinical Lead, BoltonNHS Foundation Trust)Suzanne Roberts (Consultant Haematologist, Bolton NHS Foundation Trust)Kadukkavil Padmakumar (Consultant Gastroenterologist, Bolton NHS FoundationTrust)Muhammad Athar (General Practitioner Lead, Bolton Clinical Commissioning Group)The pathway and guidance section of this document in held by Bolton CCG, andexists in this document controlled format for use by Bolton NHS Foundation Trust.Document review and audit will be performed jointly across both organisations.VersionDate1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 3 of 14
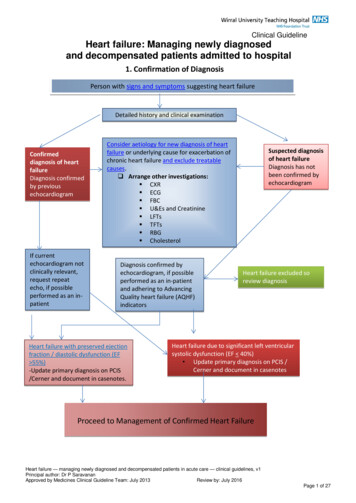
Anaemia Management in Primary CareSecondary CarePrimary CarePatient presents with suspectedanaemia or for elective surgeryClinical assessmentand FBC (first line test)AnaemiaHb 130g/L (Male), Hb 120g/L (Female)ndPerform 2 line tests: repeat FBC, Retics, U&E, Creatinine,LFT, Ferritin, B12, Folate, CRPNon‐Iron Deficiency Anaemia(Ferritin normal or raised)Iron Deficiency Anaemia(Ferritin 30ug/L)Not for elective surgeryAnaemia with suspectedhaemorrhage, cardiaccompromise or severesymptomsSend to AmbulatoryCare UnitFor elective surgeryTimingNot CriticalHyperlink to guidance for MCV 80TimingCriticalSecondary care referralguidance(Follow guidance inhyperlinks)Hyperlink to guidance for MCV 80‐100Trial of oral iron for four weeksHyperlink to Iron Deficiency guidanceHyperlink to guidance for MCV 100HbNormalisedHb NOTnormalisedHb females 120g/LHb Males 130g/LHb females 120g/LHb Males 130g/LIV Iron infusionRefer toGastroenterologyfor IV ironRefer to Gastroenterologyfor IV iron infusion and/orGI investigationRefer to gynaecology ifmenorrhagiaRed Flags Present?Males and Females with DyspepsiaPostmenopausal females with GI symptomsKey messages (hyperlink to general principles)Most anaemic patients will have Iron Deficiency Anaemia, and the majority will respond to oral iron.General Principles in the Diagnosis, Investigation and Treatment of AnaemiaPatients who are to be referred for elective surgery must be screened for anaemia and their haemoglobin must be optimised priorto surgery.Version1DocumentManagement of Anaemia in Primary Care PathwayPage 4 of 14Refer to appropriatecare specialtyinvestigate the underlying cause of anaemia (e.g. GI, gynaecological,DateNovsecondary2015Next ReviewtoDatehaematological, renal).
WHO / BCSH classification of anaemia(Hb)Males: 130 g/lFemales: 120 g/lPregnancy: 110 g/l (T1), 105 g/l (T2), 100 g/l (T3)Step 1Establish presence of anaemiaFBC: Hb, MCV, MCHStep 2Initial Work‐UpRepeat FBC (to exclude spurious anaemia)Reticulocytes (blood film is automaticallyperformed where indicated)Ferritin, B12, Folate, U&E, creatinine, LFTs, CRPClinical history and examinationStep 3Establish type of anaemiaCommence appropriate corrective therapyFurther appropriate investigation, if required, toestablish causeStep 4Monitor response to corrective treatmentTreat cause(Unless not in patient’s best interests)VersionDate1Nov 2015DocumentNext Review DateClinical history should include‐ Drug history‐ Family history‐ Social history inc diet, alcohol and ethnicoriginType of anaemia and any furtherinvestigation will be guided by the MCV(May be multifactorial)Corrective treatment (e.g. Iron) must becommenced immediately even if definitiveinvestigation remains outstandingRed FlagsAnaemia with abnormal blood film/ whitecells/ platelets- Refer to haematologyGI Symptoms‐ Follow dyspepsia/ colorectal guidelinesManagement of Anaemia in Primary Care PathwayPage 5 of 14
Microcytic AnaemiaMean Cell Volume (MCV) 80 flFerritin 30 μg/lNon‐iron deficientmicrocytic anaemia orfunctional iron deficiencyConsider:Non‐haematological causeIron deficiency (IDA)-Hyperlink to IronDeficiency guidanceAssess for source ofbleeding (includingurine dipstick)Ferritin 100 μg/lFerritin30 μg/l – 100 μg/lIron Studies(Iron/TIBC/Iron Saturation)-Acute/ chronicinflammationChronic infectionMalignancyLiver diseaseRenal failureHaematological cause-Refer as appropriateRefer togastroenterology (unlessovert non‐GI blood loss)if :‐ Adult male‐ Postmenopausalfemale‐ Premenopausal femalewith GI symptomsVersionDate1Nov 2015Haemoglobinopathyeg: ThalassaemiatraitSideroblasticanaemiaRefer to appropriate specialtyCRP 30Iron 7 µ mol/LIron Saturation 20%TIBC 45µ mol/LCRP Normal/ elevatedIron 7 µ mol/LIron Saturation 20%TIBC 45µ mol/L(functional iron deficiency)(iron replete)DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 6 of 14
Iron DeficiencyClassically presents with reduced MCV and MCH (Microcytic, hypochromic).However, in early iron deficiency and anaemia of chronic disease (where there may be a functionaliron deficiency), MCV and MCH can be normal.There may also be an associated iron deficiency with chronic blood loss and haemolysis.Ferritin, B12 and folate should be assessed in all cases of anaemia, irrespective of MCVAll patients with iron deficiency anaemia should be screened for coeliac disease with TTG antibodyTreatment of iron deficiency anaemiaOral replacement. 100 ‐ 200mg elemental iron daily (e.g. 200mg bd ferrous sulphate) Take on an empty stomach with a glass of unsweetened orange juiceAvoid simultaneous administration of other medications/antacidsAscorbic acid 500mg dailyFor nausea/ epigastric discomfort, prescribe preparation with lower iron contentDietary adviceParenteral iron, if Poor oral iron tolerance/ non‐complianceImpaired GI absorptionHaemodialysisFunctional iron deficiencyMajor surgery in 8 weeksTransfusionTransfusion should only be considered in cases of massive haemorrhage, imminent cardiaccompromise or severe symptomsMonitoring response to iron replacementRepeat FBC after 4 weeks treatment. If improvement inHb (10 – 20 g/l): Continue replacement for 2 – 4 months, then re‐check HbIf Hb normalised, continue iron replacement for 3monthsIf no improvement, consider switch to parenteralironVersionDate1Nov 2015DocumentNext Review DateIron SaltAmountFumerateSulphate, nt of Anaemia in Primary Care PathwayFerrousIron65mg65mg60mg35mgPage 7 of 14
Normocytic/Normochromic AnaemiaMean cell volume (MCV)80 ‐ 100 flIsolatedAnaemiaPancytopeniaReticulocyte Count9 80 x 10 /lReticulocyte Count9 80 x 10 /lRefer to Haematology:‐ Bone marrow infiltration‐ Bone marrow failureBilirubinNormalBilirubin ElevatedPossibleBleedingPossible HaemolysisBlood FilmDifferentials: Iron deficiency Mixed haematinicdeficiency Non‐haematologicalcause/ anaemia ofchronic disorder HaematologicalExclude iron / functionaliron deficiencyHyperlink to guidance forMCV 80 PlusReview B12 and FolateresultInvestigate asindicated byhistoryBlood filmLDHDAT (Direct Anti‐globulin Test)Refer toHaematologyConsider possible secondary iron deficiencyReview iron studiesTreat any iron deficiency whilst awaitingfurther investigationHyperlink to iron deficiency guidanceRefer to haematology ifremains unexplainedVersionDate1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 8 of 14
Macrocytic AnaemiaMean cell volume (MCV) 100 flReticulocytesIsolated AnaemiaPossible Haemolysis(See guidance for MCV 80 – 100 fl)9 80 x 10 /LNormal B12/ folate andAsymptomatic of B12/ folate deficiencyReticulocytes9 80 x 10 /LConsider:Alcohol, Hypothyroidism, Drugs, Liverdisease, PregnancyHaematological disorder (e.g. MDS,Myeloma) 3 μg/LSerumFolateSerum B12(Ensurefolatenormal)If 170 ng/Land no symptoms re check in 2months1Nov 2015Blood FilmConsider B12/ folatedeficiencyRefer to Haematology ifsuspect:Bone marrow infiltration orBone marrow failureFolate replacement andmonitor responseHyperlink to folate deficiencyB12 170 ng/L – nofurther investigationB12 still 170 ng/Lcheck Intrinsic factorantibodyCommence B12 replacementHyperlink to B12 deficiencyIf 170ng/Lor symptomaticB12 170 ng/lL, BUTstrong clinical suspicionVersionDateEnsure B12 NormalCoeliac Screen3 – 4.5 μg/LSymptomatic 170 ng/lPancytopeniaCheck Intrinsicfactor (IF)antibodyDocumentNext Review DateIntrinsic factor antibody positive(or negative, but with clinical response)Management of Anaemia in Primary Care PathwayTrial of low doseoral cobalaminIF AntibodyNEGIF AntibodyPOSLifelong B12ReplacementPage 9 of 14
Folate DeficiencyMacrocytic anaemia with megaloblastic changes (macrocytic red cells and hyper‐segmentedneutrophils seen on blood film)Causes of folate deficiencyDietaryDeficient diet, AlcoholismMalabsorptione.g. Coeliac disease, tropical sprue, IBD, jejunal resection)Excess requirementse.g Physiological – Pregnancy, prematurity/ infancy, Malignancy, Haemolytic anaemia (inc SickleCell), Inflammation (e.g. TB, Crohn’s disease)Medicatione.g. Methotrexate, Sulfalazine, Cholestyramine, AnticonvulsantsMetabolicExcess urinary excretione.g. Congestive heart failure, chronic dialysis, acute liver damage)Treatment Ensure vitamin B12 levels normal/ replaced to avoid development of sub‐acute combineddegeneration of the cordDietary adviceFolic acid 5mg daily for 4 months (may require prolonged treatment if cause persists)Further investigation and referral Generally, dictated by the likely aetiology If history consistent with malabsorption – screen for coeliac disease (anti‐transglutaminase antibodies (TTG)) Haematology referral/advice – aetiology uncertain, suspected haematological malignancy Gastroenterology referral – Suspected malabsorption, positive coeliac screen Consider referral to dieticianMonitoring response to folate replacement1. FBC and reticulocytes 10 days following initiation of treatment- Improvement in Hb- Reticulocyte count above normal level2. Repeat FBC at 8 weeks and completion of treatment to ensure normalisation of HbVersionDate1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 10 of 14
Vitamin B12 DeficiencyMacrocytic anaemia with megaloblastic changes (macrocytic red cells and hyper‐segmentedneutrophils seen on blood film)Causes of vitamin B12 deficiency1. Gastric – (e.g. gastrectomy, atrophic gastritis, H. pylori)2. Intestinal – (e.g. resection, malabsorption, ileal Crohn’s, chronic tropical sprue)3. Dietary4. Drugs – (e.g. colchicine, neomycinm anticonvulsants, PPIs/ H2 receptor antagonists)5. Pernicious AnaemiaApparent vitamin B12 deficiency1. Metformin – Check intrinsic factor antibodies if B12 levels reduced. Treat if positive orstrong clinical suspicion of deficiency (with yearly B12 monitoring)2. Pregnancy – Levels drop 30% by T3. Only treat if strong clinical suspicion of deficiency or 100 ng/L.3. Oral contraceptives/ HRT – Only investigate further / treat if B12 150 ng/l or strongclinical suspicion of deficiencyTreatment Patients with neurological symptoms ‐ Do not delay treatmentndInitially: 1000mcg hydroxycobalamin (IM) every 2 day until no furtherimprovementMaintenance: 1000mcg hydroxycobalamin (IM) every 2 months for life Patients with no neurological symptomsInitially: 1000mcg hydroxycobalamin (IM) 3x/ week for 2 weeksMaintenance for non‐dietary cause: 1000mcg hydroxycobalamin (IM) every 3 monthsfor life Dietary cause: 1000mcg hydroxycobalamin (IM) twice per year or 50 – 150mcgcyanocobalamin (PO) daily (vegans/ proven dietary deficiency)If dietary deficiency corrected, B12 can be stopped once levels normalised. Givedietary advice.Further investigation and referral: Generally, dictated by the likely aetiology. Haematology referral/advice – Pregnancy, Neurological symptoms, aetiology uncertain, suspected haematologicalmalignancy. Gastroenterology referral if suspected malabsorption (other than pernicious anaemia),Pernicious anaemia with GI symptoms. Consider referral to dietician.Monitoring response to Vitamin B12 replacement: Perform FBC and reticulocytes 10 days followinginitiation of treatment. Expect improvement in Hb and Reticulocyte count above normal level. Checkfolate if no improvement. Repeat FBC at 8 weeks and completion of treatment to ensurenormalisation of Hb. Haematology advice if persistent symptoms despite replacement.VersionDate1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 11 of 14
Monitoring ComplianceArea to be monitoredMedical patientsElective surgicalpatientsMethodologyWhoReported toFrequencyAudit ofsecondary care Bloodreferrals whereTransfusionprimary cause is Clinical LeadanaemiaHospitalTransfusionCommitteeEvery 2 yearsAudit of pre-opanaemia, post-op BloodTransfusionmorbidity andClinical Leadlength of stayHospitalTransfusionCommitteeEvery 2 yearsAppendix: References1. SHOT (2014). Annual SHOT Report 2013. [Online]. [Accessed 04.06.15].Available at: supplement2013/2. National Comparative Audit of Blood Transfusion (2013). 2011 Audit of Use ofBlood in Adult Medical Patients – Part 2. [Online]. [Accessed 14 April 2014].Availableat: http://hospital.blood.co.uk/library/pdf/2011 Medical Use Audit Part 2 Report.pdf3. Central Manchester University Hospitals NHS Trust (2013). Manchester AnaemiaGuide. [Online]. [Accessed 14 April 2014]. Availablefrom: naemia%20guide.pdf4. DHSSPSNI (2012). 4 Steps in the Investigation and Management of the AdultPatient with Anaemia. [Online]. [Accessed 14 April 2014]. Availablefrom http://www.dhsspsni.gov.uk/hss-md-22-2012.pdf5. British Committee for Standards in Haematology (2013). Guideline for thelaboratory diagnosis of functional iron deficiency. British Journal of Haematology,161 (5), 639 – 648. Availablefrom: 11/pdf6. NICE (2013). Clinical Knowledge Summaries. Anaemia – B12 and folatedeficiency. [Online]. [Accessed 14 April 2014]. Availablefrom: ciencyVersionDate1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 12 of 14
7. British Society of Gastroenterology (2011). Guidelines for the management of irondeficiency anaemia. Gut, 60; 1309- 1316.8. British Committee for Standards in Haematology (2014). Guidelines for diagnosisof cobalamin and folate disorders. British Journal of Haematology, 166, 496 –513. Available from 59/pdf9. Blood Transfusion NICE Guideline (NG24) 2015. 18 Nov 2015.10. British Committee for Standards in Haematolog (2015). Guideline on theIdentification and Management of Pre-Operative Anaemia. British Journal ofHaematology, 171, (3), 332-331Equality Impact AssessmentYes/No1.Does the document/guidance affect one groupless or more favourably than another on the basisof: Raceno Ethnic origins (including gypsies and travellers)no Nationalityno Gender (including gender reassignment)no Cultureno Religion or beliefno Sexual orientationno Ageno Disability ‐ learning disabilities, physicaldisability, sensory impairment and mentalhealth problemsno2.Is there any evidence that some groups areaffected differently?no3.If you have identified potential discrimination, arethere any valid exceptions, legal and/orjustifiable?no4.Is the impact of the document/guidance likely tobe negative?no5.If so, can the impact be avoided?na6.What alternative is there to achieving thedocument/guidance without the impact?na7.Can we reduce the impact by taking differentnaVersionDateComments1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 13 of 14
action?VersionDate1Nov 2015DocumentNext Review DateManagement of Anaemia in Primary Care PathwayPage 14 of 14
of anaemia in primary care, ensuring GP's have appropriate diagnostic and treatment guidance, and clear access to secondary care services and pathways (hosted on DXS Point-of-Care ). This is intended to avoid unnecessary outpatient referrals and inpatient admissions, and to ensure patients referred for elective