Transcription
Responding to Francis:clinical leadership
Nursing PracticeDiscussionWard sistersKeywords: Ward sister/Clinical leadership/Management skillsWard sisters need time to work in a supervisory capacity and provideclinical leadership; organisations need to ensure this can happenNT RESPONSEDeveloping skills in clinicalleadership for ward sistersIn this article. istorical development of the ward sister’s roleH Why nursing needs to modernise the role of the ward sister How ward sisters’ time can be freed up for clinical leadershipAuthors Katherine Fenton OBE is chiefnurse and professor of nursing leadershipat London City and London SouthbankUniversities and University College LondonHospitals Foundation Trust; NatashaPhillips is assistant chief nurse, UniversityCollege London Hospitals FoundationTrust, and PhD student, University ofHertfordshire, examining the ward sisterrole in the context of the acute NHS trust.Abstract Fenton K, Phillips N (2013)Developing skills in clinical leadership forward sisters. Nursing Times; 109; 9, 12-15.The Francis report has called for astrengthening of the ward sister’s role. Itrecommends that sisters should operate ina supervisory capacity and should not beoffice bound. Effective ward leadershiphas been recognised as being vital tohigh-quality patient care and experience,resource management andinterprofessional working.However, there is evidence that wardsisters are ill equipped to lead effectivelyand lack confidence in their ability to doso. University College London HospitalsFoundation Trust has recognised that thejob has become almost impossible inincreasingly large and complexorganisations. Ward sisters spend less than40% of their time on clinical leadershipand the trust is undertaking a number ofinitiatives to support them in this role.AlamyIn 1980, Sue Pembrey described theward sister as “the key nurse in negotiating the care of the patient becauseshe/he is the only person in the nursingstructure who actually and symbolicallyrepresents continuity of care to thepatient. She/he is the only person who hasdirect managerial responsibilities for boththe patients and nurses. It is the combination of continuity in a patient area togetherwith direct authority in relation to patientsand nurses that makes the role unique andso important to nursing” (Pembrey, 1980).While this quote is more than 30 yearsold, it remains as pertinent today as whenit was written. Ward sisters (also known ascharge nurses and ward managers) are theglue in the system, negotiating the boundaries of healthcare in increasingly complexhospitals. The ward sister is responsiblefor everything that happens on the ward24/7, but often has little or no control overmany of the staff who work on the ward orwith patients.The work of Pembrey and her peers inthe early 1980s demonstrated that ward sisters have a complex role with three parts:clinical expert; educator; and manager. Inreality, these elements are interrelated andinterdependent, as illustrated in Fig 1.Skilled leaders manage these overlaps,defining the boundaries and setting thepriorities. However, many struggle to balance the complexity and competingdemands of the role and this is reflected inresearch by the Royal College of Nursing(2009). This found that ward sisters areoften unclear about expectations of themand believe they lack the time, resourcesand authority to lead effectively. Nationaland international studies suggest wardleaders do not believe they have the powerto set priorities and are often merelyresponding to the demands of the system(Fealy et al, 2011; McNamara et al, 2011;Regan and Rodriguez, 2011; RCN, 2009;Gould, 2001; Aroian et al, 1996). This canlead them to focus on management tasks12 Nursing Times 05.03.13/ Vol 109 No 9 / www.nursingtimes.net5 keypoints1The ward sisterrole is vital forconsistent, highquality careLack of clinicalleadership is afactor in poor careThe Francisreport hascalled for astrengthening ofthe ward sister roleA criticalanalysisof healthcareorganisations anda whole-systemsapproach tochange is requiredto modernisethis roleThe role needsto be clearlydefined and sistersneed ongoingdevelopment2345The ward sister should work alongsidestaff as a role model and mentor
NursingTimes.netrather than providing clinical leadership.A number of high-profile cases, mostrecently Mid Staffordshire FoundationTrust (Francis, 2013), have demonstratedfailures to deliver safe and compassionatecare. These failures have contributed to alack of public confidence in healthcareproviders and particularly the nursingprofession. A lack of public faith innursing is evident in high-profile reportsby charities such as the Patients Association (2011), as well as the popular press.These concerns have led to calls toreview and strengthen the role of the wardsister (Department of Health, 2012; 2010;Nursing and Care Quality Forum, 2012;RCN, 2009). Arguably, this will help torestore public faith in both the professionand our hospitals. However, any suchefforts must not only include learningfrom these heartbreaking stories but alsofocus on the core values of nursing, takingthe best from our past and our present.The 6Cs strategy, recently launched bythe chief nursing officer (DH, 2012), seeksto do just this. It aims to reaffirm the corevalues of nursing and suggests these bedelivered through six action areas basedon initiatives such as Energise for Excellence (NHS Insititute for Innovation andImprovement, 2010) and the High ImpactActions (NHS III, 2009). The strategy callsall nurses to action to improve care, identifies the need to strengthen nurse leadership at all levels and proposes a valuesbased ward leaders’ programme.A historical perspectiveThe ward sister role has existed since theinception of modern nursing, underpinned by the Nightingale vocational tradition. It developed in a historically hierarchical nursing culture based on militaryand religious orders, where an autocraticapproach was valued and nursing wasbased on task allocation (Marquis andHuston, 2006; Moiden, 2002; Widerquist,2000). Key elements of the role were thedirect supervision of nursing staff andlearners, and the coordination of caredelivery (Bradshaw, 2010). Sister had directcontrol of the entire ward, including staffand resources. These authors suggest asurveillance role, an all-seeing figurerevered for her clinical excellence.Until the 1960s, the role of the ward sisterchanged little. However, the Salmon report(Ministry of Health and Scottish Homeand Health Departments, 1966) and thesubsequent Briggs report (1972) resulted ina restructuring of the NHS as a whole andnursing saw some direct managementresponsibilities devolved to others; thisFor articles on the Francis report,go to nursingtimes.net/francisFig 1. The ward sister roleClinicalexpertTeacherManagerClinical leadershipOrganisationreduced sisters’ direct authority. Responsibility for clinical standards remained keyto the ward sister role but evidence suggests the focus on management in theserestructures affected both organisationalunderstanding of the sister’s role and theability of sisters to maintain these clinicalstandards (RCN, 2009). Changes in titleadded to this role confusion and it could beargued that the disparity between the titleward sister and ward manager is notsimply terminology but concerns thevalues underpinning nursing. This hascontributed to the current nursing leadership crisis (Bradshaw, 2010).Essentially the role has always and continues to comprise three key elements:» Clinical nursing expert;francis on Ward sistersWard sisters and nurse managers shouldoperate in a supervisory capacity andshould not be office bound.They should: Know about the care plans relating toevery patient on their ward andshould be visible and accessible topatients and staff Work alongside staff as a role modeland mentor, developing clinicalcompetencies and leadership skillswithin the team Ensure that the caring cultureexpected of professional staff isconsistently maintained and upheld» Manager and leader of the ward staffteam and the ward environment;» Educator (of nursing and nurses, otherhealth professionals, patients andcarers).What has changed is the increasingcomplexity of the healthcare organisationsin which ward sisters operate. These complexities include an increasingly frail andolder patient population, a larger numberof professionals involved in patient care,multiple ward consultants, and multipleward rounds that often take place at thesame time. All these factors increase thechallenge of ensuring effective communication on the ward.Large and often far-removed corporateservices make it difficult to resolve day-today issues and necessitate multiple phonecalls and emails. High bed occupancy leadsto pressure to discharge patients and turntheir beds around rapidly for the nextpatient.The welcome focus on quality targetshas led to a move to understand the uniquecontribution of nursing to the quality ofcare (Griffiths, 2008). The development ofmeasures that identify, quantify and makevisible the impact of the nursing workforce on care quality outcomes increasesthe requirement for audits. This alsobrings additional work as the burden ofaudit and paperwork increases and manyreport difficulty in prioritising clinicalleadership (RCN, 2009).All these pressures, along with thedemands of managing a budget, wardresources and a large team of nursing staff,make the job almost impossible.www.nursingtimes.net / Vol 109 No 9 / Nursing Times 05.03.13 13
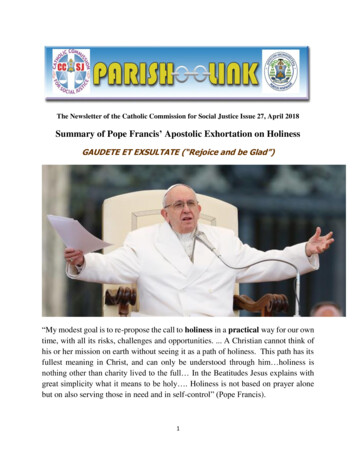
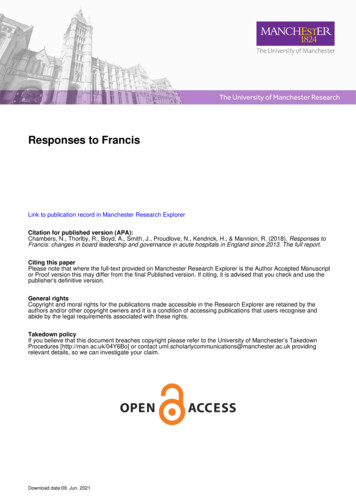
Nursing PracticeDiscussionRecently the complexities and challenges of the role have been recognised bythe profession and policy makers, whichhas led to calls to review and strengthenthe ward sister role. However, increasedpolitical pressure creates a danger ofrebranding without addressing a fundamental element to ward leadership –namely the organisation in which theleader operates.The culture of traditionally hierarchicaland bureaucratic organisations isenshrined in the structure of corporateservices and a surveillance culture thatdoes not make the demands of ward leadership easier. Evidence suggests that theway we structure our organisations has animpact on how effectively we can lead(Senge, 1990). Arguably, any efforts toenable sisters to lead must address thecomplexity of the system they work in. Awhole-systems approach to change isrequired, focusing on all elements of thesystem (Burke, 2011).Capacity to leadFlorence Nightingale said: “Let whoever isin charge keep this simple question in herhead how can I provide for the rightthing to be always done?”At UCLH we are asking this question collectively as an organisation. We are considering how to develop individual ward sisters, as well as looking at creatingorganisational strategy, values, systems andstructures that enable ward sisters to lead.Turnbull-James (2011) noted that “theNHS needs people who think of themselvesas leaders not because they are exceptionally senior or inspirational to others, butbecause they can see what needs doing andcan work with others to do it”. This resonates with and builds on Florence Nightingale’s quote of over 150 years ago.Ensuring the right thing can always bedone for patients is best achieved byworking collaboratively as an organisationto tackle the issues that constrain individual efforts to do the right thing. AtUCLH, this has led to a whole-systemsapproach to a number of projects thataddress the ward sisters’ capacity to lead,as well as the organisation’s ability toenable effective ward leadership.Liberating sisters to lead careIn 2009, the RCN called for ward sisters tobe supernumerary. These calls have beenechoed by many (Francis, 2013; DH, 2010).At UCLH, the term “supervisory to practice” is used. It is in being supervisory thatward sisters can clinically lead using theirskills as clinical experts and educators toFig 2. Ward sisters’ activity 2011With relatives4%Leadership,outsideclinical area7%Clinical care15%Leadership,in clinicalarea 21%Admin, patientrelated 4%Admin 35%Emails11%Admin,workforcerelated 11%,Meetings7%Admin, general2%Other4% Personal Projectdevelopment time4%6%Governance andsafety4%develop their teams and ensure excellencein care. We found our ward sisters werespending less than 40% of time in clinicalleadership, with 35% spent on administrative tasks. Fig 2 illustrates the breakdownof their daily activities; while many areessential to the ward sister role, such asbudget and staff management, they arenot streamlined to minimise the time awayfrom the bedside. Add in audit andreporting requirements and it becomesapparent that the role has become so vastthat it is impossible to dedicate the clinicalleadership time necessary to ensure consistency in patient care and experience.To redress the balance, organisationsneed to have all their elements aligned toreduce essential but time-consuming nonclinical workloads to free sisters to lead.This has been recognised by the HealthFoundation, whose Shared Purposeimprovement programme seeks to addressorganisational design, aligning corporateand clinical services around commonquality goals to improve patient experience (Health Foundation, 2013).We have designed and are undertakingone of these nine Shared Purpose projects,Liberating Sister to Lead. Its objective is toremove the burden of corporate processeson ward sisters, freeing them up to be visible leaders of their wards with a focus onimproving all elements of quality. A reviewof corporate services, such as humanresources and finance and estates, fromthe ward sisters’ perspective led to anobjective to increase clinical leadershiptime to 75% (Box 1). An example of this isthe introduction of a concierge service totake on many of the administrative tasks14 Nursing Times 05.03.13/ Vol 109 No 9 / www.nursingtimes.netthat take sisters away from the importantjob of leading patient care.Liberating Sister to Lead is a naturalprogression from the work on organisational values and behaviours we have beenundertakin
3The Francis report has called for a strengthening of the ward sister role 4A critical analysis of healthcare organisations and a whole-systems approach to change is required to modernise this role 5The role needs to be clearly defined and sisters need ongoing development . www.nursingtimes.net / Vol 109 No 9 / Nursing Times 05.03.13 13 » Manager and leader of the ward staff team and the ward .