Transcription
Behavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesBCN Provider Resource GuideWelcome to the BCN Provider Resource Guide!In this guide you will find contact information for many of the services that BCN offersand for the functions you most frequently perform in caring for BCN members.Use the navigation bar at the left to go directly to the information for specific topics.Use the Next and Previous buttons at the lower right to navigate forward or backwardin the document.The pages in this guide are updated on an as-neededbasis. The date shown in the lower left corner of the textreflects the date on which the information on that pagewas last revised. If you print any pages from theguide, be sure to check back for updates.You can search the guide for a specific topicby inserting one or more keywords into theFind field immediately above the guide andpressing Enter.If there is other information youfeel should be added to theguide, be sure to let usknow by contacting us atBCNProvComm@bcbsm.com.Utilization Managementbcbsm.com ereferrals.bcbsm.comPreviousNext
Behavioral Health (Mental Health / Substance Use Disorders)Behavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesPrimary care physicians are notresponsible for arranging, referringor authorizing behavioral healthservices. Primary care physiciansmay, however, directly refera member to a BCN-affiliatedbehavioral health provider. It isnot necessary for the primary carephysician to provide a written referralto the behavioral health provider.The behavioral health provider mustcontact the plan for an authorization.Primary care physicians maycall BCN Behavioral Health forassistance in arranging behavioralhealth services for a BCN member.Members in need of behavioralhealth services may either contactan affiliated behavioral healthprovider directly or call the telephonenumber located on the back of theirmember identification card.Mailing address (for claims)BCN HMOSM / BCN AdvantageSMBehavioral Health DepartmentP.O. Box 68753Grand Rapids, MI 49516-8753Utilization Managementbcbsm.com ereferrals.bcbsm.comAugust 2017Provider Inquiry - Behavioral HealthFor.During businesshours.*After businesshours.*Physician-to-physicianreview of determination(Physician Review Line)Phone: 1-877-293-2788Phone: 1-800-482-5982Member with BCNcoverage who is a BlueCross employeePhone: 1-888-265-4703Fax: 1-844-318-5145Calls are answered onlyduring ombudsmanbusiness hours.Member with BCNcoverage who is not aBlue Cross employeePhone: 1-800-482-5982Fax: 1-866-364-7145Phone: 1-800-482-5982Member with BCNAdvantage coveragePhone: 1-800-431-1059Fax: 1-866-364-7145Phone: 1-800-431-1059Member with coveragethrough Blue CrossComplete of MichiganPhone: 1-888-312-5713Fax: 1-888-987-6395Phone: 1-888-312-5713For more information about Blue Cross Complete,visit MiBlueCrossComplete.com/providers.*Business hours for BCN Behavioral Health are Monday – Friday (exceptholidays) 8 a.m. to 5 p.m. except for the ombudsman phone (1-888-265-4703),which is open 8:30 a.m. to 5 p.m.Note: For provider inquiry information related to questions other thanbehavioral health services, refer to the Provider Inquiry (non-behavioralhealth) page in this guide.Web For information on authorizations:Visit ereferrals.bcbsm.com BCN Behavioral Health. For additional information on behavioral health services:Visit bcbsm.com/providers Login BCN Provider Publications andResources Behavioral Health.PreviousHomeNext
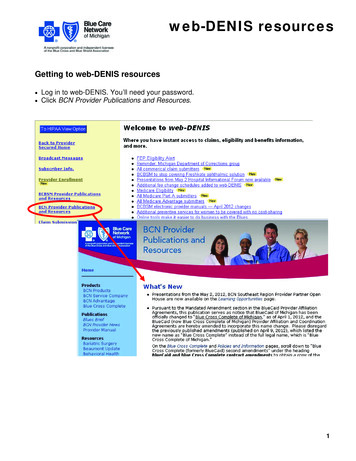
Benefits and EligibilityBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OProviders can use one of themethods outlined on this page tocheck a member’s: Eligibility Benefits Copayments anddeductibles Primary care physicianassignmentComputer-based systemTelephoneTo activate or for technicalassistance: 1-877-258-3932Business hoursMonday – Friday (except holidays)8 a.m. to 8 p.m.Web To register:Visit bcbsm.com/providers Provider Secured Services.Select the appropriate providertype under the “Michiganproviders and facilities: How toget access” heading and followthe instructions. To log in:Visit bcbsm.com/providers LOGIN web-DENIS.Health & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryPharmacyProvider OutreachFor pharmacy inquiries related tobenefits / eligibility, see the ProviderInquiry page in this guide.Quality / Population HealthTravel ServicesProvider InquiryTelephone Facility providers:1-800-249-5103 Professional providers:1-800-344-8525 Hearing / vision providers:1-800-482-4047Business hoursThe automated response system isavailable 24 hours per day / 7 daysper week.WebVisit bcbsm.com/providers Contactus (at the top). Click the desiredlink under either the “Hospitals andfacilities” or the “Physicians andprofessionals” heading.In additon, find Provider Inquiryphone numbers and fax numbers forall products on the Provider InquiryContact Information list.WebVisit bcbsm.com/providers QuickLinks Pharmacy Services.Utilization Managementbcbsm.com ereferrals.bcbsm.comweb-DENISApril 2018PreviousHomeNext
ClaimsBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comYou can use this information to: Submit claims electronicallythrough Electronic DataInterchange Submit hard-copy professionalclaims on CMS-1500 forms tothe address shown on this page Submit hard-copy facility claimson UB-04 forms to the addressshown on this page.To inquire about a claim, do one ofthe following: Check claims status throughthe computer-basedweb-DENIS system. Call the appropriate ProviderInquiry telephone number. Send written inquiries aboutclaims to the appropriateaddress on this page.Note: Some BCN services have aseparate mailing address for claims.See other pages in this guide forinformation on behavioral health;travel and guest member services;DME, medical supplies and P&O;and laboratory services not deliveredin an emergency department or aphysician office.April 2018EDI (electronic datainterchange) submissionAccessing claimsinformation via web-DENISTelephone: 1-800-542-0945, forassistance in submitting claimselectronicallyFor claims tracking, PCP claimssummaries, nonpayment codedescriptions, claims histories, andcontract eligibility, benefit and claimsinformation:Monday – Friday (except holidays)8 a.m. to 4:30 p.m.Visit bcbsm.com/providers QuickLinks Electronic Connectivity(EDI).Paper claim (and writteninquiry) submissionBCN ClaimsP.O. Box 68710Grand Rapids, MI 49516-8710BCN Advantage ClaimsP.O. Box 68753Grand Rapids, MI 49516-8753For information aboutBlue Cross Complete, visitMiBlueCrossComplete.com/providersTelephone: 1-877-258-3932, forassistance (Help Desk)Monday – Friday (except holidays)8 a.m. to 8 p.m.Visit bcbsm.com/providers Provider Secured Services.Accessing claimsinformation via ProviderInquiryTo check the status of a claim or todiscuss a Remittance Advice, callProvider Inquiry. See the ProviderInquiry page in this guide.You can also find Provider Inquiryphone and fax numbers for allproducts on the Provider InquiryContact Information list.PreviousHomeNext
Coordination of BenefitsBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessTo report other insurance,providers should direct themember to log into his or hermember account and submit anonline coordination of benefitsform to BCN. Members canaccess and submit the formonline.Note: It is the member, not theprovider, who must complete theonline coordination of benefitsform and submit it to BCN.Laboratory ServicesTelephone Providers with questions about a member’s coordination of benefitsissues, when BCN is the secondary carrier, can call Provider Inquiry.Refer to the Provider Inquiry page of this document. Members with coordination of benefits questions should call BCNCustomer Service at the number on the back of their ID card.Mailing addressBlue Care Network (or BCN Advantage, as applicable)COB DepartmentMail Code G901611 Cascade West Parkway S.E.Grand Rapids, MI 49546WebVisit bcbsm.com Help Frequently Asked Questions MoreUnderstanding My Benefits FAQs (under Understanding my benefits) What is coordination of benefits?Musculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comJuly 2021PreviousHomeNext
Customer Service (non-behavioral health)Behavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsThe information shown on this page is for members.Members should refer tothe contact information onthe back of their ID cardor access information atbcbsm.com ContactUs Blue Care Networkmembers.Note: For customer serviceinformation related tobehavioral health, referto the Behavioral Healthpage in this guide.Blue Cross CompleteCustomer ServiceFor information about BlueCross Complete CustomerService, visitMiBlueCrossComplete.comand click Contact Us.BCN Advantage CustomerServiceTelephone, for members withindividual coverage1-888-227-2345Telephone, for members with groupor individual coverageUAW Medical Benefits Trust:1-800-222-5992Other: 1-800-450-3680Telephone, for members with groupcoverageU-M Premier Care:1-800-658-8878UAW Medical Benefits Trust:1-800-222-5992Other: 1-800-662-6667TTY for all members: 711Business hoursMonday – Friday(except holidays)8 a.m. to 5:30 p.m.Mailing addressBCN Customer ServiceP.O. Box 68767Grand Rapids, MI49516-8767Provider InquiryProvider OutreachQuality / Population HealthTravel ServicesTTY for all members: 711Business hoursMonday – Friday8 a.m. to 8 p.m.,with weekend hours available Oct.1through March 31Mailing addressBCN Advantage Customer ServiceMail Code C103P.O. Box 5043Southfield, MI 48086WebVisit bcbsm.com Contact Us Medicare and Medigap members.WebVisit bcbsm.com Contact Us BlueCare Network members.Utilization Managementbcbsm.com ereferrals.bcbsm.comBCN HMO (commercial)Customer ServiceAugust 2018PreviousHomeNext
DME, Medical Supplies and P & OBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessFor outpatient durablemedical equipment,medical suppliesand prosthetics andorthotics, BCN contractswith different vendors,depending on themember’s plan or productand the type of item.Refer to the informationon this page to identify theappropriate vendor.Laboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthDiabetic supplies(not including diabeticshoes and inserts)DME and P&O(including diabetic shoesand inserts)VendorJ&B Medical SupplyVendorNorthwood, Inc.TelephoneVoice: 1-888-896-6233TTY: 1-800-737-0084TelephoneVoice: 1-800-393-6432TTY: ness hoursMonday – Friday8 a.m. to 5 p.m.Business hoursMonday – Friday8:30 a.m. to 5 p.m.Mailing addressJ&B Medical, Inc.50496 West Pontiac TrailWixom, MI 48393Mailing addressNorthwood, Inc.7277 BerniceCenter Line, MI 48015WebVisit jandbmedical.com.WebVisit northwoodinc.com.Blue CrossCompleteFor Blue Cross Completevendor contact information,see the Blue CrossComplete Provider Manualat MiBlueCrossComplete.com/providersNote: Call Northwoodto identify a contractedsupplier. The suppliersubmits the request toNorthwood for review.Travel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comBCN HMO (commercial)and BCN AdvantageJune 1, 2018PreviousHomeNext
Health & WellnessBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthHealthy living informationthrough Blue Cross Health& WellnessBCN Chronic Condition Management departmentThe Blue Cross Health & Wellnessprogram, powered by WebMD , isavailable 24 hours a day, every day,through bcbsm.com.Business hoursMonday – Friday (except holidays), 8:30 a.m. to 5 p.m.This online service offers informationon health and wellness as well ashelpful online tools and resources.Through Blue Cross Health &Wellness, members can use thefollowing resources: Health assessmentDigital Health AssistantWebMD Health RecordMessagingWebMD Weigh TodaySMDevice and app integrationHealth trackersWebMD message boardexchange WebMD tobacco cessationcoachingTelephone1-800-392-4247WebVisit bcbsm.com Health and Wellness (under For Members) Learn More(under Chronic condition management) Chronic condition managementprograms (under Blue Care Network).Mailing addressBCN Chronic Condition ManagementMail Code C336P.O. Box 5043Southfield, MI 48086-5043Travel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comNovember 2016PreviousHomeNext
Laboratory ServicesBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesContact Joint Venture Hospital Laboratories,BCN’s contracted provider for outpatient laboratoryservices, for the following:Note: This applies to outpatient laboratory servicesin locations other than physician offices. To locate a client service center nearest youTo inquire about billingTo obtain test resultsTo request materialsNote on facility claims: The following are payable byBCN: ER laboratory services Laboratory services for observation stays,when submitted on the observation claim.(Note: This does not apply to BCN usiness HoursMonday – Friday (except holidays), 8 a.m. to 4:30 p.m.Mailing addressJVHL999 Republic Drive, Suite 300Allen Park, MI 48101WebVisit Joint Venture Hospital Laboratories at jvhl.org.PT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comApril 2016PreviousHomeNext
Musculoskeletal ServicesBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachTurningPoint HealthcareSolutions, LLC, managesauthorizations for certainmusculoskeletal surgical andother related procedures forBCN HMO and BCN Advantagemembers. These include:For dates of service on or afterJuly 1, 2020: Knee arthroscopy Cervical and lumber spinesurgery Joint replacement (knee, hip,shoulder) Spinal cord stimulator(neurostimulator) Epidural or intrathecal catheter Other musculoskeletalproceduresFor dates of service on or afterJan. 1, 2021: Pain managementQuality / Population HealthWebFor information on how to submit prior authorizationrequests to TurningPoint, refer to the documentMusculoskeletal procedure authorizations: Frequently askedquestions for providers.Note: Look at the question “Should I submit authorizationrequests directly to TurningPoint?”For a list of the procedure codes associated with theservices that require review by TurningPoint, refer to thedocument Musculoskeletal procedure codes that requireauthorization by TurningPoint.This list shows where to submit authorization requests fordates of service that occurred before TurningPoint beganmanaging the authorizations for those services.For more information, visit ereferrals.bcbsm.com BCN Musculoskeletal Services.Business hoursMonday – Friday, 8 a.m. to 8 p.m., Eastern timeContact informationProvider Relations Support Team Email: BCBSMProviderRelations@tpshealth.com Phone: 313-908-6041Travel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comOctober 2020PreviousHomeNext
Pharmacy ServicesBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comWith this information you can: Access information on theformulary, including thequality interchange program,formulary alternatives,quantity limits, genericsubstitution and drugcoverage Get help with pharmacyclaims processing issues Inquire about and requestprior authorization, benefitexception or urgent review ofpharmacy servicestheir member ID card.Mail-order optionsPharmacy Help DeskFor most medications For new prescriptions, callExpress Scripts at1-888-Easy-RX1(1-888-327-9791) for a faxform. For refills, call Express Scriptscustomer service at1-800-229-0832.For drugs covered under themedical benefit, refer to BCN’sMedical Benefit Drugs - Pharmacypage at ereferrals.bcbsm.com.Mailing address -- BCN HMO(commercial)BCN Pharmacy Help DeskP.O. Box 321127-511FDetroit, MI 48232-1127This information applies to BCNHMO and BCN Advantagemembers. For Blue CrossComplete pharmacy information,refer to the Blue CrossComplete Provider Manual atMiBlueCrossComplete.com/providersNote: The telephone numbersshown on this page are forproviders only. Members shouldrefer to the Customer Servicecontact information on the back ofDecember 2017Business hours24 hours a day, 7 days a weekPrior authorization requestsTelephone: 1-800-437-3803Fax: For BCN HMO (commercial),including self-funded plans:1-877-442-3778 For BCN Advantage:1-800-459-8027Mailing address -- BCN AdvantageBCN Advantage Pharmacy HelpDeskMail Code 1610P.O. Box 32877Detroit, MI 48232-1127For specialty medicationsWalgreens Specialty Pharmacy, LLCTelephone: 1-866-515-1355Fax: 1-866-515-1356Other informationClaims processing questions:Express Scripts Pharmacy ServicesHelp DeskTelephone: 1-800-922-1557Benefit / eligibility questionsrelated to pharmacy services:See the Provider Inquiry page.WebVisit bcbsm.com/providers QuickLinks Pharmacy Services.PreviousHomeNext
Physical, Occupational and Speech Therapy ServicesBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthBCN contracts with eviCorehealthcare to manageauthorizations for membersreceiving physical, occupationaland speech therapy services inoffice and outpatient settings,including outpatient hospitalsettings.eviCore also manages physicalmedicine services delivered toBCN HMO members only: By chiropractors By athletic trainers, for datesof service on or after Jan. 1,2021Note: This informationapplies to both BCN HMOand BCN Advantage membersunless otherwise noted.For Blue Cross Completeinformation, refer to the BlueCross Complete Provider Manualat MiBlueCrossComplete.com/providersProcesseviCore healthcareSubmit prior authorizationrequests for both initial and followup treatment visits to eviCorehealthcare using one of themethods described in the Outpatientrehabilitation services frequentlyasked questions document.Prior Authorization Call CenterTelephone: 1-855-774-1317Monday – Friday (except holidays)8 a.m. to 7 p.m.Note: Initial evaluations do notrequire authorization.Other resourcesClick the links below to accessadditional information: BCN’s Outpatient PT, OT, STpage at ereferrals.bcbsm.com Utilization Management chapterof the BCN Provider Manual.Look in the section titled”Managing PT, OT and ST /Managing physical medicineservices.”CriteriaTo see the criteria eviCore usesto make determinations onauthorization requests:1. Open eviCore’ s ClinicalGuidelines webpage.2. Click Musculoskeletal: Therapies.3. Enter “Blue Care Network” as thehealth plan.4. Click the search icon.5. Click to open the desired criteriaset.WebVisit: evicore.com eviCore’s Blue Care Networkresources page atwww.evicore.comTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comOctober 2020PreviousHomeNext
Provider Enrollment and Change RequestsBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STThe process and formsused in enrolling andupdating information varywith the type of practitioner/ provider and the specificBlue Cross and BCNnetwork affiliation.For all providersAll the necessaryinformation is available atbcbsm.com/providers Quick Links Enrollment,Changes and Access Enrollment and Changes.Mailing addressBlue Cross Blue Shield of MichiganProvider Enrollment and DataManagementMail Code C301600 East LafayetteDetroit, MI 48226To enroll with or updateinformation for BlueCross Complete, 800-822-2761Fax1-866-900-0250Provider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comApril 2021PreviousHomeNext
Provider Inquiry (non-behavioral health)Behavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comContact Provider Inquiry to get helpwith general questions such as: Claim inquiries Member benefits information Primary care physicianassignmentsBCN HMO and BCNAdvantage ProviderInquiryMailing addressBlue Care NetworkGeneral CorrespondenceP.O. Box 68827Grand Rapids, MI 49516-8827WebVisit bcbsm.com/providers Contact us (at the top). Clickthe desired link under either the“Hospitals and facilities” or the“Physicians and professionals”heading.Provider Inquiry phone and fax numbers – all productsFor.During business hours.After businesshours.Member withPhone: 1-888-265-4703BCN coverageFax: 1-844-318-5145who is a BlueCross employeeCalls are answered onlyduring ombudsmanbusiness hours(Monday through Friday— except holidays —8:30 a.m. to 5 p.m.).Member withBCN HMO orBCN Advantagecoverage who isnot a Blue CrossemployeeThe automatedresponse system isavailable 24 hoursa day, seven days aweek.Call the appropriate Provider Inquirynumber: Facilities in Michigan:1-800-249-5103 Professional providers inMichigan: 1-800-344-8525 Hearing / vision providers:1-800-482-4047Provider Inquiry fax numbers: BCN HMO: 248-799-6969 BCN Advantage: 1-866-364-0080However, providerscan be connectedwith a Provider Inquiryrepresentative onlyduring business hours(Monday through Friday— except holidays —from 8 a.m. to 5 p.m.).Note: For provider inquiry information related to behavioral health services,refer to the Behavioral Health page in this guide.Blue Cross CompleteProvider InquiryFor information on BlueCross Complete, visitMiBlueCrossComplete.com/providersApril 2018PreviousHomeNext
Provider OutreachBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comContact Provider Outreach to gethelp with: Contractual issues Recurring problems orunresolved issues Education and training onBCN policies, procedures andprograms Discussion of primary groupadministration Changes in primary carephysician acceptance codes Requests for coverage /on-call providersVisit bcbsm.com/providers ContactUs (at the top). Click the desiredlink under either the “Hospitals andfacilities” or the “Physicians andprofessionals” heading.East / Mid / SoutheastEast and Mid Michigan — LansingMail Code L09C232 S. Capitol Ave.Lansing, MI 48933Southeast — SouthfieldMail Code C30220500 Civic Center Dr.Southfield MI 48076West / Upper peninsulaWest Michigan — Grand RapidsMail Code G20686 Monroe Center NWGrand Rapids, MI 49503West Michigan — Traverse CityMail Code B210202 E. State St., Suite 200Traverse City, MI 48694Upper peninsulaTelephone: 1-866-497-7647Fax: 906-228-6588Mail Code B108415 McClellan Ave.Marquette, MI 49855-5506For primary care physicians in amedical care group, look on the listof physician organization consultantsto find your consultant.For other practitioners, reviewthe regional map for professionalproviders or the regional map forfacilities. Click your region on themap to see a list of professional orfacility consultants.March 2021PreviousHomeNext
Quality and Population HealthBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STThe BCN Quality and Population Healthdepartment oversees activities relatedto: Quality of care / service concerns Clinical practice and preventivecare guidelines Coordination of accreditation andregulatory standards HEDIS * measures and initiatives Physician / provider medical recordreviews Facility reviews Physician office education Quality outcome measures Health promotion / education(including worksite wellnessprograms, community health fairs) Risk 8-455-2808Business hoursMonday – Friday, 8 a.m. to 4:30 p.m.Mailing address for quality management issuesBlue Care NetworkQuality ManagementMail Code C330P.O. Box 5043Southfield, MI 48076-5043Provider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Management*HEDIS is a registered trademark of the NationalCommittee for Quality Assurance.bcbsm.com ereferrals.bcbsm.comApril 2018PreviousHomeNext
Travel ServicesBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsUse the contact information onthis page to: Check eligibility Obtain benefit information Submit claimsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessBCN members can use thenationwide network of Blue planproviders for health care needswhile traveling outside of Michigan.Out‑of‑state Blue Cross BlueShield members can have urgentand follow-up care services whiletraveling within Michigan.BCN and out‑of‑state Blue CrossBlue Shield HMO members canarrange treatment with a traditionalprovider who participates with BlueCross Blue Shield plans.Laboratory ServicesMusculolskeletal ServicesPharmacy ServicesMailing address – professionalclaimsBlue Cross Blue Shield of MichiganClaimsP.O. Box 312500Detroit, MI 48231-2500Mailing address – facility claimsBlue Cross Blue Shield of MichiganClaimsP.O. Box 310166Detroit, MI 48231-0166Business hours7 days a week, 24 hours a dayPT, OT and STProvider Enrollment andChange RequestsTelephone To check membership andeligibility, call1-800-676-BLUE (2583).Provide the operator with thethree‑character prefix on theID card. To find a provider, call1-800-810-BLUE (2583) or goto bcbs.com and click on theFind a Doctor link.Provider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization Managementbcbsm.com ereferrals.bcbsm.comTravel services for BCNmembersMay 2022PreviousHomeNext
Utilization ManagementBehavioral HealthBenefits and EligibilityClaimsCoordination of BenefitsCustomer ServiceDME, Medical Suppliesand P & OHealth & WellnessLaboratory ServicesMusculolskeletal ServicesPharmacy ServicesPT, OT and STProvider Enrollment andChange RequestsProvider InquiryProvider OutreachQuality / Population HealthTravel ServicesUtilization ManagementBCN Utilization Management manages the following: Acute IP admissions / concurrent reviews Home health care services for BCN commercialmembers, for providers not contracted with BCN.Note: CareCentrix manages home health careauthorizations for BCN Advantage members. Home TPN and enteral feedings Post-acute care for BCN commercial membersNote: naviHealth manages post-acute careauthorizations for BCN Advantage members. Referral management Review of potential quality variances and seriousadverse events Transplant evaluations Social work services Review of provider appealsNote: All requests must include clinical information.For after-hours utilization management assistance, call1-800-851-3904 to: Determine alternatives to inpatient admissions Arrange for DME and for emergen
the address shown on this page Submit hard-copy facility claims on UB-04 forms to the address shown on this page. To inquire about a claim, do one of the following: Check claims status through the computer-based web-DENIS system. Call the appropriate Provider Inquiry telephone number. Send written inquiries about