Transcription
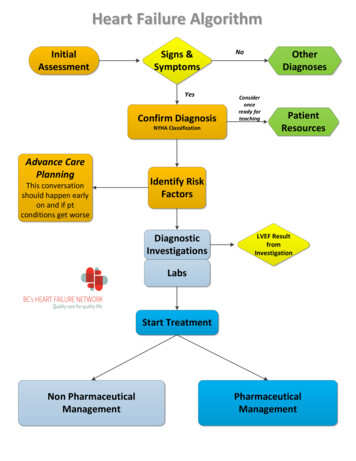
Heart Failure AlgorithmInitialAssessmentSigns &SymptomsYesConfirm DiagnosisNYHA ClassificationAdvance CarePlanningThis conversationshould happen earlyon and if ptconditions get worseNoOtherDiagnosesConsideronceready forteachingPatientResourcesIdentify RiskFactorsDiagnosticInvestigationsLVEF ResultfromInvestigationLabsStart TreatmentNon PharmaceuticalManagementPharmaceuticalManagement
Return to Page 1Print HandoutHeart Failure Patient QuestionnairePlease take the time to answer the following questions before you see your doctorAppointment Date:Since your last doctors appointment onYesNoHow many times?YesNoHow far in nDid you see a SpecialistIf yes: which specialistHave you been admitted to a hospital?Have you had to go to a hospital Emergency for treatment?What are you doing for activityFor howlong?How manytimes per weekWalkingHouseworkGardeningAnything elseAre you participating in a structured exercise program?How may pillows do you need to use to sleep?1234Worse567NoCommentsHas there been a change in your energy level since your lastappointment?Has there been an change in your shortness of breath since yourlast doctors appointment?Has your chest pain changed since your last visit?Do you ever feel your heart racing?Do you wake up at night with shortness of breath?Do you get lightheaded or dizzy?Do you have swelling in your: (circle) feet ankles legsstomachDo you take extra water pills for your swelling?SameCommentsSince your last doctors appointment do you feel your condition is?What fluid restriction do you follow?Over the last two weeks, how often have you been bothered byany of the following problems?Little interest or pleasure in doing thingsFeeling down, depressed or hopelessFeeling anxious, nervous or on edgeNot being able to stop or control worrying6‐8 cupsYes4‐6 cupsNoneOtherNoIf your patient answers “yes” to either question, go tothe PHQ9 questionnaireIf your patient answers “yes” to either question, go tothe GAD7 questionnaireQuestions you would like to ask your nurse or doctor today?Continued
Return to Page 1Print HandoutNameDateWeightVital SignsHeart SoundsLungsEdemaActivityPHYSICAL EXAMCurrentLast VisitB/PLyingStandingS1S2(circle)S3 1/4 1 2(circle) 3Type:O2 SatMurmursGradeS4Waist Circumference (cm)Murmur Location/RadiationAscites 1/2Fluid Volume(circle one) Euvolemic 4DryOverloadedTime/day: MinutesDays/wk : 1I(circle)HRJVP (cm)ClearCrackles(circle)NYHA ClassDry234IINo Sx567IIINo Sx at restIVComfortable only at restChest XRay:N/ASx at RestEF Date:(circle)EchoYesNoMIBIMUGADate:Clinical StatusBetterSameWorseStable:EDUCATIONTopic:YesMD (Directives and/or plan of mokingTravelStress ManagementType:Diuretic:ACE/ARB:Beta Blocker:Other:Medication:MEDICATIONSNotes/Changes:
Return to Page 1Signs and Symptoms of Heart FailureSignsSymptomsRed Flags Weight gain Fatigue Systolic BP 80(2 kg (4 lb) in two days or Dyspnea at rest Sa O2 , 92%2.5 kg (5 lb) in 1 week Decreased exercisetolerance Tachycardia 100 Swelling and/orAbdominal bloating Peripheral Edema Orthopnea New onset Cyanosis Oliguria Extra heart sounds Plural Effusion Elevated JVPApply O2Call 911 Ascites BNP measurement( may take up to 1 week) 20.00 100 not heartfailure 100‐400 equivocalfor Heart Failure 400 Heart failureAnd/orRefer to Acute careHospitalAnd /orConsult aCardiologist
Return to Page 1Non‐Heart Failure Causes of Shortness of BreathCardiac CausesPulmonary Causes: or other conditionsthat can mimic or exacerbate heart failureIschemic Heart Disease Myocardial infarction, ischemiaSupraventricular arrhythmias Atrial FibrillationHypertensionValvular heart disease Mitral regurgitation/stenosis,aortic insufficiency/stenosis,tricuspid regurgitation orpulmonic insufficiencyAsthmaSleep ApneaChronic Obstructive Pulmonary DiseasePneumoniaInterstitial Pulmonary DiseaseRestrictive lung disease due to abdominalobesityPulmonary EmbolismRenal InsufficiencyCollagen vascular diseaseEndocrinologic or metabolic disorders Hyperthyroidism, hypothyroidism,uremia, diabetes mellitus,acromegaly, thiamine deficiency,selenium deficiency, carnitinedeficiency, kwashiorkor, carcinoidPregnancyFebrile illnessesAnemia
Return to Page 1New York Heart Association Functional ClassFunctional ClassI (mild)II (mild)III (moderate)IV (severe)SymptomsNone Can perform ordinary activities without anylimitationsNo symptoms at rest Occasional swelling Somewhat limited in ability to exercise or do otherstrenuous activitiesComfortable only at rest Noticeable limitations in ability to exercise orparticipate in mildly strenuous activitiesSymptoms at rest Unable to do any physical activity without discomfortHeart failure is classified on a scale of I‐IV based on the patients symptoms and abilityto do activity or exercise. The functional class can get better or worse over time basedon how the patient responds to treatment and how severe their symptoms are.Treatment for patient’s heart failure is based on their functional class.Adapted from: The Criteria Committee of the New York Heart Association. Nomenclature and Criteria for Diagnosis ofDiseases of the Heart and Great Vessels. 9th ed. Boston, Mass: Little, Brown & Co; 1994:253‐256
Return to Page 1Risk FactorsCoronary artery diseaseHypertensionDiabetes MellitusAlcohol or substance abuseFamily historyAtrial fibrillationToxic exposure: includingo Chemotherapyo RadiationThyroid disease and other endocrinopathiesConditions that may worsen heart failureChronic obstructive pulmonary diseaseKidney diseaseModerate to severe sleep apneaAnemiaHypertension
Return to Page 1Advance care planningDiscussion initiated early in the disease course and particularly when symptomsand/or functional status declines despite maximal medical therapy. Discussion about natural history of the disease and prognosis in all cases Address all precipitating factors: angina, hypertension, sodium and fluidrestriction, adherence to medications, contributory conditions Ensure all active therapeutic options have been appropriately considered (ICD,biventricular pacing, revascularization, transplant)Once the decision to initiate end‐of‐life care is made, the goal of therapy is to manageall symptoms (including those of comorbid conditions, e.g. chronic pain) and addressfunction and quality of life issues.Subsequent care should be based on the following principleso Support of dying patients and their familieso Control of pain and symptoms ( eg. overload) Consider choice and dose of narcotic as renal function is likely impaired –i.e. Hydromorphone for narcotic naïve, Duragesic patch. Consider narcotic use with uncontrolled angina, or as a first‐line fordyspnea Consider home oxygen (See COPD Guideline for indicationshttp://www.bcguidelines.ca/guideline copd.html) Adequate diuretic use (sometimes more than one agent) is important ACE‐I dose may need to be reduced if limited by symptomatic hypotensionand renal impairment (Cr 250 μmol/L or 30% from baseline)o Decisions on the use of life‐sustaining therapies
Return to Page 1Heart Failure Diagnostic TestsAssessment of Left Ventricular Function(Should be within 4 weeks of Heart Failure diagnosis)2D Echocardiogram – allows assessment of left ventricularfunction as well as other cardiac structures(repeat at end of treatment)ORMUGA – most accurate assessment ‐ Left Ventricular Function consider in patients with Atrial Fibrillation or who areoverweightORPerfusion Imaging (eg MIBI Scan) – provides information aboutboth ischemia and Left Ventricular function
Return to Page 1Other Heart Failure Diagnostic and Lab TestsChest XRayECGLab:Electrolytes, BUN, creatinine and eGFRTSH, FBS, CBC, INRLiver Enzymes (AST, ALT, Gamma GT)Consider Cholesterol, NT‐proBNP or BNP
Return to Page 1Non pharmacologicalHeart Failure 101 PatientInformation HandoutMultidisciplinary HF care including specialized HFclinics where availablePatient Education with focus on HF self managemento DietLow Low sodium diet (less than 2000mg perSodiumday) Fluid Restriction 6‐8 glasses/day (1500‐Fluid2000ml or 48‐64 oz per day: IF on a diureticRestrictionsuch as Furosemide)o Activity (if stable HF, attempt regular aerobicActivityand anaerobic activity OR consider referring toa cardiac rehabilitation program)Smokingo Smoking cessation counseling or referral toCessationsmoking cessation program where availableo Daily weightsDaily Wt Weight gainChart(No more that 4 lbs (2 kg) in 2 days or 5 lbs (2.5 kg) in one weekImmunizationsCounseling for alcohol abstinence and substance abuseAlcohol & SubstanceAbuse CounselingSnap Shot of Your VisitPatient FormREFER TO HEART FAILURE ZONES FORMAlso on BC Heart Failure Website: www.bcheartfailure.caHeart Failure ZonesPatient Handout
To Non PharmeceuticalPrint HandoutReturn to Page 1Page 1 of 4Understanding Heart FailureThe BasicsHow does the heart work?What is Heart Failure?Your heart is a muscleabout the size of yourfist. It works like apump, pumping bloodand nutrients aroundyour body.Heart failure is when your heart is notpumping as strongly as it should. Your bodydoes not get the right amount of blood,oxygen, and nutrients it needs to workproperly.The heart is actually a2-sided pump. The rightside of the heart pumps‘used’ blood from thebody to the lungs. In the lungs, your blood isloaded up with oxygen. The left side of the heartpumps ‘fresh’ blood full of oxygen from thelungs to the rest of the body. The left side ofthe heart is usually the larger than the right.That is because it has to pump hard to get theblood out to all parts of your body.Each side of the heart has 2 chambers. Valveslink the chambers and keep blood pumping inthe right direction. These valves open and closewith each heartbeat.Heart failure usually gets worse over time.While heart failure cannot be cured, people dolearn to live active, healthy lives by managingtheir heart failure with medication, changes intheir diet, weighing daily and physical activity.There are two main types of heart failure: A weak pump: When the heart muscle isweak, it gets larger and ‘floppy’. A stiff pump: When the heart musclecannot relax between beats because themuscle has become stiff. The heart cannotproperly fill with blood between beats.Both types of heart failure reduce theblood flow and oxygen to your body.Draft #10 March 13-12. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.
Return to Page 1To Non PharmeceuticalPage 2 of 4What causes Heart Failure?Heart failure has many causes including: Heart attack High blood pressure Heart valve problems Heart defects at birth Lung conditions Excessive use of alcohol or drugsOther possible causes of heart failure include: Obesity Sleep apnea Infections affecting the heart muscle Abnormal heart rhythm Severe anemia Severe kidney disease Overactive thyroid gland Exposure to chemotherapy or radiationNot sure what caused your heart failure? Askyour doctor or nurse practitioner.Signs of Heart FailureYou may notice any of the following signs.You feel short of breathwhen you do daily activities.You find it harder to breathewhen resting or lying down.You wake up at nightfeeling short of breath.You find it easier to sleep by addingpillows or by sitting up in achair.You cough often, especiallywhen lying down.Your cough is either dry and hacking, ormoist and you cough up mucus (whichcould be slightly pink).You feel your heart beat faster and it doesnot slow down when you rest.You feel your heart racing, jumping, orpounding in your chest.You cannot walk as far you normally can.You are tired all the time and have noenergy to do daily activities.You feel lightheaded ordizzy, especially when youstand up or increase youractivity and this is new foryou.You cannot eat as much asyou normally would.You are not hungry and donot feel like eating.You feel bloated or yourclothes feel tighter than normal.You have swelling in yourfeet, ankles, legs, or even upinto the belly (abdomen).Sudden increase in bodyweight where you gainmore than 4 pounds (2kilos) in 2 days.You feel uneasy, like something does notfeel right.You feel confused and have troublethinking clearly (and this is new for you).Draft #10 March 13-12. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.
Return to Page 1To Non PharmeceuticalPage 3 of 4Tests to identify heart failureHow is heart failure treated?There is no single test for heart failure. Insteadyour doctor does a number of tests. The doctorlooks at all the test results to determine if youhave heart failure.Look in the mirror - the key totreatment is you.Tests can include: Blood tests to check certain enzymes Chest x-ray to look at the size of your heart Electrocardiogram (or ECG) to look at theelectrical activity of the heart Exercise stress test to look at how yourheart responds to exercise Nuclear medicine scan to get a close lookat the pumping of your heart Angiogram to look for blockage in yourheart arteries Echocardiogram or ultra sound of theheart to look at the movements of yourheart and measure your ejection fractionMore about Ejection FractionThis test is usually done during anechocardiogram or a nuclear medicine scan.Your ejection fraction can go up and down,depending on your heart condition and howwell the treatment is working. It is good toknow what your ejection fraction reading is.The reading is given as a percentage withnormal being between 55 and 70%. Less than55% means your heart is not pumping asstrongly as it should be. Your ejection fractionhelps your doctor or nurse treat your heartfailure.Your doctor relies on you to make changesin your lifestyle and eating habits. Whilethere is a team of health care providersworking with you to manage your heartfailure, you are the one in charge.Treatment is focused on helping you live alonger and healthier life. This includes: Monitoring your symptoms Reducing salt in your diet Increasing your daily activity throughregular exercise Keeping your blood pressure low Maintaining a healthy weight Stopping unhealthy habits such assmoking Taking your medications as prescribedFor some people, surgery and medical devicesare needed to treat the problem that led to theheart failure. Treatments could include: Coronary bypass surgery Valve repair or replacement surgery Implanted device such as a pacemakerand/or defibrillator Mechanical device to help the heart pump Heart transplantFor novel new ideas on heart failure treatmentconsult your health care provider.Draft #10 March 13-12. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.
Return to Page 1To Non PharmeceuticalPage 4 of 4Plan today for the futureWhy learn to manage your heart failure?Your heart failure may get worse over time.Start thinking now about how you wish to becared for if your disease progresses. This iscalled ‘advanced care planning’. Advance careplanning allows you to have a say in yourhealth care if you are unable to speak foryourself.When you take charge of your health and learnto manage your heart failure, it helps you:Talk to your family and your doctor abouthelping you live well with heart failure andabout the care you do or do not want in thefuture.Things to think about and consider:What does it mean to live well with heartfailure?What is important to you to make your lifethe best it can be?What is important to you as your conditionprogresses?Improve the quality of your life.Feel confident that you can manage yourheart failure.Control your condition so it will not controlyou.Know when to ask for help from your careteam.Limit the need to go to the hospital for care.Prevent or limit heart failure complicationsas the disease progresses.Talk with your family and your care teamabout your disease and care plan.People who learn to manage their heart failureare more likely to live a longer, healthier lifethan those who do not.For more information on heart failureWhat worries and concerns do you have?How will your progressing heart failureaffect you and your family?BC’s Heart Failure Networkwww.bcheartfailure.caWho or what gives you support when youneed it?Interior Health Authority Heart FailureOnline ilies/e-learning-module-on-hf/If you are not able to make your own healthcare decisions, who will you want to makethem for you? Does that person know whatyou want?Do you have written instructions for howyou want to be cared for if you cannotmake decisions for yourself (this is calledan advance directive).HealthLinkBC on Heart 415.html#tp17534Canadian Cardiovascular Societywww.ccs.caCanadian Heart Failure Networkwww.chfn.caHeart Failure Society of Americawww.hfsa.orgDraft #10 March 13-12. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.
To Non PharmeceuticalPrint HandoutReturn to Page 1Heart Failure Zones Weigh yourself in the morning before breakfast. Write it down.CheckWeightDaily Compare your weight today to your weight yesterday.Keep the total amount of fluids you drink to only 6 to 8 glasses each day.(6‐8 glasses equals 1500‐2000 mL or 48‐64 oz)Take your medicine exactly how your doctor said.Check for swelling in your feet, ankles, legs, and stomach.Eat foods that are low in salt or salt‐free.Balance activity and rest periods.Which Heart Failure Zone Are You Today? Green, Yellow, or RedALL CLEAR – This zone is your goal!SafeZoneYour symptoms are under control.You have: No weight gain of more than 4 lbs (2 kg) in 2 days. No shortness of breath. No swelling or increase in swelling of your feet, ankles, legs, or stomach. No chest discomfort, pressure, or pain.CAUTION – This zone is a warningCautionZoneCall your doctor’s office if you have any of the following: You gain more than 4 lbs (2 kg) in 2 days. You feel more short of breath than usual. You have increased swelling in your feet, ankles, legs, or stomach. You have a dry hacky cough. You feel more tired and don’t have the energy to do daily activities. You feel lightheaded or dizzy, and this is new for you. You feel uneasy, like something does not feel right. You find it harder for you to breathe when you are lying down. You find it easier to sleep by adding pillows or sitting up in a chair.Doctor’s NameOffice Phone NumberEMERGENCY – This zone means act fastDangerZoneGo to emergency room or call 9‐1‐1 if you have any of the following: You are struggling to breathe. Your shortness of breath does not go away while sitting still. You have a fast heartbeat that does not slow down whenyou rest. You have chest pain that does not go away with rest orwith medicine. You are having trouble thinking clearly or are feeling confused.Updated: January 2012. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.
To Non PharmeceuticalPrint HandoutReturn to Page 1Limiting Sodium (Salt)When You Have Heart FailureSodium is a mineral found in food, table salt,and sea salt. Your body needs some sodium,but too much sodium causes your body to holdon to (or retain) fluid. This fluid build‐upmakes your heart work harder. The fluidbuild‐up can cause swelling in your feet, legs,or belly. Fluid can also build up in your lungs,making it hard for you to breathe.If your weight increases by more than 2 kg(4 lb) in two days, or 2.5 kg (5 lb) in 1 week,you are retaining fluid. If this happens, youshould call your health care provider rightaway.You should restrict the amount of sodium youeat to 2000mg or less each day.In the average Canadian diet, where doessodium come from? In ready‐made processedfoods and restaurantmeals (77%) Naturally occurring infood (12%)11%12%77% Added to food in cookingand at the table (11%)Remove the salt shaker fromthe table. Don’t add salt,flavoured salts or seasoningshigh in salt to your foods.One teaspoon of salt contains2300mg of sodium!Season your food with herbs, spices, lemonjuice, dry mustard, and garlic. Try one ofthe many seasoning blends which containno salt such as Mrs. Dash.Stay away from eating: processed foods deli meats pickled foods salted snack foods such as potato chips,pretzels, dips, and salted nutsLimit the amount of canned foods you eat.Choose products labelled ‘low sodium’.Foods labelled ‘lower’, ‘less’ or ‘reduced insalt or sodium’ may still be high in sodium(including soups and meats).Eat out less often. Ask restaurants to provide informationon low sodium choices. Restaurant meals and fast foods arealways higher in salt than home cookedlow sodium meals. For more info, please refer to LowSodium (Salt) Eating Out fact sheet atwww.healthlinkbc.ca (or click here).How to avoid salt (sodium)?Eat fresh foods most of the time andprepare home‐cooked, low sodium meals.Frozen foods are acceptable if they do nothave added salt or sodium additives (whichare used as preservatives).XUpdated: January 2012. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.1Continued
Return to Page 1To Non PharmeceuticalCan I use Salt Substitutes?Some salt substitutes use potassium instead of sodium. Check with your doctor or dietitian beforeusing a salt substitute because some people need to limit how much potassium they have each day.Keep your sodium intake to less than 2000mg each day.As you gradually reduce the amount of salt you are eating, your taste buds will adjust!How do I know how much sodium is in food?Nutrition FactsHere are some helpful tips when reading the nutrition label:Serving Size: Per ½ cup (125ml)Look at the serving size – the amount of sodium listed isper serving (not the whole package).AmountCalories 140Keep track of the total amount of sodium you eat.Remember: Your maximum recommended dailyamount of sodium is no more than 2000mg per day fromall sources.Keep the sodium content of each meal below 650mg –this helps spread out your sodium intake over the daypreventing excessive thirst and/or fluid retention.By law, foods labelled ‘low sodium’ must contain 140mgor less per serving.Other ingredients high in sodium include: baking soda,brine, monosodium glutamate (MSG), soy sauce, fish sauce,garlic salt, celery salt, or any ingredient with ‘sodium’ aspart of its name.% Daily ValueTotal Fat 0.5g1%Saturated Fat 0.2g1% Trans Fat 0gCholesterol 0mg0%Sodium 390mg16%Total Carbohydrate 28g9%Dietary Fibre 5g20%Sugars 9gProtein 7gVitamin A2%Vitamin CCalcium8%Iron0%15%Look what happens to the sodium content of foods when they are processedUnprocessedProcessedCucumber7 slices 2mgDill pickle1 medium 569mgChicken Breast3oz 74mgChicken Pie1 serving frozen 889mgTomato1 small 14mgTomato Soup1 cup 960mgPork Tenderloin3 oz 58mgHam3oz 1095mgUpdated: January 2012. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.2
To Non PharmeceuticalReturn to Page 1Print HandoutDaily Weight InformationPatient Name:Heart Function Clinic or Physician’s office:Health Care Provider:Contact phone number:Check Your Weight Every DayWhy:Checking your weight every day lets you know if your body is retaining fluid.Excess fluid build up in your body makes your heart work harder.When you report weight gain early to your health care provider, they can help you prevent your heartfailure from getting worse. This can help prevent a hospital admission.If your weight increases by: More than 2 kg (4 lb) in two days, orYou are retaining fluid. More than 2.5 kg (5 lb) in 1 weekYou should call your health care provider.For further directions, please refer to ‘Heart Failure Zones’ information sheet.When:Same time every dayPreferably before breakfastHow:After you have emptied your bladder (gone ʹpeeʹ)Wear the same amount of clothingRecord your weight in the attached calendar.(or You may prefer to use your own method such as a notebook, a computer.)Remember to bring your record to your doctor or clinic appointment.Updated: January 2012. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.1Continued
To Non PharmeceuticalReturn to Page 1Your ‘Dry Weight’ (when you don’t have excess fluid in your body):Write down your weight each day compare today’s weight to yesterdays weight.If your weight increases by: More than 2 kg (4 lb) in two days, orYou are retaining fluid. More than 2.5 kg (5 lb) in 1 weekYou should call your health care FridayUpdated: January 2012. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.Saturday2
To Non PharmeceuticalPrint HandoutReturn to Page 1Limiting FluidWhen You Have Heart FailureWhat is a fluid?Any food or drink that is liquid at roomtemperature. This includes water, ice, milk,juices, soft drinks, hot drinks, alcohol, soups,gelatin desserts, ice cream, popsicles, andliquid nutrition supplements (such as Ensureor Boost).Why do you have to limit fluid?When you have heart failure, fluid can buildup causing swelling in your feet, legs or bellymaking your heart work harder. Fluid can alsobuild up in your lungs, which may cause youto have trouble breathing.How much fluid can you have in a day?You should have no more than 1.5 to 2 litres offluid in a day. You may find you are thirsty tobegin with. As you gradually reduce your fluidintake, your body will adjust!How do you know when you have too muchfluid?To keep track of whether your body is holdingon to too much fluid, weigh yourself daily.Here is how to weigh yourself:Weigh yourself at the same timeevery day. The best time is firstthing in the morning.Weigh yourself after emptyingyour bladder (gone pee).Wear the same amount of clothingeach time.You are holding on to too much fluid when:or Your weight Your weightincreases by moreincreases bythan 2 kg or 4 lbmore than 2.5 kgin two days.or 5 lb in a week.Contact your health care provider right away ifyou are holding too much fluid.Guide to Fluid Measures2 tablespoons 30 ml 1 ounce1 glass 250 ml 8 ounce1 pint 16 ounce500ml1 litre or 1 quart 1000 ml 32 ounce2 litres 2000 ml 64 ounceTotal amount of fluid per day1.5‐2 litres 48‐64 ounces 6‐8 glassesTips for reducing your fluid intakeUse smaller cups and glasses.Measure the amount of fluid your mugsand glasses hold. They may measure morethan 250 ml or 8 ounces!Sip your fluids slowly.Write down the amount you drink each dayuntil limiting your fluid becomes a habit.(More tips on page 2.)Updated: January 2012. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.1Continued
Return to Page 1To Non PharmeceuticalMore tips for reducing your fluid intakeSip your fluids throughout the day.Keeping track of fluids is the only way tolearn how to make the 1.5 to 2 litres of fluidlast you through the day.You may find it easier to use areusable water bottle. Measurehow much the bottle holds so youknow exactly how much wateryou are drinking.Drain the fluid from canned fruit.Be aware of foods with high water contentlike watermelon, yogurt, and pudding.Limit the amount of sodium you eatto 2000mg or less each day. Salt willmake you thirsty. For moreinformation, refer to the handoutLimiting salt (sodium) when you haveheart failure.Try not to eat sweet foods. They can makeyou thirsty. If you have diabetes,controlling your blood sugar also helpscontrol your thirst.XTry not to drink alcohol. Alcoholdehydrates your body and makes youthirsty.If you can, swallow your pills with softfood like yogurt or porridge.Tips to deal with thirstRinse your mouth with water often, but donot swallow.Suck on a lemon wedge, lemon candy,or sour candy.Brush your teeth often.Use lip balm to keep your lips fromdrying out.Use a mouth wash. However, do not use amouth wash that contains alcohol. Theytend to dry out your mouth.Snack on a small piece of cold or frozenfruit such as a frozen grape or cold orangeslice. Try cold crisp vegetables too.Don’t overheat your home. Considerusing a humidifier to increase themoisture in the air.Ask your pharmacist about gels or spraysthat can add moisture to your mouth.Chew sugar‐free gum.For more tips and resources for limiting fluid, call HealthLink BC (dial 8‐1‐1) to speak to a healthcare professional. You can also refer to www.healthlinkbc.ca (or click here).Updated: January 2012. For more information on heart failure, go to www.bcheartfailure.ca.The information in this document is intended solely for the person to whom it was given by the healthcare team.2
To Non PharmeceuticalPrint HandoutReturn to Page 1Why People with Heart Failure Should Keep ‘Active’What does it mean to be ‘active’?Is the activity level right for me?Activity and exercise ‐ People often use thesetwo terms to mean the same thing. All physicalactivities and exercise do involve increasingthe heart rate and strengthening muscles.Get to know your body. It isimportant that you fe
Heart failure usually gets worse over time. While heart failure cannot be cured, people do learn to live active, healthy lives by managing their heart failure with medication, changes in their diet, weighing daily and physical activity. There are two main types of heart failure: A weak pump: When the heart muscle is