Transcription
CONTINUING PROFESSIONAL DEVELOPMENT2.0 ANCCCONTACT HOURSNurse Cognition, Decision Support, and BarcodeMedication AdministrationA Conceptual Framework for Research, Practice, and EducationElizabeth Ann Sloss, MSN, MBA, RN, CNL, Terry L. Jones, PhD, RNThis article synthesizes theoretical perspectives related tonurse cognition. We present a conceptual model that canbe used by multiple stakeholders to study and contemplatehow nurses use clinical decision support systems, and specifically, Barcode-Assisted Medication Administration, tomake decisions during the delivery of care. Theoretical perspectives integrated into the model include dual processtheory, the Cognitive Continuum Theory, human factors engineering, and the Recognition-Primed Decision model. Theresulting framework illustrates the process of nurse cognition during Barcode-Assisted Medication Administration.Additionally, the model includes individual or human and environmental factors that may influence nurse cognition anddecision making. It is important to consider the influence ofindividual, human, and environmental factors on the process of nurse cognition and decision making. Specifically,it is necessary to explore the impact of heuristics andbiases on clinician decision making, particularly related tothe development of alarm and alert fatigue. Aided by theproposed framework, stakeholders may begin to identifyheuristics and cognitive biases that influence the decision of clinicians to accept or override a clinical decisionsupport system alert and whether heuristics and biasesare associated with inappropriate alert override.KEY WORDS: Barcode-Assisted Medication Administration(BCMA), Decision support, Nurse cognition, Nurse decisionwenty years ago, the Institute of Medicine published the groundbreaking report To Err Is Humanand shed light on the prevalence of medical errorsin the United States. At the time, an estimated98 000 patient deaths occurred annually as a directresult of human error.1 Despite efforts to make healthcaresafer, a recent study demonstrated that medical errors mayTAuthor Affiliations: Department of Professional Nursing Practice, Georgetown University (Ms Sloss),Washington, DC; and Department of Adult Health and Nursing Systems, Virginia CommonwealthUniversity (Dr Jones), Richmond.The authors have disclosed that they have no significant relationships with, or financial interestin, any commercial companies pertaining to this article.Corresponding author: Elizabeth Ann Sloss, MSN, MBA, RN, CNL, Department of ProfessionalNursing Practice, Georgetown University, St. Mary's Hall #410, 3700 Reservoir Road NW,Washington, DC 20057 (eak47@georgetown.edu).Copyright 2021 Wolters Kluwer Health, Inc. All rights reserved.DOI: 10.1097/CIN.0000000000000724Volume 39 Number 12result in over 250 000 patient deaths annually.2 Nurses, being at the forefront of care delivery, spend more time withpatients than most other providers.3 The ability for nursesto think critically and make clinical decisions free from human error is essential to patient safety.4 The dynamic clinicalenvironment in which nurses work is characterized by uncertainty, urgency, and high consequence, requiring quick andcritical decision making.3,5 Thus, study of nurse cognitionand factors that influence nurses' decision making within thecurrent healthcare context is necessary to improve patientsafety and quality care. This article provides a synthesis of theoretical perspectives related to nurse cognition and presents aconceptual model that can be used by multiple stakeholders.Stakeholders such as researchers, hospital administrators,nurse educators, and informaticists can use this frameworkto further explore or consider how nurses use clinical decisionsupport systems (CDSSs) to make decisions during caredelivery.BACKGROUNDNurses routinely make clinical and nonclinical decisions thatdirectly impact patient safety and outcomes.6 Critical carenurses, for example, make over 1000 decisions during a12-hour shift.7 Medication administration is a commonand safety-critical focus of nurse decision making.8 A recentstudy found that nurses administer, on average, approximately 20 medications during a 12-hour shift.9 It is estimatedthat 20% of all medication errors occur during the administration stage.10,11 Medication errors and, specifically, adversedrug events cause up to 700 000 emergency department visitsand 100 000 hospitalizations annually.12Clinical Decision Support SystemsA recent study found that during a work shift, nurses spendan average of 33% of their time interacting with varioustechnologies, including the electronic health record (EHR),intravenous infusion pumps, heart monitors, and others.13Defined as computer-based systems that enhance decisionmaking through organization and presentation of relevantinformation, CDSSs are built into many of these technologies to aid nurses' decision making and support the safetyand quality of care.14,15 However, CDSSs can be a sourceCIN: Computers, Informatics, NursingCopyright 2021 Wolters Kluwer Health, Inc. All rights reserved.851
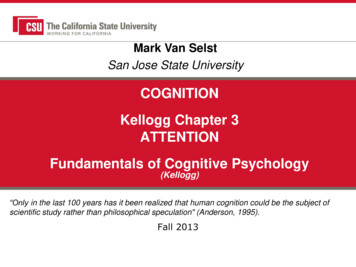
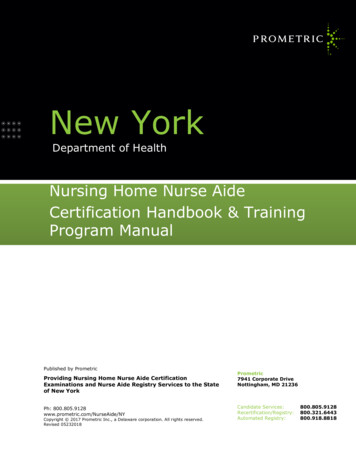
CONTINUING PROFESSIONAL DEVELOPMENTof additional error when not used as intended.15 Significantgaps in the literature exist related to understanding the interaction between CDSSs, nurse cognition, and decision making.5,15Barcode-Assisted Medication AdministrationBarcode-Assisted Medication Administration (BCMA) is atype of CDSS designed to reduce medication administrationerrors. Originally developed in 1995 at the Veterans AffairsMedical Center in Topeka, Kansas, BCMA was more broadlyimplemented in acute care settings nationwide beginning inthe early 2000s.16 During BCMA, nurses verify the rights ofmedication administration by scanning the patient's identification band and medication packaging. The electronicsystem determines if there is a match between patientidentification, medication order (drug, dose, route, andtime), and the medication on hand. If there is a discrepancy,an alert appears to warn the nurse of a mismatch. Indeed,numerous studies show that when used appropriately, BCMAis effective in reducing medication administration errors.17,18However, some unintended consequences of BCMA emergedthat introduced new sources of error associated with medication administration.Alarm FatigueAn unintended consequence of CDSS use is the occurrenceof alarm or alert fatigue. Alarms/alerts in the clinical settingare designed to signal or warn clinicians of unsafe situationsthrough auditory or visual cues.19 However, given the proliferation of technology throughout hospitals and the promiseof alarms/alerts to improve patient safety, clinicians encounter hundreds or more alarms/alerts each day.19 For example,researchers estimate the prevalence of alarms in the intensivecare unit setting to range from 100 to over 350 per patientbed each day. By extrapolation, this means that an individualnurse may be confronted with over 1000 alarms per shift.20Significantly, it is estimated that 80% to 99% of alarms arenot clinically meaningful or do not require action on the partof the clinician.20,21 When clinicians are exposed to numerous false alarms or alarms that do not require action, desensitization to the alarm stimulus develops.6 The resultingdelay in the rate and timing of clinician response alarms isknown as alarm fatigue.20Alarm fatigue is hypothesized to develop over time, as clinicians are exposed to excessive, repetitive alarms.21 One mechanism linked to the development of alarm fatigue is the sheernumber of alarms that clinicians are confronted with. Theresulting auditory sensory overload causes desensitizationto the sound of alarms.22 Additionally, alarm fatigue maybe caused by the “cry wolf” effect, where the occurrence ofrepeated false alarms, rather than the sheer number of alarmsounds, diminishes clinician response.20852Similar to but distinct from auditory stimuli provided byalarms, visual alerts, such as those generated by computerized provider order entry (CPOE), are also associated withfatigue.23 It is reported that providers override or ignore49% to 96% of all CPOE-related alerts.24 Like auditory alarms,the quantity and low clinical meaningfulness of visual alertslikely contributes to alert fatigue.25In BCMA specifically, the nurse may grow accustomed toreceiving an alert for a specific drug or when administeringmedication to a specific patient, and the familiar patternsor situational cues may impact the nurse's decision to acceptor override the alert. For example, if a nurse receives an alertwhen preparing to administer a medication related to incorrect time, the nurse would likely verify the frequency specifiedby the order and the last documented time of administrationin the patient's record, overriding the alert if it is appropriateto continue with administration. However, if the erroneousalert continues to be generated in subsequent medication administration encounters, the nurse is prompted to repeatedlydisregard the alert and “learns” that it is meaningless. An error may occur, then, if the nurse mistakenly decides to override the alert and continue with medication administrationwhen it is not time for the patient to receive the medication.To mitigate the harmful effects of alert fatigue, better understanding of how BCMA alerts affect the cognitive processes ofnurses is needed. In this article, we examine BCMA in thecontext of leading theories of human cognition and proposean integrated conceptual framework to guide inquiry intonurse decision making during BCMA.HUMAN COGNITION AND DECISION MAKINGWe synthesized multiple theories of human cognition anddecision making to explain these cognitive processes duringBCMA. Specifically, dual process theory, the Cognitive Continuum Theory (CCT), human factors engineering (HFE),and the Recognition-Primed Decision (RPD) model servedas the theoretical threads of the proposed model. Displayedin Figure 1, the proposed conceptual model illustrates theprocess of nurse cognition and the factors that contribute tonurse cognition and decision making during BCMA. In order to explain and understand various components includedin the model, it is necessary to further describe the selectedhuman cognitive and decision-making theories.Dual Process TheoryThe dual process theory reflects a two-system approach tohuman cognition.26 With regard to thinking, judgment, anddecision making, the dual process theory posits that thereare two modes of human cognition, one that is quick and another that is slow. The first mode, known as System 1, is fast,effortless, and automatic.27 System 2, alternatively, is slow, effortful, and controlled.27 Given these characteristics, SystemCIN: Computers, Informatics, NursingCopyright 2021 Wolters Kluwer Health, Inc. All rights reserved.December 2021
FIGURE 1. Conceptual model. This model synthesizes theoretical perspectives related to nurse cognition and can be used to studynurse cognition and decision making while using CDSSs, such as BCMA.1 is commonly associated with intuition, whereas System 2 islinked to reflection or conscious reasoning.27Another key characteristic of System 1 is that it is associative and governed by habit.27 In other words, System 1 seeksout or detects patterns and familiar cues and uses these patterns or cues to develop quick, intuitive impressions. Further,System 1 relies on heuristics, or mental shortcuts, to makejudgments, which can result in biases.28 Many of the identifiedheuristics and biases are thought to arise from evolutionaryorigins, but some may also be learned from social, cultural,and environmental contexts.28 It is the use of these heuristicsand associated biases by System 1 to make intuitive judgmentsthat often leads to error.28System 2 is often described as being an overseer for System 1, and errors in judgment by System 1 often result frompoor oversight by System 2.29 System 2 cognition requiresworking memory and sufficient mental capacity and is subject to interruption from other effortful tasks.26,27 Becauseof this, the majority of judgments that humans make on adaily basis are thought to stem from System 1 cognition.27Heuristics and BiasesHeuristics are mental shortcuts employed by System 1 to aidin decision making but can lead to error.30 Biases result froman error in judgment that occurs as a result of a heuristic.31According to a report published by The Joint Commission,over 100 cognitive heuristics or biases have been identified.32One example of a cognitive bias is the learned desensitization(heuristic) of an alert that results in an inappropriate decisionby the nurse to override during BCMA. Other heuristics andbiases that may influence the nurse's decision to accept orVolume 39 Number 12override an alert include but are not limited to anchoring bias,availability bias, and automation bias.Anchoring bias occurs when one gives weight to initial information or impressions, despite the availability of new information.32 For example, during BCMA, a nurse mayplace undue weight on the cognitive impressions from theinitial steps of medication administration (illustrated in theconceptual model as the first cognitive processing step). Eventhough an alert is generated, anchoring bias results in thenurse relying too heavily on initial impressions and not considering new information, such as the alert stimulus. Whilenot related to the nurse's use of BCMA, specifically, onestudy found that anchoring bias influenced both how providers interact with and how they interpret the results of aCDSS when making diagnoses.33 Another study acknowledged that anchoring bias is a common cognitive error thatoccurs when clinicians use CDSSs and may lead to errors.34Availability bias occurs when one makes an intuitive judgmentdrawing from previous, recent experiences.32 This type of bias isreported in the medical literature in relation to medical diagnosis.When making medical diagnoses, research shows that providersmay make diagnostic errors if a current clinical case presents similar to recent prior clinical case(s).31 The availability heuristic isshown to influence nurse decision making in the clinical setting,35 although it has not been linked specifically to nursecognition during BCMA. Theoretically, recent medicationadministration encounters where an alert was generatedmay influence a nurse's decision to accept or override subsequent alerts that are generated during BCMA.More recently, the concept of automation bias has beendiscussed in the clinical informatics literature.36 AutomationCIN: Computers, Informatics, NursingCopyright 2021 Wolters Kluwer Health, Inc. All rights reserved.853
CONTINUING PROFESSIONAL DEVELOPMENTbias is defined by Mosier and Skitka as “the tendency to useautomated cues as a heuristic replacement for vigilant information seeking and processing.”36 Automation bias occurswhen clinicians rely too heavily on automated cues fromCDSSs and may make errors as a result of failing to considernonautomated cues or incorrectly trust automated cues.36When administering medications using BCMA, automationbias may lead a nurse to administer an incorrect medicationeven if the system does not recognize the medication as beingincorrect and no alert is generated.Cognitive Continuum TheoryRelated to the dual process theory, the CCT was proposed byHammond in 1981.37 Rejecting the dichotomy of System 1and System 2 processing, Hammond proposed that cognitionexists on a continuum spanning from intuition to analysis.37The CCT links clinical task structure to nurse cognition, categorizing tasks from well-structured to ill-structured based on complexity, level of ambiguity of content, and presentation. The CCTsuggests that ill-structured tasks stimulate intuitive cognitive processes by the nurse, while well-structured tasks stimulate analyticalcognitive processes.37 The clinical work of nurses in today's complex work environment often presents as ill-structures tasks; therefore, it is hypothesized that nurses primarily use intuitive cognitionwhen making clinical decisions.37Human Factors EngineeringThe term “human factors” refers to human physical characteristics (eg, anthropometric measurements), cognitive characteristics, and interactions between humans and theoverall work system or environment.38 Human factors engineering emerged as a scientific field at the intersection of psychology and engineering that is focused on designing worksystems to improve human performance.38 In healthcare,specifically, HFE promotes the incorporation of cognitiveand physical considerations of clinicians into systems designwith the goal to improve patient safety and quality of care.38The consideration of human factors, and subsequently,HFE, is particularly relevant to alarm/alert fatigue andhow alarm/alert systems are designed and implemented.Using a human factors approach, systems can be designedguided by our knowledge of human factors and, specifically,cognitive heuristics and biases in mind to improve usabilityand reduce the likelihood of human error related to alarm/alert fatigue.39 Phansalkar et al40 published a review of the literature that identified numerous human factors that shouldbe considered in the design of alarms/alerts, including, butnot limited to, design (placement, visibility, color), alarm philosophy (logic), and cognitive factors (habituation, heuristics).Evidence-based recommendations to reduce alarm/alert fatigue include the implementation auditory alarms with distinctfeatures, customization of alarms/alerts for individual patients854or clinicians, and consideration of other strategies that reducefrequency and improve the sensitivity of alarms/alerts.22,25,41Recognition-Primed Decision ModelThe RPD model illustrates the decision-making processes of individuals who make difficult decisions when faced with time constraints.5 Similar to the intuitive judgments of System 1, the RPDmodel postulates that complex, time-constrained decisions areheavily based on relevant cues, expectancies, plausible goals,and typical outcomes.42 The RPD model hypothesizes thatpattern recognition or “pattern matching” occurs when anindividual encounters a similar situation and must make aquick decision.5COGNITION AND DECISION MAKING DURINGBARCODE-ASSISTED MEDICATION ADMINISTRATIONThe first step illustrated in the conceptual model (Figure 1) isthe initiation of a task and, in this case, to begin medicationadministration. Following initiation, the nurse engages in initial cognitive processing. Factors believed to influence initialcognitive processing include task/verification characteristics(complexity, difficulty), individual/human factors (knowledge,experience, working memory capacity, cognitive workload,heuristics and biases), and environmental factors (patientstatus, nurse workload, interruptions). Related to the dualprocess theory, specifically, is the presence of heuristics andbiases, considered with individual/human factors, that contribute to intuitive (System 1) judgments.As shown in the conceptual model, the output from theinitial cognitive processing step is a decision to completethe task. In the case of medication administration, cognitiveprocessing likely involves the nurse's situational awareness ofthe patient and medication to be administered, verificationof the rights of medication administration, and initiation ofBCMA. If there is no alert (stimulus) triggered duringBCMA, the nurse completes the medication administrationprocess. If an alert is triggered, it is hypothesized that additional cognitive processing takes place. The same influences(task/verification characteristics, individual/human factors,and environmental factors) continue to impact the secondoccurrence of cognitive processing. With the second occurrence, however, the process of cognition may be slightly different. When an alert is generated during BCMA, the nursemust verify the accuracy of the alert, drawing from previousinformation used during the initial cognitive processing, butalso consider new information. The concept of “expectancyviolation” arises from the RPD model and applies to a situation where cues, expectancies, goals, and actions may havebeen misunderstood.43 If a nurse expects that an alert begenerated, or alternatively, if the generation of an alert doesnot violate the expectancy of the nurse, the outcome of cognitive processes may be to inappropriately override the alert.CIN: Computers, Informatics, NursingCopyright 2021 Wolters Kluwer Health, Inc. All rights reserved.December 2021
IMPLICATIONSThe proposed model is suited for the exploration of factorsthat influence cognition and decision making while using aCDSS. It is established that alarm/alert fatigue contributesto patient harm.44 However, there is a lack of understandingabout the influence of System 1 thinking on clinician cognition when using CDSSs. Specifically, it is important toconsider the influence that heuristics and biases have onclinician decision making, particularly related to the development of alarm and alert fatigue. Therefore, the proposed model illustrates how various stakeholders may goabout beginning to identify heuristics and cognitive biasesthat influence the decision of clinicians to accept or override a CDSS alert and whether heuristics and biases areassociated with inappropriate alert override.Researchers should continue to explore the influence offactors, including heuristics and biases, on the decision of clinicians to accept or override alerts. Additionally, future studies are needed to describe the experience of alert fatigueamong nurses in the acute care setting and the impact of alertfatigue on patient safety and quality of care. Hospital administrators should be aware of environmental factors and notably, workload, as important variables to consider whenlooking for influences on cognition and propensity for System 1 thinking. Building on initial findings, subsequent research should explore the dual process theory and decisionmaking among nurses while using CDSSs, as well as the implementation of human factors approaches to CDSS design.Table 1 displays research questions that can be elucidatedusing the proposed conceptual model to guide study design.An outcome variable of interest related to the explorationof heuristics and biases in decision making is dwell time. Dwelltime was described in an explanatory analysis by McDanielet al45 and is based on timestamps from the EHR or BCMAdata log. Specifically, it is a measurement capturing the lengthof time between when an alert is generated and first appearson the computer screen to when the nurse clicks to overrideor accept the alert. As noted by McDaniel et al,45 dwell timecan illuminate the amount of time spent by the nurse to readand process the alert. Although its utility remains under consideration, dwell time as an outcome variable can be used instudies to identify factors that may influence nurse cognitionand, specifically, the influence of factors on the length of timeTable 1. Research Questions for Future InquiryWhat factors influence nurse cognition, specifically, the decision ofthe nurse to accept or override an alert during BCMA?What factors influence dwell time when alerts are generated duringBCMA?What HFE principles, when incorporated into the design of CDSSalerts, are associated with longer dwell times regardless offrequency of alert?Volume 39 Number 12that elapses between alert generation and when a decision ismade by the nurse to accept or override an alert duringBCMA. Specifically, it may be that new or novel alerts (thosethat have not appeared to the nurse before) are associated withlonger dwell times. This hypothesis is supported by McDanielet al,45 who found that the most frequent alerts had shorterdwell times than alerts that occurred only once. However,while it may be that longer dwell time indicates a more thorough and critical (eg, System 2) evaluation of an alert, furtherexploration of dwell time as an outcome variable and measureof cognitive processing is needed.45 Although further researchis needed, shorter dwell times may signal to hospital administrators that the alarm or alert is not being considered by clinicians as intended. Dwell time or other variables found toinfluence cognition and decision making can be used by hospital administrators in the design and implementation of CDSSs.The granularity of data that are collected through EHRuse is noteworthy and provides opportunity to identify individual, microsystem, and macrosystem factors that impactpatient safety outcomes. Nurse researchers are beginning to utilize large data sets captured by the EHR and linked to humanresources and other clinical databases to examine individualnurse factors and their impact on patient care outcomes.9,46,47For instance, Welton et al9 examined time-referenced data related to medication administration and were able to identifypractice patterns that elucidated clinical decision making bynurses regarding the administration of as-needed (prn) medications. Other proposed benefits of utilizing these linkeddatasets include the ability to calculate the economic valueto nursing care, engage in real-time or near-real time data collection and analysis, and the possibility of using data to identify or predict patient care outcomes.48 It may be possible touse these linked datasets to derive empirical measures forkey concepts in the proposed framework. This would facilitatefurther exploration of factors that influence nurse decisionmaking, to better understand how nurses make decisionsand to leverage this information to improve patient safetyand care outcomes.In addition to quantitative methodologies, qualitativemethodologies can be employed to generate empirical datarelated to key concepts in the proposed framework to supportthe examination of nurse cognition during CDSS use. Forexample, a qualitative approach might include the “thinkaloud” method of interviewing. This qualitative interviewingmethod is a type of cognitive task analysis that requires participants to verbalize their thoughts as they complete a taskor solve a problem and is commonly used to study cognitiveprocessing of clinicians during decision making.49,50Importantly, researchers pursuing either quantitative orqualitative studies to study questions related to cognitive biasduring CDSS use should leverage interdisciplinary teams.Teams can include researchers, clinicians, informaticists,CIN: Computers, Informatics, NursingCopyright 2021 Wolters Kluwer Health, Inc. All rights reserved.855
CONTINUING PROFESSIONAL DEVELOPMENTdata scientists, or analysts, as well as other personnel. Knowledge and expertise in working with large data sets, databasemanagement, and data dictionaries are particularly importantwhen identifying variables of interest, extracting from, andlinking EHR data to other datasets.48 Additionally, researcherswith experience in qualitative methods, and specifically the“think-aloud” method of interviewing, would be an asset tothe interdisciplinary research team.In addition to researchers and hospital administrators, nurseeducators and informaticists can use this model to better understand and identify how various factors influence nurse cognitionand decision making. In particular, these stakeholders can promote awareness among nursing students and registered nursesthat learned heuristics can develop and may lead to inappropriate response to an alarm or alert when using CDSSs.Educational strategies may be implemented that target thedevelopment of heuristics and resulting biases to reducethe occurrence alarm or alert fatigue in the clinical setting.CONCLUSIONSThis article adds to the existing literature by synthesizing theories related to and proposing a conceptual model that canbe used to explore factors that influence nurse cognitionand decision making. The proposed model can be used bymultiple stakeholders and can guide further research, considerations for CDSS design, and the education of nursing students and practicing nurses. Through identifying heuristicsand biases, as well as other factors that influence nurse cognition and decision making, it may be possible implement interventions resulting in better nurse decision making andimproved patient safety and quality of care.References1. Institute of Medicine. To Err is Human: Building a Safer Health System.Washington, DC: National Academy Press; 2000.2. Makary MA, Daniel M. Medical error-the third leading cause of death in theUS. BMJ. 2016;353: i2139. doi:10.1136/bmj.i2139.3. McClelland LE, Switzer FS 3rd, Pilcher JJ. Changes in nurses' decisionmaking during a 12-h day shift. Occupational Medicine (London). 2013;63(1): 60–65. doi:10.1093/occmed/kqs189.4. Potter P, Wolf L, Boxerman S, et al. Understanding the cognitive work ofnursing in the acute care environment. The Journal of Nursing Administration.2005;35(7–8): 327–335.5. Nibbelink CW, Reed PG. Deriving the practice-primed decision model from anaturalistic decision-making perspective for acute care nursing research. AppliedNursing Research. 2019;46: 20–23. doi:10.1016/J.APNR.2019.01.003.quality. The Journal of Nursing Administration. 2018;48(2): 100–106. doi:10.1097/NNA.0000000000000580.10. Bucknall T, Fossum M, Hutchinson AM, et al. Nurses' decision-making,practices and perceptions of patient involvement in medicationadministration in an acute hospital setting. Journal of Advanced Nursing.2019;75(6): 1316–1327. doi:10.1111/jan.13963.11. Thompson KM, Swanson KM, Cox DL, et al. Implementation of bar-codemedication administration to reduce patient harm. Mayo Clinic Proceedings:Innovations, Quality & Outcomes. 2018;2(4): 342–351. doi:10.1016/j.mayocpiqo.2018.09.001.12. Agency for Healthcare Research and Quality. Medication errors and adversedrug events. d-adversedrug-events. Accessed December 19, 2019.13. Higgins LW, Shovel JA, Bilderback AL, et al. Hospital nurses' work acti
Barcode-Assisted Medication Administration (BCMA) is a . Kansas, BCMA was more broadly implemented in acute care settings nationwide beginning in the early 2000s.16 During BCMA, nurses verify the rights of medication administration by scanning the patient's iden-tification band and medication packaging. .