Transcription
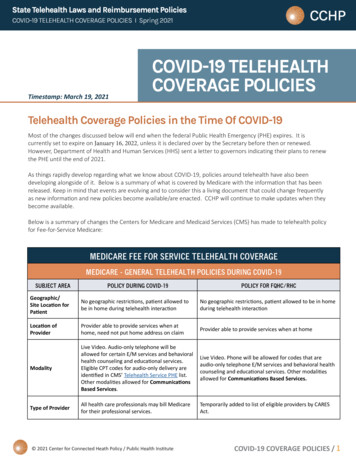
TELEHEALTH COVERAGE POLICIES IN THE TIME OF COVID-19 TO DATETimestamp: April 30, 2020 – 3 pm PTAs things rapidly develop regarding what we know about COVID-19, policies around telehealth have alsobeen developing alongside of it. Below is a summary of what is covered by various public and privatepayers with the information that has been released. Keep in mind that events are evolving and toconsider this a living document that could change frequently as new information and new policiesbecome available/are enacted. CCHP will continue to make updates when they become available.Below is a summary of changes the Centers for Medicare and Medicaid Services (CMS) has made totelehealth policy for Fee-for-Service Medicare:MEDICARE – GENERAL TELEHEALTH POLICIES DURING COVID-19SUBJECT AREAPOLICY DURING COVID-19POLICY FOR FQHC/RHCGeographic/Site No geographic restrictions, patientNo geographic restrictions, patientlocation forallowed to be in home duringallowed to be in home during telehealthpatienttelehealth interactioninteractionLocation ofProvider able to provide services when Provider able to provide services when atproviderat home, need not put home addresshomeon claimModalityLive Video. Phone will be allowed forLive Video. Phone will be allowed forcodes audio-only telephone E/Mcodes that are audio-only telephone E/Mservices and behavioral healthservices and behavioral health counselingcounseling and educational services.and educational services. Other modalitiesOther modalities allowed forallowed for under Communications BasedCommunications Based ServicesServices.Type ofAll health care professionals to billTemporarily added to list of eligibleproviderMedicare for their professionalproviders by CARES Actservices.ServicesApproximately 180 different codesCan only provide the services on THIS listavailable for reimbursement if provided via telehealth and be reimbursed byvia telehealth. List available HERE.Medicare.Amount ofSame as would received if it had been 92.03reimbursement provided in-person (Fee-for-servicerate). Some rates for telephone visitshave been increased.ModifiersPer the final interim rule, providers are For services delivered January 27, 2020 –allowed to report POS code that would June 30, 2020have been reported had the serviceRHCs: Use G2025 with CG modifier. 95been furnished in person so thatmodifier can be appended, but is notproviders can receive the appropriaterequired.facility or non-facility rate and use theFQHCs: Must report 3 HCPCS/CPT codes:modifier “95” to indicate the service(1) the PPS specific payment code; (2) thetook place through telehealth. IfHCPCS/CPT code that describes the serviceproviders wish to continue to use POSwith the 95 modifier; (3) G2025 withcode 02, they may and it pays themodifier 95facility rate.Beginning July 1, 2020 CENTER FOR CONNECTED HEALTH POLICY/PUBLIC HEALTH INSTITUTE4/30/20, 3 pm PT, Page 1
FQHCs/RHCs: Only submit G2025. RHCsshould no longer use CG modifier.MEDICARE- OTHER POLICIES RELATED TO TELEHEALTH DURING COVID-19SUBJECT AREAPOLICY DURING COVID-19End Stage Renal Disease &CMS exercising enforcement discretion on requirement that homeHome Dialysis Patientsdialysis patients receiving services via telehealth must have amonthly face-to-face, non-telehealth encounter in the first initialthree months of home dialysis and after the first initial three months,at least once every three consecutive months. ESRD clinicians nolonger must have one “hands on” visit/month for current requiredexamination of vascular access site. Clinicians will not have to meetthe National Coverage Determination or Local CoverageDetermination of face-to-face visit for evaluations and assessmentsduring this public health emergency.Nursing HomesCMS waiving requirement that physicians and non-physicianpractitioners perform in-person visit for nursing home residents andif appropriate, allow them to be done via telehealth.HospiceDuring an emergency period, the Secretary may allow telehealth tomeet the requirement that a hospice physician or nurse practitionermust conduct a face-to-face encounter to determine continuedeligibility for hospice care.Frequency LimitationsThe pre-COVID-19 frequency limitations on subsequent in-patientvisit (once every three days), subsequent SNF visit (once every 30days), and critical care consult (once a day) were removed.SupervisionPhysician supervision may be provided using live video. For othersupervision changes, see CMS Provider and Practitioner Guidance.Stark LawsCMS allowing certain waivers: hospitals and other health careproviders can pay above or below fair market value to rentequipment or receive services from physicians; health care providerscan support each other financially to ensure continuity of health careoperations; and others. See CMS Physician and PractitionerGuidance.Provider Home Address onProvider need not put their home address on the claim if theyClaimconducted a telehealth visit while at home.Out-of-pocket costs/co-paysStill applies, but the OIG is providing health care providers flexibilityto reduce or waive fees. COVID-19 testing should be waived.Prior existing relationshipCan be to new and established patientsHospitals & Originating Site Fee Hospitals can bill an originating site fee when the patient is at home.Guidance.Hospital-Only RemoteHospitals may provide through telecommunication technologyOutpatient Therapy &behavioral health and education services furnished by hospitalEducation Servicesemployed counselors or other health professionals who cannot billMedicare directly. Includes partial hospitalization services and can befurnished when the beneficiary is the home. Guidance.Resources: CENTER FOR CONNECTED HEALTH POLICY/PUBLIC HEALTH INSTITUTE4/30/20, 3 pm PT, Page 2
HR 6074HR 748CMS Fact SheetCMS FAQCMS Physician and Practitioner GuidanceCOVID-19 Emergency Declaration Blanket Waivers for Health Care ProvidersInterim Final Rule – Other changes were made in the Interim Final Rule that are not reflected inthe overview charts on this page. See CCHP’s crosswalk between the Interim Final Rule and theCMS Guidance document.HRSA/HHS Telehealth Resource Website for both Patients and ProvidersOther Medicare & Medicaid PoliciesEXISTING TELEHEALTH POLICYPOLICY CHANGE IN RESPONSEWHAT CAN BE COVEREDPRE-COVID-19TO COVID-19MEDICARELicensingTemporarily waive Medicare and Medicaid requirements to be licensed in the patient state if they areenrolled in Medicare, have valid license in the state which relates to Medicare enrollment, infurnishing services in the state where there emergency is occurring, and not excluded from practicingin that state or any other state that is part of the emergency. State requirements will still apply.Medicare AdvantageMedicare Advantage (MA) plans Medicare AdvantageMA plans have some flexibilityhave the flexibility to have more Organizations were informed by to expand their coverage ofexpansive telehealth policiesCMS that if they wish to expand telehealth beyond what theyrelated to types of servicescoverage of telehealth servicescurrently do. What is coveredcovered, where those servicesbeyond what has already beenwill depend on what each plancan take place (no geographicapproved by CMS, they willdecides to do. NOTE: MA plansor site limitations), modalityexercise its enforcementdo NOT have to provide theseused. Still limits the types ofdiscretion until it is determined more expansive telehealthproviders reimbursed.that it is no longer necessary inservices. They are only requiredconjunction with the COVID-19to provide what is covered byoutbreak. (CMS Memo)Fee-for-Service.Other Technology-Enabled ServicesVirtual Check-In CodesOther providers such as PTs,Virtual check-in codes do notG2010, G2012*OTs and speech languagehave geographic or sitepathologists may bill theserestrictions attached so theyCan be done synchronously and codes as well as G2061-G2063.can be used to engage withasynchronously and telephonepatients, but thecan be usedreimbursement amount forthese codes is low and are onlymeant to act as quick check-inswith patients that do not lastmore than a few minutes. CENTER FOR CONNECTED HEALTH POLICY/PUBLIC HEALTH INSTITUTE4/30/20, 3 pm PT, Page 3
ns (eConsult) *99446, 99447, 99448, 99449,99451, 99452Remote monitoring services: *Chronic Care ManagementComplex Chronic CareManagementTransitional Care ManagementRemote Physiologic MonitoringPrinciple Care ManagementNo Change MadeOnline Digital Evaluation (E*Visit) – G2061-2063Online medical Evaluations –99421-99423Telephone E/M ServicesMEDICAIDEXISTING TELEHEALTH POLICYPRE-COVID-19Telehealth reimbursementpolicies vary from state to state.If the State Medicaid programhas managed care, telehealthreimbursement can vary fromplan-to-plan. For Medicaid feefor-service policies, checkCCHP’s website.No Changes MadeNo Change MadeAdded by Interim Final RulePOLICY CHANGE IN RESPONSETO COVID-19A Medicaid FAQ was issuedstating that state Medicaidprograms have broad authorityto utilize telehealth within theirMedicaid programs includingusing telehealth or telephonicconsultations in place of typicalface-to-face requirements whencertain conditions are met.States would have to use theAppendix K process for this.eConsult allows a provider-toprovider consultation. Paysboth providers, but checkdefinition for the time neededfor each code.These services are notconsidered “telehealth” servicesand were never subject totelehealth limitations. They dohave other factors that limithow they can be used so makesure you check the definitionfor the codes.These services are notconsidered “telehealth” servicesand were never subject totelehealth limitations.98966-98968; 99441-99443WHAT WILL BE COVERED ATTHIS TIMEStill developing. Some stateshave encouraged providers andhealth plans to utilize telehealthmore broadly to provideservices but for many states thepolicies continue to bedeveloping as they navigate thissituation.As noted above, licensurerequirements were waived forMedicaid, though staterequirements would still apply.Other Federal ActionsDEAThe declaration of the national emergency enacted one of the exceptions to the Ryan Haight Act fortelehealth (telemedicine as it is referred to in the Act). CENTER FOR CONNECTED HEALTH POLICY/PUBLIC HEALTH INSTITUTE4/30/20, 3 pm PT, Page 4
For as long as the Secretary’s designation of a public health emergency remains in effect, DEA-registeredpractitioners may issue prescriptions for controlled substances to patients for whom they have notconducted an in-person medical evaluation, provided all of the following conditions are met: The prescription is issued for a legitimate medical purpose by a practitioner acting in the usualcourse of his/her professional practice The telemedicine communication is conducted using an audio-visual, real-time, two-wayinteractive communication system. The practitioner is acting in accordance with applicable Federal and State .htmlHIPAAA change was made regarding the Health Insurance Portability and Accountability Act (HIPAA) “Effectiveimmediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waivepenalties for HIPAA violations against health care providers that serve patients in good faith througheveryday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwidepublic health emergency.“ l-topics/emergencypreparedness/index.htmlOCR Guidance - ement-discretion-telehealth/index.htmlIt should be noted that many states do have laws and regulations regarding health information and whatis required to protect and secure it. This will likely not impact those state laws and regulations. Aseparate state action will be necessary.PRIVATE INSURERSEXISTING TELEHEALTH POLICYPRE-COVID-19Coverage varied from payer-topayer, depending on the plan.POLICY CHANGE IN RESPONSETO COVID-19Several health plans haveannounced that they will maketelehealth more widelyavailable or offering telehealthservices for free for a certainperiod of time. Some of theannouncements have comefrom Aetna, Cigna andBlueShield BlueCross.Additionally, Vice PresidentPence had announced that hehad secured a commitmentfrom the health plans to covertelehealth services, but nodetails or which plans hadagreed were given. CENTER FOR CONNECTED HEALTH POLICY/PUBLIC HEALTH INSTITUTEWHAT WILL BE COVERED ATTHIS TIMEStill developing. Few detailshave been given and wouldrequire individuals to inquirewith their insurer what isexactly covered. Montanahealth plans recently agreed tocover telehealth deliveredservices. Check CCHP’s Statesite for information. Somelinks to the announcements:AetnaCignaBlueShield BlueCross4/30/20, 3 pm PT, Page 5
* See CCHP’s Introductory Billing Guide to Medicare Fee-for-Service.State ActionsFor State Actions, go to CCHP’s webpage for the latest -19-related-state-actions CENTER FOR CONNECTED HEALTH POLICY/PUBLIC HEALTH INSTITUTE4/30/20, 3 pm PT, Page 6
the overview charts on this page. See CCHP's crosswalk between the Interim Final Rule and the CMS Guidance document. HRSA/HHS Telehealth Resource Website for both Patients and Providers Other Medicare & Medicaid Policies EXISTING TELEHEALTH POLICY PRE-COVID-19 POLICY CHANGE IN RESPONSE TO COVID-19 WHAT CAN BE COVERED MEDICARE Licensing