Transcription
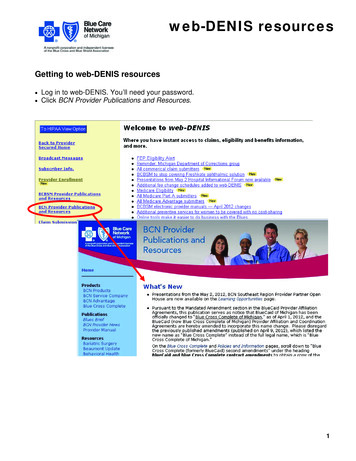
web-DENIS resourcesGetting to web-DENIS resources Log in to web-DENIS. You’ll need your password. Click BCN Provider Publications and Resources.1
web-DENIS resourcesweb-DENIS Behavioral Health page2
web-DENIS resourcesweb-DENIS Billing page3
Blue CrossBlueShieldof MichiganSTATUS CLAIM REVIEW FORMLAST NAME OF INSURED/SUBSCRIBERGROUP NO.FIRST NAMEPHYSICIAN OR PROVIDER NAME, ADDRESS, ZIP CODESERVICE CODEINSURED'S/SUBSCRIBER IDENTIFYING NO. (INCLUDE ANY LETTERS)PROVIDER CODE/NPIA.B.BC/BSF.E.P.COMP.O/STELEPHONE NUMBERNPIP.O.T.A.REJ.CORR.ORIGINAL FORM WAS PAY PROVIDERCOMP NPRYES1. PATIENT'S LAST NAME2. MID.3. FIRST NAME4. PAT'S BIRTH5. PAT'S SEXM7. PATIENT'S MEDICARE HIB NO.8. PATIENT'S ACCT. NO.6. PAT'S RELATIONSHIP TO INSUREDSELFF9. INSURED'S TELE. NO.19. DATE OF15. CITYILLNESS (FIRST SYP.) 20. ADMISSION DATE 21.DISCHARGE DATEINJURY (ACCIDENT)PREGNANCY (L.M.P.)24. PPO REFERRING PHYSICIAN CODE/NPIA.B.25. PAY'T. AMT. REC'DSPOUSE10. WAS CONDITION REL TOEMP14. INSURED'S STREET ADDRESS16. ST.NOAUTODEPENDENT11. CR IND 12. ATTACH 13. MULT.OTH17. ZIP CODE18. PRIOR AUTHORIZATION NO.22. SERVICE FACILITY CODE/NPIA.23. REFERRING/ORDERING LICENSE # /NPIA.B.B.NPI26. CHECK DATE27. CHECK NO.NPI28. NON-PAYM'T CODE29. DOCUMENT NO.NPI30. DIAGNOSIS OR ADDITIONAL INFORMATION AREA31. DATE OF SRV1 40. M-1M-2M-331. DATE OF SRV2 40. M-1M-2M-331. DATE OF SRV3 40. M-1M-2M-331. DATE OF SRV4 40. M-1M-2M-332. DX CODEM-432. DX CODEM-432. DX CODEM-432. DX CODEM-433. PLACE41. MED.REASONABLE33. PLACE41. MED.REASONABLE33. PLACE41. MED.REASONABLE33. PLACE41. MED.REASONABLE34. PROC. CODE42. MED DEDUCT.34. PROC. CODE42. MED DEDUCT.34. PROC. CODE42. MED DEDUCT.34. PROC. CODE42. MED DEDUCT.35. QTY.36. DURATION43. OTR CARRIER AMOUNT35. QTY.44. QUAL. RENDERING LICENSE #A.B.5 40. M-1M-2M-331. DATE OF SRV6 40. M-1M-2M-332. DX CODEM-432. DX CODEM-433. PLACE41. MED.REASONABLE33. PLACE41. MED.REASONABLE34. PROC. CODE36. DURATION43. OTR CARRIER AMOUNT42. MED DEDUCT.34. PROC. CODE42. MED DEDUCT.35. QTY.37. CHARGES44. QUAL.RENDERING LICENSE #B.36. DURATION43. OTR CARRIER AMOUNT35. QTY.37. CHARGES44. QUAL. RENDERING LICENSE #A.B.A.31. DATE OF SRV37. CHARGES36. DURATION43. OTR CARRIER AMOUNT35. QTY.44. QUAL. RENDERING LICENSE #A.B.36. DURATION43. OTR CARRIER AMOUNT35. QTY.37. CHARGES43. OTR CARRIER AMOUNT44. QUAL. RENDERING LICENSE #A.B.37. CHARGES44. QUAL.A.39. I.C.45. RENDERING NPINPI38. MISC. DATE39. I.C.45. RENDERING NPINPI38. MISC. DATE39. I.C.45. RENDERING NPINPI38. MISC. DATE39. I.C.45. RENDERING NPINPI37. CHARGES36. DURATION38. MISC. DATERENDERING LICENSE #B.38. MISC. DATE39. I.C.45. RENDERING NPINPI38. MISC. DATE39. I.C.45. RENDERING NPINPIDO NOT WRITE IN THIS AREA - DOCUMENT NUMBERPROVIDER SIGNATURECF 1362 JAN 07Blue Cross Blue Shield of Michigan is a nonprofit corporation and independent licensee of the Blue Cross and Blue Shield AssociationDATE
Blue Care NetworkFilling Out the Paper Status Claim Review Form for BCN ClaimsFor BCN claims, providers completing the Status Claim Review Form must re-bill the entire claim for anyservices performed on a particular date of service and include any corrections. The chart below provides stepby-step instructions for professional billers completing the paper Status Claim Review Form for BCN claims.Note: For Blue Cross Blue Shield of Michigan claims, providers should follow the instructions on page 2 of theBCBSM Status Review Claim Form.How to complete the paper Status Review Claim FormField #Upper leftcornerUpper rightcornerField NameInformationSUBSCRIBER INFORMATIONSubscriber NameEnter subscriber’s last name and first name.Group NumberNot requiredService CodeNot requiredInsured SubscriberIdentifying No.Enter the subscriber’s alphanumeric ID number.Type of Coverage BC/BS: — Leave blank. F.E.P. — Leave blank. COMP. — Leave blank. O/S — Leave blank.PROVIDER INFORMATIONProvider Name andAddressEnter the provider’s name and address.Provider Code/NPIEnter the NPI.Note: Effective Sept. 30, 2009, only the NPI is accepted as the provideridentifier.Provider’s PhoneEnter area code and phone number.continued on next page1Revised January 2011
Blue Care NetworkFilling Out the Paper Status Claim Review Form for BCN ClaimsHow to complete the paper Status Review Claim FormField #Field NameInformation P.O.T.A. — A payment was received other than what was anticipated. REJ. — A rejection is being questioned. CORR. — A correction to the original claim is being submitted. COMP NPR — Leave blank. Original Form Was Pay Provider — Enter an X in the appropriate on ForSubmission1Patient’s Last NameEnter patient’s last name.2MidIf known, enter patient’s middle initial.3First NameEnter the patient’s complete first name. Do not use a nickname unless thepatient is listed that way on the contract.4Patient’s BirthEnter the patient’s birth date in a six-digit format with no spaces (MMDDYY).5Patient’s SexEnter an X in the appropriate box.6Pat’s. Relationship toInsuredEnter an X in the appropriate box.7Patient’s Medicare HIBNo.Leave blank.8Patient’s Account No.Not required. If an office has assigned a case number to the patient, enter ithere. A maximum of 20 characters may be used. BCN will include this numberon the payment voucher to assist providers in the patient’s accounting.9Insured’s Tele No.Enter the subscriber’s area code and phone number.10Was condition Rel. to EMP — Enter an X if the accident took place in the patient’s place ofemployment. AUTO — Enter X if the patient’s condition is related to an auto accident. OTH — Enter X if the accident is not related to employment or auto accident.11CR IndLeave blank.12AttachEnter the number of pages attached to the claim form. This includesexplanatory letters or copies of other carrier’s payment vouchers. If thenumber of attachments is not indicated, the claim may not be processedcorrectly.13Mult.Enter an X in this box if there are multiple diagnoses or to indicate thatadditional information is entered in field 30. This field applies only for claimswith multiple diagnoses or additional information.14Insured’s StreetAddressEnter the subscriber’s address.15CityEnter the subscriber’s city.16STEnter the subscriber’s two-letter state abbreviation as used by the U.S. PostalService.17Zip CodeEnter the subscriber’s ZIP code.18Prior Authorization No.If billing a service that was authorized by BCN, enter the authorization numberreceived. The number of digits may vary.Enter an X in all boxesthat apply.continued on next page2Revised January 2011
Blue Care NetworkFilling Out the Paper Status Claim Review Form for BCN ClaimsHow to complete the paper Status Review Claim FormField #Field NameInformation19Date of Enter the date the patient first experienced symptoms of the illness orcondition for which services were performed, with the following exceptions:o If the service is related to end stage renal disease, enter the date of thefirst maintenance dialysis or the date of the kidney transplant.o If the service is related to an injury — whether it is the initial treatment ora follow-up service — enter the date of the injury.o If the service is related to pregnancy, enter the date of the lastmenstrual period. If unable to determine the LMP, use the estimateddate of conception. Enter the date in a six-digit format: for example, enter Jan. 1, 2007, as010107.20Admission DateIf the service was performed on an inpatient basis, enter the admission date.Otherwise, leave the field blank. For inpatient services only21Discharge DateIf the service was performed on an inpatient basis, enter the discharge date.(Only the discharge doctor is responsible for this information.) Otherwise,leave the field blank.Use this field only for inpatient services performed by the physician whodischarged the patient.22Facility CodeNot required23Referring/Ordering PhysicianInformationNot required24PPO ReferringPhysician Code/NPILeave blank25Payment Amt. Rec’d.Enter the total payment received for the services in question.26Check DateEnter the date of the Remittance Advice for the service in question.27Check No.Enter the check number from the Remittance Advice.28Nonpayment CodeEnter the nonpayment code from the Remittance Advice for the service inquestion.29Document No.Enter the BCN claim number from the Remittance Advice for the service inquestion.30Diagnosis orAdditional InformationArea Diagnosis — Enter diagnosis codes. Additional Information — Provide an explanation of why BCN shouldreconsider action on this claim. Enter additional information or anyinformation that was omitted on the original claim. Describe any attachments.Attach a second sheet of paper if needed. If original claim was denied for noauthorization on file and a copy of the authorization has been retained fromthe primary care physician, attach it to the Status Claim Review Form.continued on next page3Revised January 2011
Blue Care NetworkFilling Out the Paper Status Claim Review Form for BCN ClaimsHow to complete the paper Status Review Claim FormField #Field NameInformationService informationIn fields 31 through 45, enter service information. If entering information that was omitted or reported incorrectly on theoriginal claim, enter an X in the small shaded box to the right of that item.31Date of Srvc.Enter the date each service was provided. Enter the date in a six-digit format(MMDDYY).32Dx CodeEnter the full five-digit, four-digit or three-digit ICD-9-CM code that representsthe primary diagnosis.33PlaceEnter the appropriate HIPAA-compliant location of service code to describewhere care was provided. Refer to the CMS-1500 (08/05) claim informationearlier in the Professional Claim Examples chapter of the BCN ProviderManual.34Proc. CodeEnter the five-character procedure code for the procedure performed.35Qty.Enter the number of treatments, visits or anesthesia minutes.36DurationLeave blank.37ChargesEnter the original charge billed for the service. If billing multiple services asone line item, enter the total amount for all services on the same service line.Do not include dollar signs, decimals, negative signs or any other nonnumericcharacters. Also, do not indicate if the patient has already paid all or someportion of the charges; payments from the patient should not be shownanywhere on the form.38Misc. Date If reporting multiple services on one line, enter the last date of service in thisfield. If the service date is related to pregnancy, enter the first date of prenatalcare. In all other cases, leave this field blank.39I.C.Enter modifier 22 if reporting unusual circumstances and have used anunlisted procedure code*.Use for unusual circumstances and unlisted procedure codes only.40ModifiersEnter up to four two-character modifiers to further define the procedure codeentered in Field 34. Report up to four modifiers for each procedure code.41Med. ReasonableLeave blank.42Med. Deduct.If requesting additional BCN 65 payment, enter the total amount applied to theMedicare deductible as shown on the Medicare payment voucher. Use onlyfor BCN 65 inquiries when an amount was applied to the patient’sdeductible.43Other Carrier AmountNot required.44Qual.RenderingLicense #A. Not required.B. Enter the rendering physician’s BCBSM license number, for example,AS123456. This is crucial when billing with a Group Bill PIN.45Rendering NPIEnter the rendering provider’s NPI.Lower rightcornerProvider SignatureEnter the provider’s authorized signature or stamped reproduction and date. Ifcompleting claims form on computer, “signature on file” is acceptable.4Revised January 2011
Blue CrossBlueShieldof MichiganSTATUS CLAIM REVIEW FORMLAST NAME OF INSURED/SUBSCRIBERSUBSCRIBERGROUP NO.FIRST NAMEPHYSICIAN OR PROVIDER NAME, ADDRESS, ZIP CODESAMPLESAMPLE PROVIDERADDRESSCITY, STATE, ZIP CODESERVICE CODEXXXXXXINSURED'S/SUBSCRIBER IDENTIFYING NO. (INCLUDE ANY LETTERS)PROVIDER LEPHONE L FORM WAS PAY PROVIDERCOMP NPRYES1. PATIENT'S LAST NAME2. MID.3. FIRST NAMEPATIENT4. PAT'S BIRTHSAMPLE7. PATIENT'S MEDICARE HIB NO.8. PATIENT'S ACCT. NO.SELF25. PAY'T. AMT. REC'D80 00SPOUSEEMPAUTO17. ZIP CODESTXXXXXDEPENDENT11. CR IND 12. ATTACH 13. MULT.10. WAS CONDITION REL TO16. ST.CITYILLNESS (FIRST SYP.) 20. ADMISSION DATE 21.DISCHARGE DATEINJURY (ACCIDENT)PREGNANCY (L.M.P.)24. PPO REFERRING PHYSICIAN CODE/NPIA.6. PAT'S RELATIONSHIP TO INSUREDFXXXXXXXXXX15. CITYADDRESSB.M9. INSURED'S TELE. NO.XXXXX14. INSURED'S STREET ADDRESS19. DATE OF5. PAT'S SEX050110NOOTH18. PRIOR AUTHORIZATION NO.22. SERVICE FACILITY CODE/NPIA.23. REFERRING/ORDERING LICENSE # /NPIA.B.B.NPI26. CHECK DATE07291127. CHECK NO.NPI28. NON-PAYM'T CODEXXXXXX29. DOCUMENT NO.EXXXXXXXXXXXNPI30. DIAGNOSIS OR ADDITIONAL INFORMATION AREACORRECTING PROCEDURE CODE 90471 FROM ORIGINAL CLAIM. REPLACING IT WITH PROCEDURECODE 90472.31. DATE OF SRV0720111 40. M-1 M-232. DX CODEV068M-3M-433. PLACE1141. MED.REASONABLE34. PROC. CODE9047242. MED DEDUCT.35. QTY.36. DURATION30720112 40. M-1 M-232. DX CODEV0489M-3M-431. DATE OF SRV32. DX CODE072011V0683 40. M-1M-2M-331. DATE OF SRV0720114 40. M-1 M-2LTM-2M-2M-41141. MED.REASONABLE33. PLACE1141. MED.REASONABLE33. PLACE1141. MED.REASONABLE34. PROC. CODE9047342. MED DEDUCT.34. PROC. CODE9069842. MED DEDUCT.34. PROC. CODE6921042. MED DEDUCT.35. QTY.44. QUAL. RENDERING LICENSE #A.B.36. DURATIONM-3M-332. DX CODEM-432. DX CODEM-433. PLACE41. MED.REASONABLE33. PLACE41. MED.REASONABLE34. PROC. CODE42. MED DEDUCT.34. PROC. CODE42. MED DEDUCT.37. CHARGES135. QTY.44. QUAL. RENDERING LICENSE #A.B.36. DURATION37. CHARGES144. QUAL. RENDERING LICENSE #A.B.36. DURATION37. CHARGES144. QUAL.RENDERING LICENSE #B.36. DURATION43. OTR CARRIER AMOUNT35. QTY.NPI XXXXXXXXXX38. MISC. DATE45. RENDERING NPINPI XXXXXXXXXX38. MISC. DATE39. I.C.45. RENDERING NPINPI XXXXXXXXXX38. MISC. DATE39. I.C.36. DURATION43. OTR CARRIER AMOUNT37. CHARGES44. QUAL.45. RENDERING NPINPI XXXXXXXXXX37. CHARGES44. QUAL. RENDERING LICENSE #A.B.A.RENDERING LICENSE #B.38. MISC. DATE39. I.C.45. RENDERING NPINPI38. MISC. DATE39. I.C.45. RENDERING NPINPIDO NOT WRITE IN THIS AREA - DOCUMENT NUMBERCF 1362 JAN 0739. I.C.45 0043. OTR CARRIER AMOUNT35. QTY.45. RENDERING NPI25 0043. OTR CARRIER AMOUNT35. QTY.39. I.C.25 0043. OTR CARRIER AMOUNTA.31. DATE OF SRV6 40. M-132. DX CODE3829M-331. DATE OF SRV5 40. M-1M-433. PLACE38. MISC. DATE25 0043. OTR CARRIER AMOUNTLT31. DATE OF SRV37. CHARGESPROVIDER SIGNATURE080311PROVIDER SIGNATUREDATEBlue Cross Blue Shield of Michigan is a nonprofit corporation and independent licensee of the Blue Cross and Blue Shield Association
Resubmitting a claim for inquiryFacilityproviders canfile a paperinquiry usinga UB-04 with aTOB 7Facility providers can submit a paper status inquiry claim using a UB-04 claimform with a TOB 7.When completing the UB-04 with a TOB 7, the provider must rebill allservices that were performed on a particular date of service and include anycorrections. The claim should be submitted by completing the following steps:1. Print and complete the UB-04 claim form available at web-DENIS BCNProvider Publications and Resources Billing UB-04 form.Note: Providers should complete the form according to instructionsavailable in the National UB-04 Manual.This includes the following:--Enter the appropriate type of bill code ending in 7.--Enter the claim number from the original or previous RemittanceAdvice for the service in question.2. Attach any relevant documentation.3. Mail the request to the appropriate address:Blue Care NetworkP.O. Box 68710Grand Rapids MI 49516-8710BCN Advantage- OR Blue Cross CompleteP.O. Box 68753Grand Rapids MI 49516-8753For additional information on how to file a status inquiry claim, facilityproviders should review the claim example Status inquiry claim: outpatient,TOB 7, which is available at web-DENIS BCN Provider Publications andResources Billing Status inquiry claim: outpatient, TOB 7.14-46Claims2012
Resubmitting a claim for inquiryProfessionalproviders canfile a paperinquiry usingthe Status ClaimReview FormProfessional providers can submit a paper status inquiry using the StatusClaim Review Form.When completing the Status Claim Review Form, providers must rebill allservices that were performed on a particular date of service and include anycorrections. The claim should be submitted by completing the following steps:1. Print and complete the front page of the Status Claim Review Form,which is available at web-DENIS BCN Provider Publications andResources Billing Status Claim Review Form.Note: Providers should complete the form according to the instructionsavailable at web-DENIS BCN Provider Publications and Resources Billing Status Claim Review Form instructions (paper) for BCNclaims.This includes entering the claim number from the original or previousRemittance Advice for the service in question.2. Attach any relevant documentation.3. Mail the request to the appropriate address:Blue Care NetworkP.O. Box 68710Grand Rapids MI 49516-8710BCN Advantage- OR Blue Cross CompleteP.O. Box 68753Grand Rapids MI 49516-8753For additional information on how to complete the form, professionalproviders should review the Status Claim Review Form example available atweb-DENIS BCN Provider Publications and Resources Billing StatusClaim Review Form example.Professionalproviders only:obtaining thepaper form14-47A copy of the front page of the Status Claim Review Form (without theBCBSM back-page instructions) is available at web-DENIS BCN ProviderPublications and Resources Billing Status Claim Review Form.Note: To order large quantities of the Status Claim Review Form, providersshould complete and fax or mail the BCBSM Professional and FacilitySupply Requisition Form. This can be found at MiBCN.com I am aprovider Provider Supply Forms BCN Providers Use the Facility andProfessional Provider Supply Requisition Form.Claims2012
UB-04 claim examples – outpatientStatus inquiry claim: outpatient, TOB 7This claim example illustrates a status inquiry claim sent by a facility provider to request that BCN reconsider a denial on the originalclaim.When completing the UB-04 with a TOB 7, providers must rebill all services that were performed on a specific date of service andcommunicate any corrections.For additional information, providers should refer to the “Resubmitting a claim for inquiry” section of the Claims chapter of the Blue CareNetwork Provider Manual.Form locatorDescriptionWhat to enter4TYPE OF BILLEnter the appropriate outpatient type of bill code ending in 7, to indicate replacement of a prior claim.54PRIOR PAYMENTSEnter the payment amount the provider has received toward payment of this bill prior to this billing date bythe payer indicated.64DOCUMENTCONTROL NUMBEREnter the 12-digit BCN claim number located on the original or previous Remittance Advice for the servicein question.80REMARKSIndicate the reason for resubmission.Note: If any of the information presented here conflicts with the BCN provider contract, the contract language should be followed.*CPT codes, descriptions and two-digit numeric modifiers only are copyright 2011 American Medical Association. All rights reserved.Guidelines for reviewing the claim examples: The entire claim must be completed before it is sent to BCN for processing. It is not possible to show examples ofall types of claims, so providers may need to reference multiple examples to obtain the information needed to properly complete a claim.Where appropriate, providers should substitute their own billing information. For example, a claim submitted for a different type of facility or classification will have adifferent type of bill (form locator 4) than that shown in the example. In all cases, providers should refer to the National UB-04 Manual for a detailed description ofeach form locator.continued on next pageJanuary 2012
In Box 4(Type of Bill),enter "7."143a PAT.CNTL #b. MED.REC. #265 FED. TAX NO.8 PATIENT NAME9 PATIENT ADDRESSa10 BIRTHDATE11 SEX31OCCURRENCECODEDATE12DATEacADMISSION13 HR 14 TYPE 15 SRC 16 DHR 17 OF BILL7STATEMENT COVERS ON CODES2422232135CODE25262736CODEOCCURRENCE SPANFROMTHROUGHd28e29 ACDT 30STATE37OCCURRENCE SPANFROMTHROUGHaabb3839CODE40CODEVALUE CODESAMOUNT41CODEVALUE CODESAMOUNTVALUE CODESAMOUNTabcd42 REV. CD.44 HCPCS / RATE / HIPPS CODE43 DESCRIPTION45 SERV. DATE46 SERV. UNITS47 TOTAL CHARGES48 NON-COVERED N DATE50 PAYER NAME52 REL.INFO51 HEALTH PLAN ID53 ASG.BEN.2355 EST. AMOUNT DUE54 PRIOR PAYMENTS56 NPIA57ABOTHERBPRV IDCC58 INSURED’S NAME59 P. REL 60 INSURED’S UNIQUE IDIn Box 64,enter originalclaim number.ABC63 TREATMENT AUTHORIZATION CODES62 INSURANCE GROUP NO.61 GROUP NAMEABC65 EMPLOYER NAME64 DOCUMENT CONTROL NUMBERAABBCC66DX67IAJ69 ADMIT70 PATIENTDXREASON DXPRINCIPAL PROCEDUREa.74CODEDATEBKabCLOTHER PROCEDURECODEDATEb.OTHER PROCEDUREDATECODEe.cDM71 PPSCODEOTHER PROCEDURECODEDATEEN7572ECIFOa76 ATTENDINGGPbNPILASTc.OTHER PROCEDURECODEDATEd.OTHER PROCEDURECODEDATE77 OPERATING81CCaUB-04 CMS-1450APPROVED OMB NO. 0938-099778 OTHERbLASTc79 OTHERdLASTNUBC National UniformBilling Committee73QUALFIRSTNPILAST80 REMARKSHQc68QUALFIRSTNPIQUALFIRSTNPIQUALFIRSTTHE CERTIFICATIONS ON THE REVERSE APPLY TO THIS BILL AND ARE MADE A PART HEREOF.
Getting to web-DENIS resources . BCBSM Status Review Claim Form. How to complete the paper Status Review Claim Form Field # Field Name Information Revised January 2011 SUBSCRIBER INFORMATION Subscriber Name Enter subscriber's last name and first name. Upper left corner .