Transcription
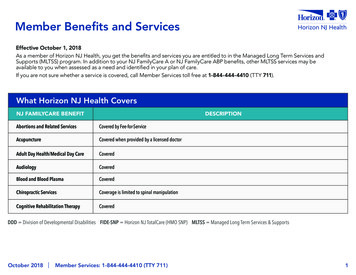
6/26/2014Managed Long Term Servicesand Supports (MLTSS)Business ProcessOffice of Community Choice OptionsHospital and Nursing FacilityMLTSS Business Process OCCOJune 20141Managed Long Term Services and SupportsObjective: Overview of New Jersey FamilyCare Role of Managed CareOrganizations for Medicaidenrollees Role of OCCO for Medicaidpending or non-managed caremembersMLTSS Business Process OCCO June 201421
6/26/2014New Jersey Family Care MLTSSNJ’s Medicaid Program NJ Family Care NJ Family Care Managed Care deliverscoordinated health care services and supportsthrough a network of providers.Delivery of all of an individuals' Medicaidbenefits through one organizationNJ has chosen to provide Medicaid Long TermServices and Supports (MLTSS) through NJFamily Care Managed Care and PACE programsThis is called NJ Family Care Managed LongTerm Services and Supports (MLTSS)MLTSS Business Process OCCO June 20143MLTSSMLTSS Policy and Philosophy A MCO managed care delivery systemMLTSS- will coordinate long term servicesand supports for eligible Medicaidbeneficiaries.Provides a comprehensive menu ofservices options across beneficiary groupsand care settings.Coordination of providers, services, andsupports.Services and Supports can be provided invarious settings including Community, NF,SCNF, Assisted Living (AL, CPCH, ALP, AFC),and Community Residential Services (CRS).MLTSS Business Process OCCO June 201442
6/26/2014MLTSS NJ Family Care MLTSS is the consolidation of DoAS and DDS Waiversincluding: Global Options(GO) Traumatic Brain Injury(TBI) Community Resources for Persons with Disabilities (CRPD) AIDS Community Care Alternatives(ACCAP)All of the above waivers will now be MLTSSNo change in waiver eligibility Clinical and FinancialBroader array of service optionsNo Waiver slot limitationsMLTSS Business Process OCCO June 20145MLTSS for Nursing Facility (NF)and Special Care Nursing Facility (SCNF) Populations1.2.3.Individuals entering a NF or SCNF afterJuly 1, 2014 will be required to enroll inManaged Care.Individuals in a NF or SCNF who becomeMedicaid eligible after July 1, 2014 will berequired to enroll in Managed Care.Those in a NF or SCNF prior and eligiblefor Medicaid prior to July 1, 2014 will notbe enrolled in an MCO or MLTSS unlessthere is a change in placement.a.Any non-hospital change in placement willrequire a new PAS and MCO enrollmentMLTSS Business Process OCCO June 201463
6/26/2014MLTSS vs FFS Once an individual is enrolled inManaged Care, they always remainin Managed Care and outside of theFee for Service (FFS) systemregardless of placement. Medicaid State Plan Services areavailable FFS during gap betweenMedicaid Eligibility and MCOEnrollment.MLTSS Business Process OCCO June 20147Business Process forMedicaid Managed Care MembersMedicaid Eligible with MCO Enrollment OCCO will not conduct NF LOC evaluations for MCO Medicaidrecipients in a Hospital, NF, or SCNF settingThe Hospital shall receive all NF stay certifications from theindividual’s MCO.The Nursing Facility/SCNF will receive all NF/SCNF staycertifications from the individual’s MCO. The MCO is responsiblefor Prior Authorization and payment.Upon determination of MLTSS, the MCO is responsible for CareManagement and completing the NF LOC assessment. NF LOC isrequired when:1. The individual is deemed NF custodial care – rehab hasbeen discontinued and there is no expectation ofdischarge.2. The individual is discharging to the community and is inneed of MLTSS services upon discharge3. Annually for MLTSS membersMLTSS Business Process OCCO June 201484
6/26/2014Business Process forMedicaid Eligible without MCO Enrollment (FFS)Potentially eligible for Medicaid within 180 daysMedicaid Eligible, or potentially eligiblewithin 180 days, without MCO Enrollment The Hospital may request an E-ARC from OCCO whichwill serve as a temporary 30 day PAS. It will be the NF’sresponsibility to request a formal on-site assessment byOCCO dependent upon length of stay per usualprotocols. PAS should not be requested until Day 21. OCCO will assess and counsel individual on autoenrollment process. Once financial and clinical eligibilityis determined, the individual will be eligible for Fee ForService in the NF until MCO enrollment occurs. NJ Medicaid Fee For Service will be payor in the NF untilMCO enrollment occurs as long as a valid PAS is on file.MLTSS Business Process OCCO June 20149Medicaid Managed Care Members in Hospital Hospital will determine ifpatient is enrolled inMedicaid MCO. If enrolled in Medicaid MCO– MCO conducts the PriorAuthorization.– Hospital will get the PriorAuthorization from the MCO.– MCO will conduct a NF LOCassessment upon conclusionof rehab or upon discharge ifMLTSS needs identifiedMLTSS Business Process OCCO June 2014105
6/26/2014Medicaid pending Members in Hospital Non-Medicaid – will requireMedicaid within 180 days thehospital will:– Refer individual to CWA/ADRC– Utilize the EARC ScreeningprocessMLTSS Business Process OCCO June 201411Medicaid FFS in Hospital If individual is Medicaid Fee for Servicethe hospital will:– Verify Medicaid Fee for Service with noMCO enrollment– Utilize EARC screening processMLTSS Business Process OCCO June 2014126
6/26/2014NF Stays - Who Pays?Medicaid Eligible with MCO Enrollment MCO Medicaid MCO will prior authorize andprovide payment.No PAS will be completed until custodial care isreached.Medicaid Eligible without MCO Enrollment(FFS) New to Medicaid (pending) OCCO will conduct PAS.OCCO must be notified of NF to NF or NF- hospital todifferent NF so MCO can occur.–FFS Medicaid Individuals in need of MLTSS services upon dischargeto community require an IDTMLTSS Business Process OCCO June 201413Medicaid Managed Care Members in a Nursing Facility MCO will be the payor source from dayof admission. Managed Care Organization isresponsible for authorizing the servicebenefits for up to 180 days. After 180 days or end of rehab services,the NF stay becomes custodial care andthe member is now eligible for MLTSS. Under MLTSS, the MCO is responsiblefor Care Management and NF LOCannual assessmentsMLTSS Business Process OCCO June 2014147
6/26/2014Medicaid FFS Members in a Nursing FacilityMedicaid Pending in a Nursing Facility Upon admission to the nursing facility acompleted Status Notification Form (LTC-2) willbe sent to OCCO. The LTC-2 will be utilized fornotification of Admission, Termination, PASRequest , and Transfers. The LTC-2 provides the information to OCCO toinitiate the NF LOC process. Upon determination of both Clinical andFinancial eligibility, MCO auto-enrollment will betriggered NJ has a 2 year Any Willing Provider, AnyWilling Plan provisionMLTSS Business Process OCCO June 201415Business Process forMedicaid FFS MembersMedicaid FFS members in NF/SCNF A change in placement setting requires a new PAS. Theseindividuals will be triaged for MLTSS. OCCO is to be notifiedof Transfers by the NF so that OCCO can complete anassessment which will trigger enrollment process in MLTSS ifappropriate.o NF to NFo NF to SCNFo SCNF to NFo SCNF to Different SCNFo Hospital stay does not trigger a new PAS if individual returns to thesame facility.MLTSS Business Process OCCO June 2014168
6/26/2014E-ARC Target PopulationWhat does MLTSS Mean to the EARC Business Process? Individuals now on Medicaid Managed Care will no longerqualify for an EARC PAS. MCO will be responsible forauthorizations of NF stay. EARC will be for Medicaid Pending or Medicaid FFS only. Individuals currently in an acute non-psychiatric hospital setting whoare potentially Medicaid eligible within 180 days, and entering aMedicaid Certified Nursing Facility, or Special Care Nursing FacilityVentilator Unit, with an expectation of billing to Medicaid for all orpart of the stay.Individuals currently in an acute non-psychiatric hospital setting whoare Medicaid eligible without MCO enrollment, and entering aMedicaid Certified Nursing Facility, or Special Care Nursing FacilityVentilator Unit, with an expectation of billing to Medicaid for all orpart of the stay.MLTSS Business Process OCCO June 201417E-ARC Process For EARC target population, the Hospital conduct anE-ARC which will serve as a temporary 30 day PASupon OCCO Authorization. NF is responsible to request a formal on-siteassessment by OCCO dependent upon length of stayper usual protocols. PAS should not be requesteduntil Day 21. OCCO will assess and counsel individual on autoenrollment process. Once financial and clinicaleligibility is determined, the individual will be eligiblefor Fee For Service in the NF until MCO enrollmentoccurs. Upon MCO enrollment, the MCO will be responsiblefor payment and service coordination.MLTSS Business Process OCCO June 2014189
6/26/2014What does MLTSS Mean to the NF/SCNFPopulation? The MCO is responsible for payment andservice coordination regardless of careneeds and placement setting The MCO is responsible for determiningwhen MLTSS is appropriate– Not until Custodial Care or discharging tocommunity with MLTSS needs The MCO will be responsible for CareManagement and NF LOC assessmentannually and for change in condition Discharge to community with MLTSS needswill require NF LOC reassessment and IDTMLTSS Business Process OCCO June 201419What does MLTSS Mean to theCommunity Population?Role of the MCO under MLTSSCare Management:o Authorization, Coordination, and Payment ofAcute, Long Term Services and Supports, andBehavioral service delivery systemso Assessment/Reassessment to establish Level ofCare for NJ Family Care MLTSS members.o OCCO is responsible for determinationo Plan of CareMLTSS Business Process OCCO June 20142010
6/26/2014Business ProcessOffice of Community Choice OptionsQUESTIONSMLTSS Business Process OCCO June 20142111
6/26/2014Department of Human ServicesDivision of Aging ServicesOffice of Community Choice OptionsLTC-2 Notification From Long Term Care FacilityAdmission and Termination of a MedicaidBeneficiaryOCCO June 20141LTC-2 Notification From Long Term Care FacilityGoals and Objective: Overview andChanges to LTC-2Business Process Review of updatedform Role of providerOCCO June 201421
6/26/2014LTC-2 Notification From Long Term Care FacilityCurrent ProcessOverview of LTC-2The Notification from Long Term Care Facility(LTC-2) is the tool used by NJ MedicaidCertified Nursing Facilities to communicate tothe Office of Community Choice Options(OCCO) Regional Office1. Admissions2. Terminations3. Request for PAS4. PASRR status notificationLTC-2 applies only to Medicaid beneficiaries orpotentially eligible Medicaid individuals (within 180days of placement).OCCO June 20143LTC-2 Notification From Long Term Care FacilityCurrent Process Within two (2) working days of a nursingfacility (NF) admission, the NF submits acompleted Status Notification Form LongTerm Care Facility (LTC-2) as perN.J.A.C.8:85 to the Regional Office ofCommunity Choice Options (OCCO): Medicaid and potentially MedicaidIndividuals within 180 days:––––Request for PASNotice of AdmissionNotification of terminationPASRR statusOCCO June 201442
6/26/2014LTC-2 Notification From Long Term Care FacilityMLTSS Impact to LTC-2 Process The form has been updated to reflect the July 1,2014 implementation of Medicaid Managed Careand the Long Term Services and Supports (MLTSS).The Medicaid Managed Care Organization (MCO)will authorize NF placement for its members.Upon identification of MLTSS eligibility, the MCOwill conduct the PAS assessment.– Member must be certified NF Custodial Care(rehab has been exhausted) or– Member is identified for discharge tocommunity and in need of Home andCommunity Based ServicesOCCO June 20145LTC-2 Notification From Long Term Care FacilityLTC-2 Process ChangesThe NF will utilize the LTC-2 for notification toOCCO of: Request for PAS-for New to Medicaid andpending Medicaid beneficiaries– Only individuals not enrolled in an MCO Notice of Admission- no changeNotice of Termination- no changeNotice of Transfer- new changeOther section of the LTC-2 have additionalinformation required:– Patient information– PASRR Status– Request for PASOCCO June 201463
6/26/2014LTC-2 Notification From Long Term Care FacilityLTC-2 Process Changes Patient eligibility information- willcapture patient information on NJ FamilyCare, MLTSS, FFS, and MCO if applicable. PASRR status has been expanded andclarified to capture all outcomes of thePASRR Level I screen and Level II asapplicable. Request for PAS - expanded with newcategories.OCCO June 20147LTC-2 Notification From Long Term Care FacilityLTC-2 Process Changes Request for PAS has beenexpanded with additionalcategories: FFS- Current MedicaidBeneficiary not enrolled inMCO Transfers- Notificationinitiates enrollment processto from FFS to MLTSSOCCO June 201484
6/26/2014LTC-2 Notification From Long Term Care FacilityLTC-2 Process ChangesNotice of Transfers- New Type of Notification to the LTC-2. This willinitiate the MCO enrollment process for individuals who are FFS. Initial transfers of Fee for Service (FFS) Medicaid individuals willnow require a New PAS by OCCO which will trigger MCOenrollment. Types of transfers to be captured:oooooNF to NFNF to SCNFSCNF to NFSCNF to Different SCNFNF/SCNF to Community and in need of Home and Community BasedServices Imperative for OCCO to be notified of Transfers so that OCCOcan complete the assessment which will trigger enrollment inManaged Long Term Services and Supports Waiver (MLTSS).OCCO June 20149LTC-2 Notification From Long Term Care FacilityLTC-2 Process Changes Recap of Changes:– Form has been revised– New to Medicaid or pendingMedicaid will require a PAS fromOCCO.– Individuals enrolled in a MCO , theMCO will do the assessment.– Notice of transfer will trigger a NewPAS and if eligible, the MCOenrollment process to MLTSS Waiver.– Patient information expanded– PASRR section expanded– Request for PAS section expandedOCCO June 2014105
6/26/2014LTC-2 Notification From Long Term Care FacilityRole of the Provider The Nursing Facility will berequired to complete the LTC-2 forall Admission, Termination,Request for PAS , and Transferswithin 2 days of admission to thefacility. LTC-2 must be fully completed tobe processed. NF provider will request the MCOfor authorization for MCOmembers.OCCO June 201411LTC-2 Notification From Long Term Care FacilityOCCO June 2014126
6/26/2014LTC-2 Instructions for Completion Complete each section and fax to theOffice of Community Choice OptionsRegional Office for notice of PAS request,Admission, Termination, and Transfers. Type of Notification: (Check the appropriate box) Request PAS Notice of Admission Notice of Termination Notice of TransferOCCO June 201413LTC-2 Instructions for CompletionSECTION I - PATIENT INFORMATION Social Security Number - patient’s numberNote: The Medicare number is NOT ALWAYS thepatient’s SSN HSP#-12digit Medicaid Number, if availableConfirmed By: Give name of CWA approvingfinancial eligibilityNJ Family Care, MLTSS, FFS, MCO (indicate name)SECTION II - PROVIDER INFORMATION No changes to this sectionOCCO June 2014147
6/26/2014LTC-2 Instructions for CompletionSECTION III - Status PASRR Enter date of PASRR Level I screen.Check the appropriate box: Negative or Positive.If positive, continue to check the appropriate box for the positivescreen.Date of the Positive Level ll evaluation (unless PASRR 30 DayExempted Hospital Discharge)Outcome of PASR Level ll evaluation- check the appropriate box forspecialized services.Changes made only to make the form user friendly.Information to be captured is for Level I and Level IIoutcomes.OCCO June 201415LTC-2 Instructions for CompletionSECTION IV – REQUEST FOR PAS: Check off box indicating type of PAS Request:– Private to Medicaid- Spend downs– PAS Exempt 20days Physician 20 day note must accompany request If the 20 day note is not attached then the referent will benotified and case will not be processed until the 20 daynote is received. If the 20 day note is not submitted , thecase will be processed as a 30 day referral.OCCO June 2014168
6/26/2014LTC-2 Instructions for CompletionSECTION IV – REQUEST FOR PAS (Continued)– Medicare to Medicaid– Out of State Approval Admission – On site PAS requiredto be completed by OCCO within 30 days of request.– SCNF to NF– NF to SCNF– Transfer-Change in Level of Care requires a new PAS. Thetransfer notification will trigger the process for MCOenrollment and move to MLTSS.– EARC PAS- This will require a on site PAS to be completedwithin 30 days of notification.– OtherOCCO June 201417LTC-2 Instructions for CompletionSECTION V - ADMISSION INFORMATIONNo changes Admission Date - the date resident wasadmitted to the facility.For Private to Medicaid cases this date shouldreflect the date the patient was originallyadmitted to the facility. This type of caseshould be sent to the field office 6 monthsprior to the anticipated date of conversion toMedicaid.OCCO June 2014189
6/26/2014LTC-2 Instructions for CompletionSECTION VI - No changesSECTION VII - CERTIFICATION 1. By signing this certification, Provider isattesting that the facility has a “valid PAS onfile”. 2. If is the responsibility of NF to completethis form in compliance with N.J.A.C.8:85.Failure to comply may result inreimbursement issues.OCCO June 201419LTC-2 Instructions for CompletionSECTION VIII – No ChangeCWA USE ONLY (TO BECOMPLETED BY CWAONLY)Section IX – No ChangeGENERAL INFORMATIONFOR NURSING FACILITIESOCCO June 20142010
6/26/2014LTC-2 Instructions for CompletionOCCO June 20142111
Type:New Jersey Department of Human ServicesDivision of Aging ServicesRequest PASNotice of AdmissionNotice of TerminationNotice of TransferNOTIFICATION FROM LONG-TERM CARE FACILITYADMISSION OR TERMINATION OF A MEDICAID BENEFICIARYI.PATIENT INFORMATION1. Name:(Last)2. Social Security No.:(First)5. HSP# (Medicaid) Case No. if applicable:Confirmed By (CWA):3. Sex:NJ Family CareII. PROVIDER INFORMATION1. Provider Number:FemaleMLTSSMale4. Date of Birth//MCO5. Provider Phone #:6.SCNF:2. LTCF Name:3. Address:4. City, State, Zip:III. PASRR STATUS (COMPLETE FOR ALL NEW ADMISSIONS)1. Date of PASRR Level I//Screen:2.Outcome of PASRR Level I Screen – For Positive Screens Check all that ApplyNegativePositive:MIID/DDDMI and ID/DDD30-Day Exempted Hospital Discharge//3. If Positive, Date of PASRR Level II Evaluation:Outcome of PASRR Level II Evaluation - Client Needs Specialized Services:YesNoIV. REQUEST FOR PASPrivate to MedicaidPAS Exempt 20 DaysMedicare to Medicaid-SCNF to NFNF to SCNFOut of State Approval AdmissionCategoricalTransferE-ARC PASOther:V. ADMISSION INFORMATION1. Admission Date:////2. Date of PAS, if applicable:3. Admitted from:Community/Boarding HomePsychiatric Hospital//Private to Medicaid - Anticipated Medicaid Effective Date:HospitalOther LTCFOther(specify)://4. Nameof Hospital/LTCF:Admission Date:Address:5. If admitted from Hospital/LTCF, give the name/address of previous residence (Hospital Name and Address or Home Address):VI. TERMINATION INFORMATION//1. Discharge Date:2. Discharged to:Home-Community (including relative’s home)/ County of residence:County of NF:Facility Name:County of Residence:Other (specify):Telephone Number of Discharge Site://3. Death (Date):In LTCFIn HospitalVII. CERTIFICATION: The facility certifies that the patient will reside only in those areas of the facility which are certified forparticipation in the New Jersey Medicaid Program at the level of care authorized for this patient by the New Jersey Medicaid Program.The facility also certifies that upon discharge to a hospital, the patient’s room/bed will be reserved for the full period of time coveredby the New Jersey Medicaid Bed Reserve Policy. If nursing facility bills Medicaid for long term care services, the person signing this formcertifies that the facility has a valid PAS on file. This form completed by:Phone Number:Date:Name:Title:VIII. CWA USE ONLY/Medicaid Effective Date:Medicaid ONLY (PR-1 Attached)SSI Only (PR-1 Required, Contact DHS)Not Eligible/Transcript Requested - Date:Remarks:Name of Case Worker:LTC-2June 14/COUNTY WELFARE OFFICEStreet Address:/City and Zip:Date:Original-CWACopy-OCCO ROCopy-Provider
INSTRUCTIONS FOR COMPLETION OF THENew Jersey Department of Human ServicesDivision of Aging ServicesNOTIFICATION FROM LONG-TERM CARE FACILITY FOR ADMISSION AND TERMINATIONComplete each section and fax to the Office of Community Choice Options Regional Office for notice ofPAS request, admission, termination, and transfer.Notification -Type of Notification: Check the appropriate box.Request PASNotice of AdmissionNotice of TerminationNotice of TransferSECTION I - PATIENT INFORMATION1. Name - self explanatory2. Social Security Number - patient’s number(Note: the Medicare number is NOT ALWAYS the patient’s SSN)3. Sex - self-explanatory.4. Date of Birth-self – explanatory5. HSP#-12digit Medicaid Number, if available (Confirmed By: Give name of CWA approving financialeligibility) NJ Family Care, MLTSS, FFS, MCO write in name of MCO if know.SECTION II - PROVIDER INFORMATION1. Provider Number-7 digit Molina provider number2- 4 Facility name and address5. Facility Phone number6. SCNFSECTION Ill - Status PASRR1. Enter date of PASRR level1 screen.2. Check the appropriate box, negative or Positive. If positive, continue to check the appropriate box for thepositive screen.3. Date of the Positive Level ll evaluation. (unless PASRR 30 Day Exempted Hospital Discharge)4. Outcome of PASR Level ll evaluation- check the applicable box for yes or no for specialized services.SECTION IV – REQUEST FOR PAS:Check off box indicating type of PAS Request:a. Private to Medicaidb. PAS Exempt 20days (Physician 20 day note must accompany request or PAS will not becompleted).c. Medicare to Medicaidd. Out of State Approval Admission,e. SCNF to NFf. NF to SCNFg. Transferh. EARC PASi. OtherJune 2014 1
SECTION V - ADMISSION INFORMATION(IF THIS IS A TERMINATION, SKIP TO SECTION V)1. Admission Date This is the date resident was admitted to the facility. For Private to Medicaid cases this dateshould reflect the date the patient was originally admitted to the facility. This type of caseshould be sent to the field office 6 months prior to the anticipated date of conversion toMedicaid. Transfer- Check the box yes or no.2. Date of PAS –if applicable3. Admitted from-check appropriate location: Community/Boarding Home Medicare to Medicaid Psychiatric Hospital Private to Medicaid-complete “anticipated Medicaid Effective Date”(Note: It is no longer necessary to attach PA-4) Hospital - Acute Care Hospital or Rehab Hospital-also complete #5 Other Long Term Care Facility (LTCF)-also complete #5 Other (specify)-use this category if above categories do not apply.4. Name and Address of Hospital/LTCF Admission Date-self explanatory5. If admitted from Hosp/LTCF, give the name/address of previous residence-self explanatorySECTION V1 - TERMINATION INFORMATION(IF THIS IS AN ADMISSION, SKIP TO SECTION V)1. Discharge Date-date patient was discharged from the facility2. Discharged to: (check one) Home – Community (including relative’s home)/County of residence Facility (includes NF and AL)/ County of Residence Other (use this category if above categories do not apply. Include name and address of“other”/County of residence Death (Date)-self explanatory Check “In LTCF” or “In Hospital”SECTION V11 - CERTIFICATION1. By signing this certification, Provider is attesting that the facility has a “valid PAS on file”. Complete Name, Title,Phone Number, and DateSECTION VI11 - CWA USE ONLY (TO BE COMPLETED BY CWA ONLY)Section IX - GENERAL INFORMATION FOR NURSING FACILITIES:Send an LTC-2 for all new admissions that have been prescreened, private to Medicaid, out of state and EARC,and PAS Exempt cases. LTC-2 is now required to be sent for PASRR notification regardless of payor source andfor notice of termination.N.J.A.C. 10:63-1.8 (k) mandates the nursing facility (NF) to submit the LTC-2 (formerly MCNH-33) form to theOffice of Community Choice Options Regional Field Office, serving the county where the NF is located withintwo working days of status of admission, termination, request for PAS for all persons who are currently Medicaideligible, or will be eligible within 180 day and for PASRR notification regardless of payor source.June 2014 2
Overview of LTC-2 The Notification from Long Term Care Facility (LTC-2) is the tool used by NJ Medicaid Certified Nursing Facilities to communicate to the Office of Community Choice Options (OCCO) Regional Office 1. Admissions 2. Terminations 3. Request for PAS 4. PASRR status notification LTC-2 applies only to Medicaid beneficiaries or