Transcription
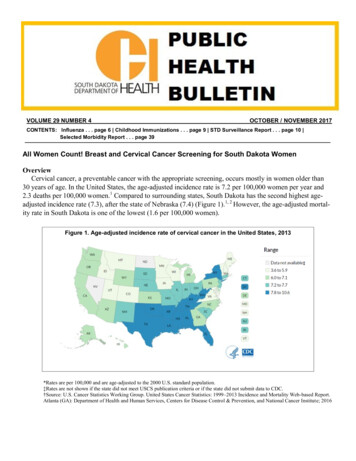
Research Round UpNEWS FOR PATIENTS FROM THE 2013 ASCO ANNUAL MEETINGADVANCED CANCERNew Targeted Immunotherapy Is a PromisingTreatment for Several Advanced CancersCONTENTSA new type of targetedimmunotherapy (calledMPDL3280A) was able to shrinkseveral different types of cancer,including lung, melanoma,kidney, colorectal, and stomachcancers in patients whose cancerhad worsened while receivingother treatments. Immunotherapyis designed to boost the body’snatural defenses to fight thecancer. It uses materials eithermade by the body or in alaboratory to improve, target, orrestore immune system function.Specifically, this new treatmenttargets PD-L1, a protein onthe surface of tumor cells thatprevents the immune system fromfighting the tumor. Basically,this treatment stops PD-L1 fromworking, which then allows thebody’s immune system to fightthe cancer.This study included 140patients with locally advancedcancer (cancer that has spreadnear where it started) ormetastatic cancer (cancer thathad spread to other parts of thebody) that had worsened whilereceiving earlier treatments.Breast Cancer. 2Overall, 29 out of 140 (21%)patients had their tumors shrink,and the treatment has continuedto work for three months tomore than 15 months for 26 ofthese 29 patients. However, thiswas a small, early study, andlarger studies will be needed toconfirm that this immunotherapyworks well.What this means for patients:“We are impressed with howoften and how long this drugworked for patients with verydifficult-to-treat tumors. Sofar, almost none of the patientsthat have had tumor shrinkagehave had their cancers worsen,”said Roy S. Herbst, MD, PhD,Ensign Professor of Medicine andPharmacology at Yale CancerCenter and Chief of MedicalOncology at Smilow CancerHospital at Yale-New Haven inConnecticut. This new treatmentis still being researched, and atest to find PD-L1 on the surfaceof tumors is being developedand studied. It is currently onlyavailable through clinical trials. IfAdvanced Cancer. 1A Word From The President. 2Cervical Cancer. 6Colorectal Cancer. 8Glioblastoma. 9Leukemia.10Lung Cancer.10Melanoma.13Oropharyngeal Cancer.16Ovarian Cancer.17Prevention.18Survivorship.19Thyroid Cancer. 21The ideas and opinions expressed in ResearchRound Up do not necessarily reflect the opinionsof the American Society of Clinical Oncology(ASCO). The information in Research Round Upis not intended as medical or legal advice, or asa substitute for consultation with a physicianor other licensed health care provider. Patientswith health care-related questions should call orsee their physician or other health care providerpromptly and should not disregard professionalmedical advice, or delay seeking it, because ofinformation encountered on the website. Themention of any product, service, or treatment inResearch Round Up should not be construed asan ASCO endorsement. ASCO is not responsiblefor any injury or damage to persons or propertyarising out of or related to any use of ASCO’spatient education materials, or to any errors oromissions.Continued on page 2ASCO is the world’s leading professional organization representing physicians who treat people with cancer.
BREAST CANCERA WORD FROM THE PRESIDENTDear Friends,Welcome to the 2013 American Society of ClinicalOncology (ASCO) Annual Meeting. My themefor this year’s meeting and for my term as thePresident of ASCO is Building Bridges to ConquerCancer. To me, this theme brings together manyof the “bridges” that represent our current needsand challenges in oncology, such as the need for a global oncologycommunity, the need to close the gap in health disparities, the needto connect science with the clinic, and the need to bring the highestquality care to the patient.Every day I see gaps in connecting proven treatments andpreventive measures with underserved populations, and many ofour members working with these populations are frustrated with thechallenges of bringing what they hear at the Annual Meeting to theirpractices at home. To help you, the patient, learn about what the latestin high-quality cancer care means for you, ASCO provides summariesof the research highlighted at the 2013 ASCO Annual Meeting inChicago, Illinois, from May 31 through June 4.I am excited and encouraged by the progress made in thediagnosis and treatment of cancer. Together, we are making a world ofdifference in cancer care. For more information about cancer, pleasevisit Cancer.Net, ASCO’s patient information website.Sincerely,Sandra M. Swain, MD, FACPASCO PresidentTwo CommonlyUsed PaclitaxelChemotherapySchedules are EquallyEffective for Early-StageBreast Cancer, but OneHas Fewer Side EffectsWomen with higher-risk, earlystage breast cancer who receivedweekly chemotherapy withpaclitaxel (Taxol) after surgeryas part of a clinical trial lived forthe same amount of time withoutthe cancer returning as thosewho received higher doses ofthe same drug every two weeks(known as dose-dense therapy).However, the researchers foundthat the women who receivedchemotherapy every weekexperienced fewer and less serioustreatment-related side effects.Chemotherapy is the use ofdrugs to kill cancer cells, whichADVANCED CANCERNew Targeted ImmunotherapyIs Promising for SeveralAdvanced CancersContinued from page 1you are interested in participatingin a clinical trial, talk with yourdoctor for more information.Dr. Herbst was a recipient of aConquer Cancer Foundation ofASCO Young Investigator Award2 RESEARCH ROUND UPin 1997 and a Career DevelopmentAward in 1999. nWhat to Ask Your Doctor What type of cancer do Ihave and what is the stage?What does this mean? What are my treatmentoptions? What clinical trials are opento me?For More Information:Advanced Cancer Guides to Cancer(www.cancer.net/cancer) erapy)
work by stopping the cancer cells’ability to grow and divide. Drugslike paclitaxel are often givenafter surgery for breast cancerto kill any cancer cells that mayremain in the body. Paclitaxel isusually given to patients eitherweekly or every two weeks, ata higher dose. Although doctorscurrently use both treatmentschedules, this is the first timeresearchers have looked atwhether they have differentresults for patients.To answer this question,more than 2,700 women withnode-positive (cancer wasfound in the lymph nodes atdiagnosis) or high-risk nodenegative breast cancer that couldbe removed surgically firstreceived treatment with oneof three different schedules oftwo common chemotherapies,doxorubicin (Adriamycin) andcyclophosphamide (Neosar), andthen received either a standarddose of paclitaxel every weekfor 12 weeks (12 treatments) or ahigher dose every two weeks for12 weeks (six treatments).The researchers observedthat the cancer in 82% of thewomen who received weeklychemotherapy and 81% of womenwho received chemotherapyevery two weeks had notreturned within five years.However, the women whoreceived treatment every twoweeks experienced more allergicreactions and greater muscleand bone pain compared withthose who received treatmentevery week. Receiving treatmentevery two weeks also causedmore neurologic toxicity, acommon side effect involvingnumbness, tingling, and painin the fingers and toes. Thisside effect potentially could belessened or reduced by givingonly four treatments as is thecurrent practice rather than thesix treatments that were given aspart of this study.What this means for patients:“Our results suggest that eithertreatment plan will have a goodeffect, but the weekly scheduleseems to result in better qualityof life for patients, causing lessmuscle and bone pain and allergicreactions,” said lead study authorG. Thomas Budd, MD, a medicalFor Early-Stage Breast Cancer, Lymph NodeRadiation Therapy Works as Well as Surgery with aLower Risk of LymphedemaResults from a recent study showthat directing radiation therapyto the underarm lymph nodesworks as well as removing thelymph nodes with surgery and isless likely to cause lymphedemafor women with early-stagebreast cancer. Lymphedema isthe abnormal buildup of f luid(lymph) in the arm, causingswelling that can be painful andlimit a person’s movement. It isa common side effect from bothsurgery and radiation therapy tooncologist at the Cleveland Clinicin Ohio. “The findings provideassurance that women canchoose the lower-dose therapywithout sacrificing their chancesof survival.” After a diagnosisof cancer, patients and theirfamilies must make a number ofdecisions about cancer treatment,some of which are more difficultthan others. Take time to learnabout your treatment options andbe sure to ask questions aboutanything that is unclear. nWhat to Ask Your Doctor What type of chemotherapydo you recommend? Why? How often will I need to havetreatment? For how long? How will the treatmentbe given? How will chemotherapy affectmy daily life? Will I be able towork, exercise, and performmy usual activities? What are the potential sideeffects of this treatment? What can be done toprevent or manage theseside effects?the underarm lymph nodes.Because the first place breastcancer often spreads is the lymphnodes in the underarm, someof these lymph nodes are oftenremoved to look for signs ofcancer. This is called a sentinellymph node biopsy. If cancercells are found in the sentinellymph nodes, it is considered astandard part of care to removemore lymph nodes in a procedurecalled an axillary (underarm)Continued on page 4RESEARCH ROUND UP 3
BREAST CANCERFor Early-Stage BreastCancer, Lymph NodeRadiation Therapy Works asWell as SurgeryContinued from page 3lymph node dissection.In this study, 1,425 patients withsigns of cancer in the underarmlymph nodes (seen with a sentinellymph node biopsy) receivedeither an axillary lymph nodedissection or radiation therapyto the underarm lymph nodes.Researchers found that with bothtreatments, the risk of the diseasecoming back in the underarmlymph nodes was low—less than1% of those who had an axillarylymph node dissection had thedisease come back comparedwith about 1% of those who hadradiation therapy. In addition,both groups of patients wereequally likely to live for at leastfive years after treatment—aboutOne in Five AfricanAmerican Women withBreast Cancer Have aGenetically Higher Riskof Breast CancerIn a recent genetic study,researchers found that one in fiveAfrican American women withbreast cancer have an inherited(passed down in the family)mutation (change) in at least oneof the 18 genes that are linkedwith a higher risk of breast4 RESEARCH ROUND UP93% of patients in both groups.When researchers looked athow many patients developedlymphedema, they found adifference between the twogroups of patients. In the firstyear after treatment, 40% ofpatients who received an axillarylymph node dissection hadlymphedema, compared with 22%of those who received radiationtherapy. In addition, at five yearsafter treatment, 28% of those whoreceived an axillary lymph nodedissection still had lymphedema,compared with 14% of those whoreceived radiation therapy.What this means for patients:“I am sure these findings willlead many doctors to re-thinktheir strategy for treating patientswho have a positive sentinellymph node biopsy,” said leadauthor Emiel J. Rutgers, MD,a surgical oncologist at theNetherlands Cancer Institute.“Lymphedema is a seriouscancer. Compared to the generalpopulation, African Americanwomen are more likely to bediagnosed with breast cancer at ayounger age, die from the disease,and have triple-negative breastcancer. Triple-negative breastcancer is a fast-growing anddifficult-to-treat cancer that doesnot have hormone receptors (forthe hormones estrogen and/orprogesterone) or HER2 receptors(a protein found on some breasttumors). Researchers havesuspected that these differencesare due to inherited genes linkedto breast cancer, but this is thefirst study to look at all knownbreast cancer gene mutations, notconcern for patients and a sideeffect that can affect their qualityof life indefinitely.” Although it’snot possible to predict who willdevelop lymphedema, there aresteps you can take to help reduceyour risk, and the condition canoften be managed to help youfeel more comfortable. Talk withyour doctor for more informationabout preventing and managinglymphedema. nWhat to Ask Your Doctor What stage of breastcancer do I have? What doesthis mean? What are the results of mysentinel lymph node biopsy? What treatment plan do yourecommend? Why? Will I need an axillary lymphnode dissection? Radiationtherapy? What can I do to help avoidlymphedema or manage thecondition?just BRCA genes.For this study, researchersused genetic information from249 unrelated African Americanwomen with breast cancer to lookfor mutations in 18 genes using anew genetic test called BROCA.Overall, 56 out of 249 women(22%) had at least one mutationthat increases the risk of breastcancer. They also found thatthe mutations most commonlyoccurred on BRCA1, BRCA2,CHEK2, PALB2, ATM, andPTEN genes. In addition, theyfound that mutations were mostcommon for women with triplenegative breast cancer, with 30%of women with this type having a
breast cancer gene mutation. Also,27% of women diagnosed beforeage 45, 49% of women with asecond breast cancer, and 30% ofwomen with a family history ofeither breast or ovarian cancer hadmutations in at least one breastcancer gene.Researchers also found thatmost of the mutations were uniqueto each person, meaning that itvaried between each family. Othergroups of people with a higherinherited risk of brea
RESEARCH ROUND UP 3 work by stopping the cancer cells’ ability to grow and divide. Drugs like paclitaxel are often given after surgery for breast cancer to kill any cancer cells that may remain in the body. Paclitaxel is usually given to patients either weekly or every two weeks, at a higher dose. Although doctors currently use both treatment schedules, this is the first time researchers .