Transcription
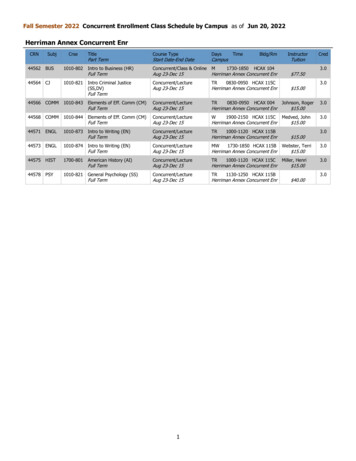
THURSDAY CONCURRENT SESSION #1S-1.Effects of Hormone Therapy on Heart Fat and AtherosclerosisProgression in Recently Postmenopausal Women from KEEPS TrialSamar R. El Khoudary, PhD, MPH1, Qian Zhao1, JoAnn E. Manson2, Maria M. Brooks1,Nanette Santoro3, Dennis M. Black4, Mitchell Harman7, Marcelle I. Cedars4, Paul N.Hopkins8, Ann E. Kearns6, Virginia Miller6, Hugh S. Taylor9, Matthew J. Budoff5.1University of Pittsburgh, Pittsburgh, PA; 2Harvard Medical School and Brigham andWomen’s Hospital, Boston, MA; 3University of Colorado, Aurora, CO; 4Universityof California San Francisco, San Francisco, CA; 5Los Angeles Biomedical ResearchInstitute, Torrance, CA; 6Mayo Clinic, Rochester, MN; 7Phoenix Veterans AffairsHealth Care System, Phoenix, AZ; 8University of Utah Health, Salt Lake City, UT;9Yale University, New Haven, CTObjective: Heart fat depots, within [epicardial adipose tissue (EAT)] and outside[paracardial adipose tissue (PAT)] the pericardium, have been linked to increasedcardiovascular disease risk. Postmenopausal women have greater volumes of heart fatthan premenopausal women. Recent evidence suggests a role of endogenous estrogenin heart fat accumulation, possibly limited to PAT. The impact of hormone therapy(HT) on heart fat buildup is unknown. We evaluated the differential effects of HTon the accumulation of heart fat depots and their associations with coronary arterycalcification (CAC) progression in recently postmenopausal women. Design: KEEPSwas a multi-center, randomized, clinical trial of the effects of oral conjugated equineestrogens (o-CEE) and transdermal 17β-estradiol (t-E2), both with progesterone,compared to placebo, on 48-month subclinical atherosclerosis progression in recentlypostmenopausal women. Heart fat volumes and CAC were measured on CT scans atbaseline and 48 months later. Significant CAC progression was defined as present if (1)baseline CAC score 0 and 48 month CAC Agatston score 0 ; (2) baseline CAC score 0 to 100 and annualized change in CAC score 10 ; or (3) baseline CAC score 100and annualized percent change in CAC score 10%. Changes in heart fat depots weretested using Wilcoxon signed test and compared by treatment group using Kruskal–Wallis test. Associations between change in heart fat volumes and CAC progression aswell as effect modification by HT type were tested using logistic regression adjustingfor age, race, study site, education, physical activity, smoking, alcohol intake, lipids,systolic blood pressure, waist circumference, anti-hypertensive medications and baselineheart fat volume. Results: Of 727 randomly assigned women, 474 [mean age (SD):52.7(2.6); 78.1% White] had heart fat volumes and CAC scores at baseline and 48months. EAT volume increased significantly over time in the placebo group [median(Q1, Q3): 2.12(-4.58, 6.36) cm3, P 0.003] but not in the o-CEE [-0.05(-5.93, 6.12)cm3, P 0.99] or the t-E2 group [1.68(-4.07, 4.91) cm3, P 0.07]. PAT volume did notchange significantly in any group. Changes in EAT and PAT did not vary by treatmentgroup. KEEPS only included women whose screening CAC score was 50, resulting in88.4% of participants having CAC 0 at baseline. At 48 month CAC progressed in 14%of the study participants. Changes in EAT and PAT were not significantly associatedwith CAC progression overall. However, assigned treatment significantly modified theassociation between changes in PAT and CAC progression in adjusted model, P 0.02,such that changes in PAT were associated with greater CAC progression risk only int-E2 group [OR (95% CI) per 1 SD of PAT change: 2.8(1.3, 5.9)]. Conclusion: Therewas no significant difference among treatment groups in 48 month changes of heartfat depots. However, there was a suggestion that O-CEE slowed progress on heart fataccumulation, although not in the t-E2 group. Greater PAT changes were associated withgreater CAC progression risk only in the t-E2 group. The current findings support thenotion that EAT and PAT are distinct fat depots and suggest a complex role of HT in theaccumulation of heart fat depots and their associations with CAC progression in recentlypostmenopausal women.Sources of Funding: KEEPS: Aurora Foundation to the Kronos Longevity ResearchInstitute, NIH P50 AG 44170 to VMM, 1 UL1 RR024150, Mayo CTSA 1 UL1RR024150, the Mayo Foundation, CTSA UL1 RR024139, UL1 RR024131 fromthe NCRR. Study medications: supplied in part by Bayer Health Care and by AbbottPharmaceuticals. The ClinicalTrials.gov number is NCT00154180. KEEPS Heart FatAncillary study: NHLBI R21HL140011.S-2.Effects of Single-Capsule 17β-Estradiol/Progesterone (TX-001HR) onMetabolic Parameters and Cardiovascular Outcomes in MenopausalWomen of the REPLENISH TrialRogerio Lobo, MD1, James Liu, MD2, Andrew M. Kaunitz, MD3, Brian Bernick, MD4,Shelli Graham, PhD4, Ginger Constantine5, Sebastian Mirkin, MD4. 1Columbia UniversityMedical Center, New York, NY; 2University Hospital Cleveland Medical Center,Cleveland, OH; 3University of Florida College of Medicine-Jacksonville, Jacksonville,FL; 4TherapeuticsMD, Boca Raton, FL; 5EndoRheum Consultants, LLC, Malvern, PAObjective: TX-001HR (TherapeuticsMD, Boca Raton, FL), an investigational productthat combines 17β-estradiol and progesterone (E2/P4) in a single, oral softgel capsule,significantly reduced the frequency and severity of moderate-to-severe vasomotorsymptoms (VMS) in menopausal women of the REPLENISH trial (Lobo et al, ObstetGynecol 2018, in press). The objective of this report is to summarize safety endpointsrelated to metabolic parameters and cardiovascular outcomes from REPLENISH.Design: REPLENISH (NCT01942668) was a phase 3, randomized, double-blind,placebo-controlled, multicenter trial that evaluated 4 TX-001HR doses vs placebo inmenopausal women (40-65 years) with a uterus. Women were randomized to E2/P4doses or placebo in a proportion of 11:1. Clinical laboratory measurements were takenat baseline, week 12 and months 6, 9 and 12. Changes from baseline to month 12 in lipidand coagulation parameters, blood glucose, and cardiovascular events are summarizeddescriptively. Results: 1835 women were randomized and took 1 capsule of dailyE2/P4 (mg/mg) of 1/100 (n 415), 0.5/100 (n 424), 0.5/50 (n 421), 0.25/50 (n 424) orplacebo (n 151). Total cholesterol and LDL-cholesterol levels numerically decreasedfrom baseline to month 12, HDL-cholesterol levels remained similar to baseline andtriglycerides levels increased (Table). Few women had triglycerides and cholesterolincreases ( 50 mg/dL or above normal levels) at 12 months with TX-001HR (6-11% and1-4%, respectively) vs placebo (7% and 3%). Fasting glucose levels remained similarto baseline at 12 months. Antithrombin activity and factor XIV and protein S levelstended to decrease from baseline compared with placebo, and time for activated partialthromboplastin, prothrombin time, fibrinogen levels and prothrombin internationalnormalized ratio remained similar to baseline at 12 months. Two women experienced“coronary heart disease” adverse events considered not related to treatment: unstableangina in one subject (E2/P4 0.5/50), and angina and coronary artery disease inanother (E2/P4 1/100). The woman who experienced unstable angina also experiencedsubarachnoid hemorrhage and cerebellar infarction, neither considered treatment related.One case of deep vein thrombosis (DVT) with E2/P4 0.5/50 was reported in a womanwith a family history of DVT. Conclusion: Twelve months of TX-001HR treatment inmenopausal women with VMS and an intact uterus had minimal clinically meaningfuleffects on lipid, glucose, or coagulation parameters. Observed changes in triglyceridelevels, antithrombin activity, factor XIV, and protein S were consistent with oral estrogentherapy. Although this trial lacked statistical power to assess these outcomes, VTE rates,cardiovascular disease, and cerebrovascular events were as expected for a postmenopausalpopulation. If approved, TX-001HR may provide the first oral combination of E2/P4 forthe treatment of VMS in menopausal women with a uterus.Sources of Funding: TherapeuticsMDaPTT: activated partial thromboplastin time; INR: international normalizedratio.S-3.Evaluation of Systemic Effects of a Vaginal Estradiol Softgel Capsule(TX-004HR) in Menopausal Women with Moderate-to-Severe DyspareuniaLisa C. Larkin MD, MD5, Andrew M. Kaunitz, MD1, James Liu, MD2, Shelli Graham,PhD3, Brian Bernick, MD3, Sebastian Mirkin, MD3, Ginger Constantine4. 1Universityof Florida College of Medicine-Jacksonville, Jacksonville, FL; 2University HospitalsCleveland Medical Center, Cleveland, OH; 3TherapeuticsMD, Boca Raton, FL;4EndoRheum Consultants, LLC, Malvern, PA; 5Lisa Larkin MD and Associates,Mariemont, OHObjective: TX-004HR (an investigational, vaginal softgel capsule of low-dose,solubilized 17β-estradiol, designed to be mucoadhesive and rapidly dissolving)significantly improved vaginal physiology and dyspareunia (primary endpoints) as well asdryness (secondary enpoint) in menopausal women with moderate-to-severe dyspareuniaas their most bothersome symptom in the phase 3 REJOICE trial (NCT02253173). 1Improvements were achieved with negligible to very low systemic absorption ofestradiol with doses of 4 µg, 10 µg and 25 µg (the 4 µg and 10 µg doses have beensubmitted for FDA approval).2 Systemic levels of estradiol with 10 µg and 25 µg doseswere shown to be lower than with the same doses of a commercially available vaginalestradiol tablet (Vagifem ) in head-to-head studies.3 This report summarizes the effectsof TX-004HR on clinical outcomes that previously have been reported to be influenced
by systemic estradiol absorption.4 Design: REJOICE was a randomized, double-blind,placebo-controlled, multicenter study that evaluated 4 µg, 10 µg, and 25 µg TX-004HRversus placebo in menopausal women (40-75 years) with vulvar and vaginal atrophy(VVA) and moderate-to-severe dyspareunia. Safety endpoints (cardiovascular [CV] andbreast effects and venous thromboembolism [VTE]) in the total population that could beaffected by systemic estradiol absorption were assessed. Twelve-lead electrocardiograms(ECGs) and breast exams were performed at baseline and week 12. Treatment-emergentadverse events (TEAEs) of special interest were summarized descriptively. Serum sexhormone binding globulin (SHBG) was measured at baseline and weeks 2 and 12 in asubset of women (n 72). Results: From the safety population, 764 women (mean age59 years) were randomized to 4 µg (n 191), 10 µg (n 191) or 25 µg TX-004HR (n 190),or placebo (n 192). Seven CV TEAEs were reported (Table 1): complete heart block,palpitations, and sinus node dysfunction as well as sinus bradycardia and first degreeatrioventricular block identified in one woman at the end of study that were consideredmild. Only the 2 cases of palpitations were considered possibly related to treatment.No CHD, VTE or other thrombotic episodes were reported. There were no treatmentrelated, clinically significant adverse ECG changes. Two women in the 4 μg TX-004HRgroup had reports of mild hypertension as a TEAE. Three women (n 1 each; 4 μg,10 μg, placebo) had mild blood pressure increases reported as TEAEs; one was considerednot treatment related (10 μg), while the others were considered possibly related. Tenbreast-related TEAEs were reported (Table 1), of which 6 occurred with placebo; allbut two (breast mass and fibrocystic breast with placebo) were considered as possibly orprobably related to treatment. Other than these TEAEs, no clinically significant breastevents were reported. Changes from baseline for SHBG with TX-004HR ranged from1.9 16.6 to 3.0 11.7 nmol/L at week 2 and -0.6 16.0 to 4.4 27.0 nmol/L at week 12,and were comparable to changes with placebo at the same time points (-2.1 11.7 and10.2 41.7 nmol/L, respectively), with no dose-related pattern. Conclusion: Evidenceof systemic effects of TX-004HR was not observed in the 12-week REJOICE trial. Noclinically meaningful differences in cardiovascular or thrombotic-related adverse events,or blood pressure were found between TX-004HR and placebo. Lastly, there was noevidence of estrogen-related clinical outcomes or liver metabolism such as an increase inserum SHBG suggesting systemic absorption. 1Constantine G, et al. Menopause 2017;24:409-416 2Archer DF, et al. Menopause 2017;24:510-516 3Pickar JH, et al. Climacteric2016;19:181-187 4Pickar JH, et al. Expert Opin Drug Saf 2017;16:941-954Sources of Funding: TherapeuticsMDTreatment-emergent Adverse EventsS-5.Comparing written and verbal delivery of a treatment regimen to womenwith overactive bladder: single-blinded, randomized controlled trialLindsay Shirreff, MD, FRCSC, MSc(HQ)1, Michelle Anderson2, Colleen McDermott,MSc, MD, FRCSC1. 1Obstetrics and Gynaecology, Mount Sinai Hospital, Toronto, ON,Canada; 2University of Toronto, Toronto, ON, CanadaObjective: Overactive bladder (OAB) is a common condition among older womenrequiring a multifaceted treatment approach, usually communicated by physician topatient in the clinic setting. The objective of this two-centre, single-blinded, randomizedcontrolled trial was to determine if a written list of six management strategies for OABimproves both immediate and delayed recall of these recommendations compared to atraditional, verbal discussion. Design: Between May 2016 and February 2018, womennewly diagnosed with OAB were randomized to either the intervention group wherethey received a transcribed list of six treatment recommendations or to the controlgroup where the same six recommendations were communicated only verbally by theirphysician. Patients in both groups were asked to recall treatment recommendationsimmediately following their appointment and two weeks later. A score out of sixwas assigned at each time point based on the number of recommendations patientscould remember. Scores at each point of recall were compared between groups.Results: For those recruited to the study (n 60) and randomized, there were nosignificant differences between group demographics for age, education, income, orlanguage. Immediate total recall scores on treatment recommendations were significantlybetter for those who received the handwritten list compared to those who received onlyverbal communication (P 0.004). There was no difference in two-week total recall scoresbetween groups. Recall scores compared for each of the six recommendations were notsignificantly different between the written and verbal recommendations at immediateor two-week follow up. Conclusion: A written list of recommendations can improveOAB patients’ immediate recall of a suggested treatment regimen but does not impactrecall two weeks later. Distributing written lists in the ambulatory setting may have thepotential to improve quality and delivery of care for OAB patients.Sources of Funding: A departmental grant from Mount Sinai Hospital (Department ofObstetrics and Gynaecology) was awarded to support this project.THURSDAY CONCURRENT SESSION #2S-6.Caucasian women have greater gains in subcutaneous abdominaladiposity in the years leading up to menopause compared to AfricanAmerican womenS-4.Effect of age, time since menopause and previous hormone therapy on theresponse to intravaginal 6.5 mg prasteroneDavid Archer, MD1, Fernand Labrie2, Celine Martel2, Érick Moyneur3. 1CONRADClinical Research Center, Norfolk, VA; 2Endoceutics Inc., Quebec, QC, Canada; 3StatlogEconometrics Inc., Montreal, QC, CanadaObjective: To analyse the effect of intravaginal 6.5 mg prasterone (Intrarosa ) insubgroups who participated in the clinical trials performed with women sufferingfrom moderate to severe (MS) pain at sexual activity (dyspareunia) identified as theirmost bothersome symptom (MBS) of vulvovaginal atrophy (VVA). This analysisintends to assess the potential influence of age, time since menopause, and previoushormone therapy (HRT) on the response to treatment. Design: Data obtained from twoindependent prospective, randomized, double-blind and placebo-controlled clinical trialswere combined to evaluate the effect of daily intravaginal 6.5 mg (0.50%) prasteroneadministered for 12 weeks on MS/MBS dyspareunia in different subgroups of womendepending on their age ( 55 yrs and 56 yrs), time since menopause (1-2 yrs, 3-5 yrsand 6 yrs) and had or not received previous HRT. Results: In 406 women treated with6.5 mg prasterone and 234 women who received placebo, the difference from placeboin the improvement of the severity score of MS/MBS dyspareunia was of 0.44 unit and0.36 unit in women aged 55 yrs [n 123; 57] and 56 yrs [n 283; 177], respectively.On the other hand, the improvement of MS/MBS dyspareunia was of 1.59, 0.59 and0.27 unit for prasterone in comparison to placebo in women who were menopausal since1-2 yrs [n 22; 11], 3-5 yrs [n 59; 27], and 6 yrs [n 325; 196], respectively. Finally,women who previously received HRT [n 184; 115] before taking intravaginal prasteronehad an improvement of their MS/MBS dyspareunia of 0.45 unit over placebo incomparison to a difference from placebo of 0.32 unit in women who did not receive HRTpreviously [n 222; 119]. Conclusion: No major influence of age and previous hormonetherapy was observed on the response to intravaginal 6.5 mg prasterone (Intrarosa ). Thesmaller effect on dyspareunia observed with a longer time since menopause deservesfurther investigation in order to optimize treatment.Sources of Funding: This study was funded by Endoceutics Inc.Kara Marlatt, PhD, MPH1, Robbie Beyl, PhD1, Jennifer Lovejoy, PhD3, Steven Smith,MD2, Leanne Redman, PhD1. 1Pennington Biomedical Research Center, Baton Rouge,LA; 2Translational Research Institute for Metabolism and Diabetes, Orlando, FL;3Arivale, Inc., Seattle, WAObjective: Menopause is characterized by estrogen deficiency and results incommensurate metabolic changes (e.g., weight gain, increased abdominal adiposity,insulin resistance). The differential impact of the menopause transition in differentraces, particularly among African-Americans (AA), is not well understood. Many healthstatistics for AA women are significantly worse compared to Caucasians; therefore,understanding the deleterious impact of menopause on metabolic health among womenof different races is of great public health significance. The Healthy Transitions study(R01: ‘Menopause Effect on Obesity, Energy Balance, and Insulin’) was a pioneering,prospective cohort study conducted between 1997-2006 at the Pennington BiomedicalResearch Center with the overall objective to examine the impact of menopause onchanges in body composition, fat distribution, and cardiometabolic risk factors in AAand Caucasian women. Design: Ninety-four healthy women (25 AA, 69 Caucasian)were phenotyped annually for up to 7 y for changes in body composition, abdominalfat distribution, and hormone levels. At enrollment, women were aged 43 y or olderand pre-menopausal (i.e., had at least five menstrual periods in the prior 6 monthsand follicle-stimulating hormone (FSH) 30 mIU/mL). Women taking hormones wereexcluded. All women in the present analysis transitioned through menopause (indicatedas Year 0) during follow-up, which was defined by absence of menstruation for 1-y andFSH 30 mIU/mL. Annual assessments included: (1) body composition (fat mass, fat-freemass) by Hologic QDR2000 DXA; (2) abdominal fat distribution including subcutaneousadipose tissue (SAT), deep (dSAT) and superficial (sSAT), visceral adipose tissue (VAT),and total adipose tissue (TAT) by computed tomography; (3) fasting blood collectionfor quantitative insulin-sensitivity check index (QUICKI); and (4) hormone levels.Results: At menopause onset, women overall had a mean age 53 2 y and BMI 27.0 5.8 kg/m2. As expected, estradiol decreased and FSH increased throughout the menopausetransition. Compared to the pre-menopausal state (2-6 years before menopause), womenweighed significantly more at menopause onset, characterized by greater total fatmass and increased abdominal SAT, VAT, and TAT (all p 0.05 from Year 0). In the2-6 years before menopause, Caucasian women had significant increases in weight, fatmass, SAT, dSAT, sSAT, VAT, and TAT (all p 0.05 from Year 0) compared to AA women(Fig. 1, all p 0.05). No significant between-race differences in fat-free mass, VAT,estradiol, FSH, or QUICKI were observed. At menopause, AA women weighedsignificantly more than Caucasians, but no other between-race differences in bodycomposition, QUICKI, or hormones were observed. Conclusion: The menopausetransition may impact Caucasian women more than AA women in terms of subcutaneousadipose tissue deposition. No race differences in body composition were observed at
menopause onset which suggests that AA women had a worse pre-menopause bodyadiposity profile yet maintained adiposity levels throughout the menopause transitionwhile Caucasian women caught up in body adiposity.Sources of Funding: NIH Grant #s: NIDDK-R01-DK50736A (PI: Lovejoy); NIDDKT32-DK064584 (to Marlatt); U54-GM104940 (LA CaTS). Registered trial onClinicalTrials.gov (Healthy Transitions; NCT00412269).S-7.Increased Anxiety and Depressive Symptoms Are Associated withAbnormal Resting Cardiac Autonomic Function in Peri- andPostmenopausal Women with Hot FlashesPolly Fu, MD1, Carolyn Gibson, PhD, MPH1,2, Wendy Mendes, PhD3, Michael Schembri,BS4, Alison Huang, MD, MAS, MPhil1. 1Department of Medicine, University ofCalifornia San Francisco, San Francisco, CA; 2San Francisco Veterans Affairs HealthCare System, San Francisco, CA; 3Department of Psychiatry, University of California SanFrancisco, San Francisco, CA; 4Department of Obstetrics, Gynecology, and ReproductiveSciences, University of California San Francisco, San Francisco, CAObjective: The menopause transition is marked by an increased prevalence of moodsymptoms in midlife women, including anxiety and depression. Prior research innon-menopausal populations have suggested that both anxiety and depression may beassociated with alterations in cardiac autonomic function that are in turn associatedwith cardiovascular disease or adverse cardiovascular outcomes. We aimed to examinewhether anxiety and depressive symptoms are associated with an adverse cardiacautonomic profile among midlife women with hot flashes. Design: The MenopausalTreatment Using Relaxation Exercise (MaTURE) trial was a parallel-group, singleblinded, randomized trial of slow-paced respiration for treatment of hot flashes inperi- and postmenopausal women, age 40 to 59 years old, with at least four hot flashesreported per day. Anxiety and depressive symptoms were assessed as continuous scoreson multiple validated self-administered questionnaires. State anxiety (i.e., fluctuating,transitory emotional state in reaction to perceived threats) and trait anxiety (i.e., stableindividual tendency towards perceived threats) were measured using the SpielbergerState Trait Anxiety Inventory (STAI). Cognitive anxiety (i.e., mental component ofanxiety associated with fear of future adverse events) was assessed using the anxietysubscale of the Hospital Anxiety and Depression Scale (HADS). Depressive symptomswere assessed using Beck Depression Inventory-II (BDI-II) and the depression subscaleof HADS. Main outcomes of cardiac autonomic function included pre-ejection period(PEP) and respiratory sinus arrhythmia (RSA), both measured during a resting periodat baseline and 12 weeks using impedance cardiography and electocardiography. PEP,the time from the start of cardiac ventricular depolarization to the opening of aorticvalve, is a marker of sympathetic activity. RSA, the variability of the heart rate duringthe typical respiratory cycle, is a marker of parasympathetic activity (i.e., cardiac vagaltone). Multivariable repeated measures linear regression models examined associationsbetween anxiety, depressive symptoms, and cardiac autonomic markers, adjustedfor age and body mass index. Results: Among the 121 participants[HA1] (mean age53 years old), no significant differences in mean anxiety or depression scores weredetected between the paced respiration and the music control groups at baseline or12 weeks. Resting cardiac autonomic parameters were similar at baseline and at 12weeks with no significant between-group differences. Greater trait anxiety and cognitiveanxiety were associated with lower RSA, reflecting decreased parasympathetic activity(β -0.03, p 0.01 for STAI Trait Anxiety; β -0.06, p 0.01 for HADS Anxiety Subscale).Greater depressive symptoms were also associated with lower RSA (β -0.03, p 0.02for BDI-II; β -0.06, p 0.02 for HADS Depression Subscale). Greater state anxiety wasassociated with shorter PEP, reflecting higher sympathetic activity (β -0.24, p 0.01),but no other significant associations between anxiety or depression and PEP weredetected. Conclusion: Among peri- and postmenopausal women with hot flashes, greaterself-reported anxiety and depression were associated with lower levels of cardiac vagaltone, while greater state anxiety was associated with higher resting sympathetic nervoussystem activation. Findings suggest that midlife women with increased anxiety anddepressive symptoms may have an unfavorable cardiac autonomic profile with potentialimplications for their overall cardiovascular risk.Sources of Funding: This study was funded by grant #5R01AT005491 from the NationalCenter for Complementary and Integrative Health. Dr. Huang was supported by a Paul B.Beeson Career Development Award in Aging Research from National Institute on Aging(1K23AG03833) and the American Federation on Aging Research. Dr. Gibson wassupported by an Advanced Fellowship in Women’s Health from the Veteran’s AffairsOffice of Academic Affiliations.S-8.Modifying Effect of ApoE4 Genotype on the Association BetweenMetabolic Phenotype and Subclinical Atherosclerosis in PostmenopausalWomenIntira Sriprasert, MD1,3, Wendy Mack, PhD1,2, Howard Hodis1,2, Roksana Karim, PhD1,2.1Preventive Medicine, Keck School of Medicine, University of Southern California,Los Angeles, CA; 2Atherosclerosis Research Unit, Keck School of Medicine, Universityof Southern California, Los Angeles, CA; 3Obstetrics and Gynecology, Faculty ofMedicine, Chiang Mai University, Chiang Mai, ThailandObjective: Both metabolic risk factors and presence of ApoE4 genotype are knownto have effects on coronary heart disease. We examined the interaction between thesetwo factors for their associations with subclinical atherosclerosis among early and latepostmenopausal women using baseline data from the Early versus Late InterventionTrial with Estradiol (ELITE). Design: Postmenopausal women from the ELITE trialwith available ApoE4 genotype were included in the analysis. Women were categorizedinto healthy, high blood pressure, and poor metabolic clusters based on the levels ofbaseline glucose, the HOMA insulin sensitivity score, ketones, triglycerides, high densitylipoprotein cholesterol, low density lipoprotein cholesterol, hemoglobin A1c, and systolicand diastolic blood pressure using k-means clustering analysis. ApoE4 genotype wasclassified as either ApoE4 (homo- or heterozygous for E4 allele) or ApoE4-. Generallinear models were used to test whether the cross-sectional association between metabolicclusters and baseline common carotid intima media thickness (CIMT) differed byApoE4 genotype after adjusting for age. A longitudinal analysis was also performedusing mixed effects analysis to evaluate the modifying role of ApoE4 genotype on theassociation between metabolic clusters and CIMT progression over a median followup of 4.8 years. Results: A total of 497 women with information on CIMT, ApoE4genotype (343 women with ApoE4 and 154 women with ApoE4-) and metaboliccluster (208 healthy, 190 high blood pressure and 99 poor metabolic) were includedin the analysis. In cross-sectional analysis among all women, ApoE4 women in thepoor metabolic cluster had the highest CIMT(SE) of 832.41(17.45) μm, compared toother groups of women. In the ApoE4- group, CIMT significantly differed betweenhealthy and high blood pressure clusters (p 0.004) and in the ApoE4 group, CIMTwas significantly higher in the poor metabolic cluster compared to healthy (p 0.0003)and high blood pressure (p 0.001) clusters. ApoE4 genotype significantly modified theeffect of metabolic cluster on CIMT (interaction p 0.001). In stratified analysis by early( 6 years) and late ( 10 years) postmenopause, the highest CIMT was consistently seen inApoE4 women in the poor metabolic cluster in both early and late postmenopause strata.Among late postmenopausal women, metabolic cluster was significantly associated withCIMT (p 0.04) and there was a significant synergistic effect of both factors on CIMT(interaction p 0.02), whereas the interaction was marginally significant among the earlymenopausal women (interaction p 0.05). These results were not observed on longitudinalanalysis of CIMT with a median follow up of 4.8 years. Conclusion: ApoE4 womenwith poor metabolic phenotype have higher levels of subclinical atherosclerosis,particularly when they are further from menopause. These results have significant clinicaland public health implications as preventive intervention strategies targeted to these highrisk women can substantially reduce the burden of coronary heart disease, which is theleading cause of death in women globally.Sources of Funding: NoneTable: CIMT by metabolic clusters and ApoE4 genotype among early and latepostmenopause stratumCIMT reported as μm; Model adjusted for age; Tukey-Kramer method as used totest for pairwise comparisons
S-9.Menstrual Cycle Length over the Menopause Transition is Associatedwith Subclinical Atherosclerosis after Menopause: The Study of Women’sHealth Across the Nation Daily Hormone StudySamar R. El Khoudary, PhD, MPH1, Xirun Chen1, Karen A. Matthews, PhD1,Amanda Allshouse2, Sybil Crawford3, Carol A. Derby5, Rebecca C. Thurston1,Rasa Kazlauskaite4, Nanette Santoro2. 1University of Pittsburgh, Pittsburg
Cleveland, OH; 3University of Florida College of Medicine-Jacksonville, Jacksonville, FL; 4TherapeuticsMD, Boca Raton, FL; 5EndoRheum Consultants, LLC, Malvern, PA Objective: TX-001HR (TherapeuticsMD, Boca Raton, FL), an investigational product that combines 17β-estradiol and progesterone (E2/P4) in a single, oral softgel capsule,