Transcription
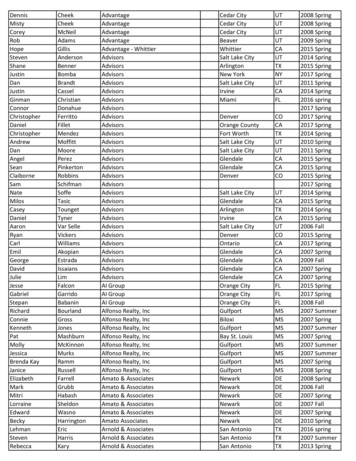
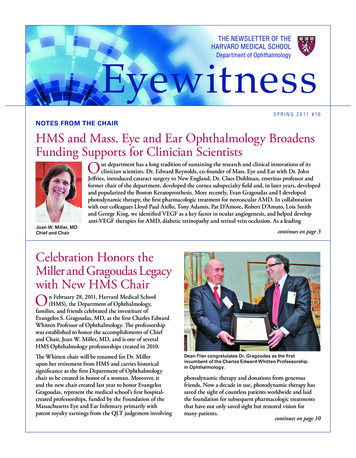
The Newsletter of theHarvard Medical SchoolEyewitnessDepartment of OphthalmologyS P R I N G 2 0 11 # 16notes from the chairHMS and Mass. Eye and Ear Ophthalmology BroadensFunding Supports for Clinician ScientistsOJoan W. Miller, MDChief and Chairur department has a long tradition of sustaining the research and clinical innovations of itsclinician scientists. Dr. Edward Reynolds, co-founder of Mass. Eye and Ear with Dr. JohnJeffries, introduced cataract surgery to New England. Dr. Claes Dohlman, emeritus professor andformer chair of the department, developed the cornea subspecialty field and, in later years, developedand popularized the Boston Keratoprosthesis. More recently, Evan Gragoudas and I developedphotodynamic therapy, the first pharmacologic treatment for neovascular AMD. In collaborationwith our colleagues Lloyd Paul Aiello, Tony Adamis, Pat D’Amore, Robert D’Amato, Lois Smithand George King, we identified VEGF as a key factor in ocular angiogenesis, and helped developanti-VEGF therapies for AMD, diabetic retinopathy and retinal vein occlusion. As a leadingcontinues on page 3Celebration Honors theMiller and Gragoudas Legacywith New HMS ChairOn February 28, 2011, Harvard Medical School(HMS), the Department of Ophthalmology,families, and friends celebrated the investiture ofEvangelos S. Gragoudas, MD, as the first Charles EdwardWhitten Professor of Ophthalmology. The professorshipwas established to honor the accomplishments of Chiefand Chair, Joan W. Miller, MD, and is one of severalHMS Ophthalmology professorships created in 2010.The Whitten chair will be renamed for Dr. Millerupon her retirement from HMS and carries historicalsignificance as the first Department of Ophthalmologychair to be created in honor of a woman. Moreover, itand the new chair created last year to honor EvangelosGragoudas, represent the medical school’s first hospitalcreated professorships, funded by the Foundation of theMassachusetts Eye and Ear Infirmary primarily withpatent royalty earnings from the QLT judgement involvingDean Flier congratulates Dr. Gragoudas as the firstincumbent of the Charles Edward Whitten Professorshipin Ophthalmology.photodynamic therapy and donations from generousfriends. Now a decade in use, photodynamic therapy hassaved the sight of countless patients worldwide and laidthe foundation for subsequent pharmacologic treatmentsthat have not only saved sight but restored vision formany patients.continues on page 10
I n t h e S p ot l i ghtIn this issue:Notes from the Chair. . . . . . . . . . . CoverCelebration Honors the Millerand Gragoudas Legacy withNew HMS Chair. . . . . . . . . . . . . . . CoverDavid G. Hunter, MD, PhD,Promoted to Professor ofOphthalmology . . . . . . . . . . . . . . . . . . . 2Meet Our Scholars. . . . . . . . . . . . . . . . . 3Ophthalmic Pathology ServiceInvigorates Teaching, Research,Patient Care . . . . . . . . . . . . . . . . . . . . . . 5Anti-VEGF Therapies RedefiningTreatment for Diabetic MacularEdema. . . . . . . . . . . . . . . . . . . . . . . . . . . 6Ophthalmology Faculty ExploreAcademic Opportunities InShanghai . . . . . . . . . . . . . . . . . . . . . . . . 7HMS Ophthalmology GlaucomaCenter of Excellence: Partneringfor a Cure. . . . . . . . . . . . . . . . . . . . . . . . 8News from All Over. . . . . . . . . . . . . . . 11Published three times a year:Joan W. Miller, MD, EditorJudy Gibian, Staff WriterSuzanne Ward, Staff Writer2E y e witn e s sDavid G. Hunter, MD, PhD, with pediatric patient.David G. Hunter, MD, PhD, Promotedto Professor of OphthalmologyDavid G. Hunter, MD, PhD, the Richard Robb Chair in Ophthalmologyand Ophthalmologist-in-Chief at Children’s Hospital Boston, was recentlyhonored with an HMS promotion to Professor of Ophthalmology. Dr. Hunterreceived his MD and PhD degrees at Baylor College of Medicine, and completedan ophthalmology residency at Massachusetts Eye and Ear Infirmary/HMS.Dr. Hunter furthered his training with a pediatric ophthalmology fellowshipat Wilmer Eye Institute of Johns Hopkins Medical School, where he joined thefaculty in both Ophthalmology and Biomedical Engineering. He returned toHMS in 2002 as Ophthalmologist-in-Chief of Children’s Hospital.During his tenure, Dr. Hunter has encouraged both clinical excellence andresearch innovation within the Ophthalmology division at Children’s. Hecreated the first International Fellowship in Pediatric Ophthalmology and led thedevelopment, initiation and funding of the Children’s Hospital Boston VisitingProfessor Lecture Series. Since its establishment in 2006, this lecture serieshas brought four to six internationally recognized visiting professors to Bostoneach year.A devoted mentor and teacher, Dr. Hunter was nominated for the Harvard MedicalStudent Teaching Award in 2004, and received the Robert Petersen PediatricOphthalmology teaching award in 2005. As HMS Ophthalmology Vice Chair forPromotions and Reappointments, Dr. Hunter facilitates the academic advancementof the department faculty across all HMS affiliates. He has also added to the wealthof academic strength and collaboration within the Department by rigorouslyrecruiting dual-fellowship trained faculty combining pediatric ophthalmology andsubspecialty training in neuro-ophthalmology and oculoplastics.continues on page 7
Meet Our ScholarsNotes from the Chair, continued from coverdepartment in the country, we firmly believe that clinician scientists are key totransformational medicine, working with basic scientists to provide the clinicalcontext of scientific endeavor and to aide in its translation.Yet, despite the national desire to support translational research, fundingfor clinician scientists remains limited and difficult to obtain, leaving manyto wonder if it can remain a viable career path. Seven years ago, we began aconcerted mission to develop and encourage junior faculty to pursue researchcareers. Under the leadership of Dr. Reza Dana, we were awarded one of thefew National Eye Institute (NEI) K12 grants for the Harvard Vision ClinicalScientist Research Program, enabling us to recruit, train and support firstrate clinician scientists in a mentored program that aims to develop theirtranslational and clinical research interests into meaningful advances forpatients. We have enrolled seven remarkable junior faculty to date, and theprogram was recently renewed by NEI for another five years.Scholar Funds Support Clinician ScientistsWhile the K12 program provides an excellent mentoring program to supportthe early career development of clinician scientists, the path is still a difficultone, given that the average age of a researcher receiving their first-time RO1or equivalent award is 42. At Mass. Eye and Ear, we have been fortunateto establish Scholar funds that provide salary support to clinician scientistfaculty and, in particular, to junior faculty for intermediary support betweenmentored K awards and independent funding. The award and continuingroyalties that come to Mass. Eye and Ear from our successful QLT judgment –itself the outcome of successful clinician scientist research – have funded muchof this scholarship support. Two named retina scholar positions have beenestablished from the research laboratory royalties of Dr. Gragoudas and myself;and three additional scholar positions have been established with departmentroyalties. In addition, we have been able to establish a scholar program inthe Cornea Service with a portion of the proceeds from sales of the BostonKeratoprosthesis, the work of Dr. Claes Dohlman. The first incumbents havebeen placed in these six scholar positions. (See “Meet Our Scholars, at right.)Multi-Purpose Funding Boosts Salaries, Programs andAcademic PursuitsScholar funds are just one way in which the HMS OphthalmologyDepartment supports research and education in the department. Ourdepartment now offers annual financial support for Mass. Eye and Ear researchfaculty to assist with expenses associated with professional advancement,such as meeting attendance and publication expenses. Furthermore, we haveadopted an approach to provide bridge funding to research faculty at Mass.Eye and Ear: salary support for a number of years, which can be used on aflexible basis as needed while alternatives are aggressively pursued.In some instances, we also target funds to support individual researchprograms. These funds are multi-purpose in nature and have been used, forexample, to support stem cell studies in our Cornea Service; translationalresearch in our Glaucoma and AMD Centers of Excellence; and will soonhelp to make available our highly innovative and interactive, cataracttraining software program – the Mass. Eye and Ear Cataract Surgery Trainerdeveloped by Drs. Bonnie Henderson, Carolyn Kloek, John Loewenstein, andcolleagues – to residency programs nationwide.We also work closely with our scientists to seek out and apply for outsidefunding from federal, academic, industry and private sources. In 2008,Ivana K. Kim, MDEvangelos S. GragoudasDistinguished Scholar in RetinaResearchHMS Assistant Professorof OphthalmologyCo-Director, HMS OphthalmologyAMD Center of ExcellenceDirector, AMD Unit, Mass. Eyeand Ear InfirmaryDr. Kim joined the full-time faculty of Mass. Eye andEar’s Retina Service in 2003. As a key member of theangiogenesis research team at HMS/MEEI, she hasbeen involved in numerous clinical and translationalstudies directed toward the development of newtherapies for age-related macular degeneration(AMD) and other ocular conditions involvingchoroidal neovascularization. Her preclinicalresearch utilizes genetic analysis to identify bothrisk factors and new pathways associated withpathological disease processes investigating bothmelanoma and macular degeneration. One area ofrecent focus explores the use of animal models tostudy the pathophysiology and progression of dryAMD to geographic atrophy and blindness. She isalso working with colleagues to test the safety andefficacy of antiangiogenic therapies for a growingnumber of ocular diseases.Dr. Kim’s research has been funded by a grant fromResearch to Prevent Blindness for her studiesinvestigating the genetic basis of uveal melanomafor which she more recently received a 2-yearR21 (exploratory/developmental research) grantfrom the National Cancer Institute at NIH. She wasalso recently awarded a 2-year, Clinical ResearchAgreement from Genentech to conduct a Phase Ib/IImulti-center investigation of the safety, tolerabilityand evidence of beneficial activity of intravitrealinjections for patients with geographic atrophy.Demetrios G. Vavvas, MD, PhDJoan W. Miller Scholar inRetina ResearchHMS Assistant Professor ofOphthalmologyDr. Vavvas is on the full-timefaculty of MEEI’s Retina Service.His laboratory research spansneuroprotection, ocular cancer,angiogenesis, retinopathy of prematurity anddiabetes. He is participating in ongoing studiesto find safer and less toxic therapies for treatingretinoblastoma in infants, and aims to developtherapies that prevent the growth of primaryand metastatic tumors in uveal melanoma. Incollaboration with Dr. Joan Miller, he is alsopursuing neuroprotection strategies that canprevent photoreceptor death, and potentiallypreserve vision in many retinal diseases.He has been the recipient of several grants,including a Boston Area Diabetes EndocrinologyResearch Center pilot grant award (2008-2010) anda Fight For Sight Grant-In-Aid (2008-2009) for hisinvestigative work on the role of AMP dependentkinase in diabetic retinopathy. In collaboration withDrs. Miller and Kim, he has received funding todevelop the first dry AMD primate model.continues on page 4continues on page 4S P R IN G 2 0 1 1 # 1 63
Scholars, continued from page 3Ula V. Jurkunas, MDDepartment ofOphthalmology ScholarHMS Assistant Professorof OphthalmologyAssistant Scientist,Schepens Eye ResearchInstituteDr. Jurkunas is a full-timemember of MEEI’s Cornea and RefractiveSurgery Service and Assistant Scientist atSchepens Eye Research Institute (SERI). Herstudies focus on translational research relatedto corneal dystrophies and stem cell-basedtherapies for other diseases of the cornea.In 2006, she was one of the first HMS juniorclinician scientists to receive a K12 HarvardVision Clinical Scientist Development Programaward, monies that supported her awardwinning research into the pathophysiology ofFuchs Endothelial Corneal Dystrophy (FECD).Today, Dr. Jurkunas is independently fundedat SERI where she is principal investigator ofan NIH-funded RO1 research grant that willfurther her studies of FECD. In addition, hertranslational research to bring corneal stem celltherapy into clinical practice has been acceptedby the Production Assistance in CellularTherapies program of the National Heart Lungand Blood Program.Lucia Sobrin, MD, MPHDepartment ofOphthalmology ScholarHMS Assistant Professorof OphthalmologyDirector, Morse LaserCenter, Mass. Eye andEar InfirmaryDr. Sobrin is a fulltime clinician scientist with the Retina andUveitis Services. She, too, joined Mass. Eyeand Ear in 2006 with an award from the K12Harvard-Vision Clinical Scientist DevelopmentProgram. One of Dr. Sobrin’s primary researchinterests is elucidating the genetics of diabeticretinopathy in African Americans. She was thefirst ophthalmologist to be awarded fundingunder the HMS Catalyst Grant Program, andis principal investigator for a study entitled“Epidemiology and Genetics of DiabeticRetinopathy in the Jackson Heart Study.”Dr. Sobrin has received several grants tosupport her work including, most recently,a major grant from the American DiabetesAssociation for her research project,“Admixture mapping to discover diabeticretinopathy genes in African Americans.”This year, she has been honored with theARVO/Alcon Early Career Clinician ScientistResearch Award.continues on page 54E y e witn e s sNotes from the Chair, continued from page 3the HMS Department of Ophthalmology was the number one universityrecipient of NIH funding in the country by a wide margin (OphthalmologyTimes, October 2009), attesting to both our sheer doggedness in proposalsubmittals and the innovative, high caliber work of our researchers. Tocontinue on this positive trajectory, we’ve recently staffed up our researchprogram areas to provide additional administrative assistance to faculty withfunding/application processes, and to help coordinate our robust clinicalresearch activities.Faculty Support a Major PriorityRecognizing and supporting the incredible talent within our ranks has beena major priority throughout my tenure. We have put aggressive mechanismsin place to facilitate promotions and appointments of our faculty throughan expanded mentorship program, professional development workshops andleadership seminars. Two years ago, I appointed Dr. David Hunter as ViceChair of Promotions and Reappointments to oversee these efforts and furtherhone our organizational goals. So far, these concerted efforts have culminatedin seven professorial promotions, as well as numerous junior facultyadvancements. Another important venue of support is the establishment ofendowed professorships. Not only is this the highest honor we can bestowupon a faculty member, but it gives the incumbent the freedom and flexibilityto pursue his or her specific areas of interest. In just the last year, we haveestablished five additional professorships; two of these – the Charles EdwardWhitten and the Stelios E. Gragoudas Professorships – were funded by theFoundation of the Mass. Eye and Ear Infirmary from our QLT royaltiesand generous donors, representing the first primarily hospital-endowedprofessorships in the medical school’shistory – testimony to the strength of The historical uncertaintyour partnership and future endeavorsof funding makes us morebetween Mass. Eye and Ear anddetermined than ever toHarvard Medical School.Our Mission of ExcellenceContinuesensure that the efforts ofour clinician scientists arerigorously supported asthey fulfill the department’stripartite mission.The historical uncertainty offunding makes us more determinedthan ever to ensure that the effortsof our clinician scientists arerigorously supported as they fulfillthe department’s tripartite mission. Our faculty is highly motivated in theiracademic work, often eschewing more lucrative, private-sector salaries topursue passionately research that can vastly improve the lives of countlesspatients, and to concentrate on training the next generation of ophthalmicleaders. Their dedication and commitment deserves first-rate support fromour academic leaders and community. In this regard, we are very fortunateto have excellent relationships with generous organizations and donors whoseon-going commitment to eye research and education support the faculty incritical ways and make their work possible. We also enjoy the unswervingloyalty of our hospital and academic leadership as we have navigateddifficult and prolonged legal battles over royalty rights, charted plans forunprecedented expansion, and sought to raise the visibility and recognitionof the department. This multi-faceted and emphatic commitment to facultyresearch support is pivotal to advancing ophthalmic science, and to ourultimate goal of eradicating blinding diseases in this century. n
Ophthalmic Pathology ServiceInvigorates Teaching, Research,Patient CareFrederick A. Jakobiec, MD, DSc,the Henry Willard WilliamsProfessor of Ophthalmology,Emeritus and Professor ofPathology, Emeritus, was Chiefand Chair at Harvard MedicalSchool/Massachusetts Eye and EarInfirmary from 1989 until 2002,when ill health made it necessaryfor him to step down. Happily forus, he made an excellent recoveryand, at the invitation of Dr. JoanMiller, returned in July 2007as director of the reorganizedand expanded David G. CoganLaboratory of OphthalmicPathology at Mass. Eye and Ear.Under Dr. Jakobiec’s direction,the Cogan Laboratory cooperatesextensively with the MassachusettsGeneral Hospital (MGH)A teaching moment: Dr. Frederick JakobiecPathology Service to provideand Ophthalmic Pathology Fellows Mariaenhanced diagnostic services,Kirzhner, MD and Fouad Zakka, MD(background) use a multi-headed, lightresident and fellow teaching, andmicroscope to examine a specimen during aclinico-pathology research projects.read-out session in the Cogan Laboratory.Additionally, an alliance withBoston University (BU) Department of Ophthalmology allows BU residentsto rotate through the Cogan Laboratory. One of the projects Dr. Jakobiecdeveloped upon his return was a pathology-based, visiting professor lectureseries covering all aspects of ophthalmic pathology. This popular teachingvenue, now in its fourth year, attracts speakers who are national leaders inophthalmic pathology. The lectures are open to all HMS and BU MedicalSchool residents and fellows in ophthalmology and pathology.Another aspect of the eye pathology education program is OphthalmicPathology Rounds. Held once a month in the evening, the rounds arecomprised of a comprehensive review of cases presented by residentsand fellows on all subspecialty services. They are offered as “unknowns”to Dr. Jakobiec who covers the clinical features, differential diagnosis,pathologic features and management issues reflected in each case. Traineesand faculty from all HMS affiliate institutions are welcome and oftencomprise part of the audience. nFor information on Ophthalmic Pathology Rounds dates, locations,and times, contact the Mass. Eye and Ear Ophthalmic Pathology officeat 617-573-3319 or go to ology and click on “Meetings and Courses” for a monthlycalendar of educational events, rounds and conferences.Scholars, continued from page 4Louis R. Pasquale, MDDistinguished Scholar inOphthalmologyHMS Associate Professor ofOphthalmologyCo-Director, HMS OphthalmologyGlaucoma Center of ExcellenceDirector, Glaucoma Service,Mass. Eye and EarDirector, Ocular Telemedicine Program, Mass. Eye and EarAssociate Epidemiologist, Channing Laboratory,Brigham and Women’s HospitalDr. Pasquale is the director and a full-time facultymember of Mass. Eye and Ear’s Glaucoma Service.Dr. Pasquale’s research focuses on early detection andan improved understanding of disease pathogenesis inprimary open-angle glaucoma (POAG). He is principalinvestigator of several NIH-funded studies that examinethe gene-environment interactions related to the diseasethat aim to reveal factors that increase intraocularpressure (IOP) in POAG, as well as target novel factorsthat contribute to optic nerve degeneration in POAG.Together with Janey Wiggs, MD, PhD, Dr. Pasquale isco-leading the NEIGHBOR Consortium – a multi-centercohort study that includes 8,000 glaucoma cases andcontrols, gathered from the Mass. Eye and Ear, theNurses’ Health Study (NHS), the Health ProfessionalsFollow-up Study, and eight other institutions. Fundedthrough the National Human Genome Research Institute,this work has generated the largest known group ofPOAG cases and, long-term, seeks to identify the fullcomplement of genes, gene-gene and gene-environmentinteractions associated with POAG. This study has alsoformed the basis for subsequent projects includinga genetic epidemiology study that demonstrated anassociation between gene variants and hormonereplacement therapy in POAG. Additional studieshave identified candidate genes for pseudoexfoliationsyndrome, and have revealed trends in exfoliationglaucoma that highlight the importance of geneenvironment interactions in glaucoma.Pedram Hamrah, MDHenry Allen Cornea ScholarHMS Assistant Professor ofOphthalmologyDirector, Ocular Surface ImagingCenter, Mass. Eye and Ear InfirmaryDr. Hamrah is a full-time facultymember of MEEI’s Cornea andRefractive Surgery Service. Hedirects the newly formed Ocular Surface ImagingCenter, where he is interested in developing live imagingtechniques and using in vivo confocal microscopy (IVCM)for image-guided therapy.Dr. Hamrah’s research focuses on immune cell traffickingin immune and infectious diseases of the cornea,including viral and microbial keratitis, corneal transplanttolerance and rejection, neurotrophic keratopathy andocular surface disease. From 2008 through May 2010,his research was supported by a K12 Harvard-VisionClinical Scientist Development Program award; this wasfollowed by an individual K08 award from the NEI for hisbasic science work on the immunology of corneal antigenpresenting cells. Recent research funding includes aGrant-in-Aid award from Fight for Sight, and two grantawards from Alcon Research, LTD.S P R IN G 2 0 1 1 # 1 65
E yes on R ese a rc hAnti-VEGF TherapiesRedefining Treatmentfor Diabetic MacularEdemaFor the first time in 30 years, some peoplesuffering from central retinal swelling, ordiabetic macular edema (DME), may be able tosubstantially improve their vision thanks to novelpharmacologic therapies already FDA-approvedfor treating the “wet” form of age-related maculardegeneration. A recent landmark clinical trial,sponsored by the Diabetic Retinopathy ClinicalResearch Network (DRCR.net), has shownthat the anti-vascular endothelial growth factor(VEGF) medication ranibizumab (Lucentis ) –Jennifer Sun, MD, PhD with diabetes patient Kevin England, a participant incombined with either prompt or deferred laserthe DRCR.net-sponsored Diabetic Macular Edema study. Mr. England begantreatment – significantly improved vision intreatment in 2008 for his left eye. Thirteen months into the study, visual acuitymany patients with DME. Findings from thein his eye had climbed 15 lines on the eye chart, giving him better-than-averagestudy demonstrate that the new therapy mayvision of 20/16.prove even more beneficial thanFew participants experiencedstandard laser photocoagulation byThe results from this clinicaleye-related complications andfurther reducing diabetes-associatedthere were no serious systemicswelling in the retina. The newtrial demonstrate that anti-VEGFevents such as heart attack ortherapy is quickly emerging as atherapies for treating diabetic macularstroke associated with treatment.potential and powerful first-lineedemacanberemarkablyeffective,Results from the trial weretreatment for people with thepublished online in April 2010providing substantial improvementsdisease. Dr. Lloyd P. Aiello, HMSin Ophthalmology. Two yearOphthalmology Vice Chair forin vision and substantial reductionsfollow-up data are available forCenters of Excellence, Director ofin vision loss.57 percent of study participantsthe Beetham Eye Institute at Joslin—Dr. Lloyd P. Aielloand these results are consistentDiabetes Center, and the inauguralwith the one-year findings.chair of the NIH-funded DRCRnetwork, is a lead author of the study.“The results from this clinical trial demonstrate that anti-“”The ongoing, five-year study involves a total of 854 eyes of691 people diagnosed with type 1 or 2 diabetes and diabeticmacular edema involving the retinal center. At one year offollow-up, participants who received anti-VEGF therapygained an average of nine letters (nearly 2 lines) in visualacuity, a three-fold improvement over laser treatment alone.The percentage of patients who achieved at least two linesof vision gain jumped dramatically, from 28 percent toapproximately 50 percent with anti-VEGF treatment (withprompt or deferred laser) compared to laser treatment alone.Conversely, the number of individuals treated with antiVEGF medication versus laser alone who experienced twoor more lines of vision loss also fell sharply from 13 percentto fewer than 5 percent of patients, representing a significantreduction in the number of people who experiencedadverse effects.6E y e witn e s sVEGF therapies for treating diabetic macular edema can beremarkably effective, providing substantial improvementsin vision and substantial reductions in vision loss,” saidDr. Aiello. “Anti-VEGF treatments represent a full benchto‑bedside cycle of translational research and, for thefirst time in more than a quarter-century, offer a new andpowerful method for restoring sight to perhaps millions ofpeople whose vision might otherwise be compromised bydiabetic macular edema.”Initially designed as a three year study, involving 52 siteswithin the DRCR network, the trial – now in year three –has been extended to five years and is supported by theNational Eye Institute and the National Institute of Diabetesand Digestive and Kidney Diseases, part of the NationalInstitutes of Health. n
David G. Hunter, continued from page 2Dr. Hunter is best known for his expertise in complexstrabismus in adults and children. He is exploring andpublishing innovative techniques in strabismus surgeryincluding the “short tag noose” adjustable suture, andtransposition procedures for paretic strabismus. Hisresearch is focused on developing more accurate ways tohelp pediatricians identify eye problems in children.Dr. Hunter collaborates with Elizabeth Engle, MD, HMSProfessor of Neurology and Ophthalmology, HowardHughes Medical Institute Investigator, and a worldrenowned strabismus pioneer and geneticist, who identifiedgenetic mutations that cause congenital fibrosis of theextraocular muscles (CFEOM), a rare and complex ocularmotility disorder. Drs. Hunter and Engle have establishednew clinical systems and protocols for studying the geneticsof common strabismus disorders, including simple esotropia,exotropia and anisometropic amblyopia. These newprotocols – which include clinical exams and sampling ofaffected and non-affected family members to ensure properphenotyping – will serve as a model for ongoing and futuregenetic studies at HMS affiliates.A preeminent expert in optics and refraction, Dr. Hunterdelivers lectures around the world (and via podcast) and hasauthored numerous scientific articles, editorials, and bookchapters. He co-authored Last Minute Optics, a widely usedoptics review book, and serves as Editor-in-Chief of Journalof the American Association for Pediatric Ophthalmology andStrabismus. For his outstanding contributions to clinicalophthalmology, Dr. Hunter has received numerous honors,including the Richard Starr Ross Clinician Scientist Awardfrom Johns Hopkins University and the Research to PreventBlindness Lew R. Wasserman Merit Award. nOphthalmology FacultyExplore AcademicOpportunities inShanghaiThe HMS Department of Ophthalmologycontinues to nurture global partnershipsin Aravind and Singapore, and explore newopportunities for collaboration and outreach. LastOctober, a group of five HMS faculty members –including Drs. Joan Miller, John Loewenstein,Evangelos Gragoudas, Janey Wiggs, and Ivana Kim,along with Ophthalmology Vice President JavierBalloffet – traveled to China on an internationaloutreach trip to the Shanghai Eye and ENT hospitalat Fudan University. The purpose of the five-daytrip was to explore potential research collaborationswith Shanghai colleagues, and provide them withinformation and insight on how to further developa residency training program within the University’shealth care system. The group received a tour ofthe Shanghai hospital, and enjoyed presentationson its clinical and research efforts. For their part,HMS faculty offered an overview of ongoing clinical research efforts within the HMS Department, including glaucoma, retina,ocular cancer and genetics projects. They also provided details about the organization and structure of the HMS ResidencyTraining Program, innovations to the curriculum, and how trainees can enhance the patient experience.Participants on all sides have expressed their appreciation for the frank exchange of information, and are now formulatingplans for further collaborative work, including a joint grand rounds teleconference. In early May, HMS Ophthalmologyfaculty welcomed a five-member team from Shanghai Eye and ENT Hospital. During their eight-week visit, team members –who specialize in glaucoma, retina, cornea and cataracts – are witnessing our resident and fellow training programs, andparticipating in a full rang
Director, AMD Unit, Mass. Eye and Ear Infirmary Dr. Kim joined the full-time faculty of Mass. Eye and Ear's Retina Service in 2003. As a key member of the angiogenesis research team at HMS/MEEI, she has been involved in numerous clinical and translational studies directed toward the development of new therapies for age-related macular .