Transcription
Heart failure
Heart failure Heart Failure is the inability of the heart to pumpsufficient blood to meet the needs of the tissuesfor oxygen and nutrients. It is otherwise known as Congestive CardiacFailure. Heart failure results in intravascular andinterstitial volume overload and poor tissueperfusion.
causes Reduced ventricular contractility Ventricular outflow obstruction (pressureoverload ) Ventricular inflow obstruction Ventricular volume overload Arrhythmia Diastolic dysfunction
Acute causes Acute myocardial infarctionDysrrhythmiasPulmonary emboliThyrotoxicosisHypertensive crisisRupture of papillary muscle( eg: mitral valve)Ventricular septal defectMyocarditis
Chronic causes Coronary artery diseaseHypertensionRheumatic heart diseaseCongenital heart diseaseCor pulmonaleCardiomyopathyAnemiaBacterial endocarditisValvular disorders
RISK FACTORS Advancing ageHypertensionDiabetesObesityHigh serum cholesterolCigarette smoking
PRECIPITATING CAUSES AnemiaInfectionHypothyroidismBacterial endocarditisPaget’s diseaseNutritional deficienciesHypervolemia
PATHO PHYSIOLOGYCompensatory mechanism 1. Hemodynamic alterations2. Neurohormonal responses3. Ventricular dilation4. Ventricular hypertrophy
Alterations in Beta-adrenergic Receptor pathway Increased NE concentration cause down regulation ofbeta-1 adrenergic receptors in the ventricles. Beta- adrenergic receptor kinase(BARK) enzyme levelincreases.
Role of Arginine Vasopressin (AVP) Circulating AVP is elevated. This leads to salt and waterretention and systemic vasoconstriction.
Role of cytokinine They have crucial roles in mediating thechanges in myocardial structure and functionin CHF.
Cellular and Molecular Mechanisms Role of calcium Calcium plays a central role in myocardialcontraction and relaxation. In CHF, there isprolonged elevation of intracellular calciumduring relaxation
Role of free radicals and apoptosis Altered mitochondrial oxygen metabolismresults in formation of free radicals. Free radicals produced by various mechanismshave been shown to result in apoptosis ofcardiac myocytes in CHF.
DECOMPENSATED HEART FAILURE Ventricular remodeling Sustained neurohumoral activation
Counter regulatory mechanism ANP and BNP are hormones produced by the heartmuscle . ANP is released in response to stretch or increasedvolume in the chambers. Levels of circulating ANP can be correlate withfunctional class prognosis and hemodynamic state.
Inhibit renin, aldosterone and ADH secretion and resultsin excretion of sodium and water Promotes venous and arterial vasodilatation. BNP is released in response to an increase in wall stressor triggered by pressure.
TYPES OF HEART FAILURE Left –sided heart failure or left ventriculardysfunction Right sided heart failure or rightventricular failure Biventricular heart failure Diastolic and systolic dysfunction
High output versus low output failureHigh output failure occurs when the heart despitenormal output to high output levels is simplynot able to meet the accelerated needs of thetissuesLow output failure occurs in most forms of heartdisease resulting in hypoperfusion of tissuecells .
Backward versus forward failure Backward failure focuses on the ventriclesinability to eject completely ,which increasesventricular filling pressures ,causing venousand pulmonary congestion . Forward failure is a problem of inadequateperfusion. It results when reduced contractilityproduces a decrease in stroke volume andcardiac output
Acute versus chronic heart failure
CLINICAL MANIFESTATIONS Left Sided HeartFailure Acute LVF presents with a sudden onset ofdyspnoea at rest. progresses to acute respiratory distress,orthopnoea and prostration. appears agitated ,pale and clammy Rapid pulse
Cool peripheryHigh BPElevated JVP if associated with RVF.Auscultaition – crepitations,triple gallop rhythm.Displaced apex beat.
Respiratory system TachypneaCapillary refill 3 secondsOrthopneaDyspnea on exertionNocturnal dyspneaCough with frothy sputum (indicative ofpulmonary edema)
Basilar crackles or rhonchiCyanosisHypoxia (respiratory acidosis)Kussmaul’s signCheyne stokes respiration
Cardiovascular system Diaphoresis Audible S3 and S4 heart tones Murmur or mitral insufficiency Enlarged left ventricle on X-ray Enlarged left atrium on X-ray Narrowing pulse pressure Pulses alternans (alteration of weak and strongbeats)
Basilar crackles or rhonchiCyanosisHypoxia (respiratory acidosis)Kussmaul’s signCheyne stokes respirationElevated pulmonary artery pressuresElevate pulmonary artery occlusive pressures
Central nervous system Mental confusionGeneralized symptoms Weight gain. Fatigue/weakness/lethargy
Right sided heartfailureGastro intestinal system Hepatomegaly Splenomegaly Hepatojugular reflux Ascites
Weight gain Weight loss and emaciation as a result of inadequateintake of food and wasting of tissues. This picture istermed as cardiac cachexia
Cardiovascular system ArrhythmiasElevated CVPElevated right atrial pressureElevated right ventricular pressureNarrowing pulse pressureMurmur or tricuspid insufficiency
Audible S3 and S4 heart tonesEnlarged right atrium on X-rayEnlarged right ventricle on X-rayDependant pitting edemaVenous distention
Urinary system Oliguria Nocturia
Chronic heart failure FatigueDyspneaOrthopneaParoxysmal nocturnal dyspneaTachycardiaEdema
Nocturia Skin changesChronic swelling result in pigment changescausing the skin to appear brown cool and damp to the touch Behavioral changes Chest pain Weight changes
COMPLICATIONS Pleural effusion DysrhythmiasEF less than 35%have a high risk of fataldysrhythmias and sudden cardiac death. Renal failure Impaired liver function & Cardiac cirrhosis ThromboembolismHypokalemia & Hyperkalemia
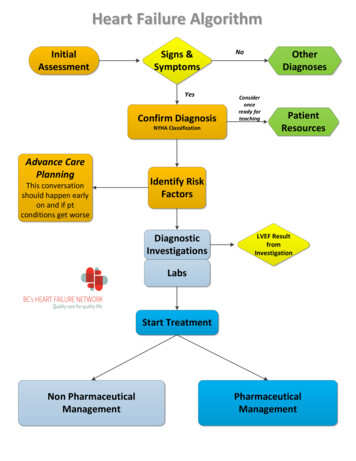
DIAGNOSTIC STUDIES History Physical Examination
Electrocardiogram Laboratory data(cardiac enzymes, BNP,serum chemistries,liver function studies ,thyroid function studies andcomplete blood count). In severe CHF dilutionalhyponatremia occurs. BUN and creatinine are moderatelyelevated.
BNP levels are used to assess the HF. BNP 100pg/ml- heart failure veryimprobable BNP100-500pg/ml-HF probable BNP 500pg/ml-HF very probabl
Echocardiogram : EF less than 40% accepted as evidenceof systolic dysfunction. Asessment of myocardial viabilityThis can be done by using dobutamine or dipyridamolestress echocardiography, nuclear imaging using thalliumor sestamibi and positron emission tomography
Identify patients who will benefit from long term therapywith drugs such as ACE inhibitors Stress testing,(treadmill test, stress echocardiography andnuclear perfusion studies) Cardiac catheterization and coronary angiography:
Endomyocardial biopsyThis is indicated in patients with clinical indication ofmyocarditis and systemic disease with possible cardiacinvolvement such as hemochromatosis, amyloidosis,sarcoidosis and those who have received adriamycinchemotherapy.
MANAGEMENT OF ACUTE PULMONARY EDEMA Sit the patient up Give oxygen(high flow ,high concentration ).non invasive positive pressure ventilation(CPAP-5-10 mmhg) IV glceryl trinitrate 10-200 microgram/minute until clinical improvement occurs orsystolic blood pressure falls to 110mmHg. loop diuretic such as frusemide 50-100mg IV
continuous monitoring Ionotropic agents Intra aortic balloon pump
Management General measuresPharmacologic therapyDevicesSurgeryNewer evolving therapies
General measures Rest Correction of aggravating factors Salt restriction – sodium intake should belimited to 2g/day Fluid restriction- to 1-2l/day is advisable inpatients with dilutional hyponatremia. Smoking cessation Avoid alcohol Management of co morbidities
Pharmacologic therapyTo Reduce workload Angiotensin converting enzyme inhibitors Angiotensin II receptor blockers Vasodilators Diuretics Beta blockers
ACE inhibitors Interrupts the vicious cycle of neurohumoral activation Prevents salt and water retension ,peripheral arterial andvenous vasoconstriction Also increase the concentrations of the vasodilatorbradykinin. Decreases SVR and improves myocardial performance.
Enalapril: 2.5 mg 12 hrlyLisinopril 2.5 mg dailyRamipril :1.25 mg dailyCaptopril :50 mg tds
Adverse effects Persistant coughHypotensionHyperkalemia\deteriorating renal functionLoss of taste
Angiiotensin II receptor blockers Similar hemodynamic effects to ACE inhibitorsDo not affect bradykinin metabolismLosartan, Valsartan, Irbesartan and EprosartanLosartan :25 mg dailyCandesartan:4 mg dailyValsartan : 40 mg daily
Vasodialators Venous dialationblood is trapped in theveins ,and venous return to the heart isdecreased .This reduces preload eg: nitroglycerin and isosorbide dinitrate Dilation of arterioles: arteriolar vasodilatorsdecreases peripheral vascular resistance andafterload Eg:ACE inhibitors
Combined action on veins and arterioles decrease both preload and afterload sodium nitroprusside relaxes the smooth muscle of bothveins and arterioles.it does not directly affect the heartmuscle or heart rate
Beta blockers Directly block the direct effects of the SNS Cardio selective agents block beta 1 adrenergicreceptors.non selective agents block beta 1 and beta 2adrenergic receptors. Eg: atenolol,metoprolol , bisoprolol, bucindolol,labetalol,carvedilol,esmolol (25-50 mg bd)
Diuretics To mobilize edematous fluid , reduce pulmonary venouspressure ,and reduce preload Thiazide diuretics may be the first choice in chronic HF lazone
Loop diuretics eg.Frusimide ,torsemide Spironolactone is an inexpensive ,potassium sparingdiuretic.
Human b-type natriuretic peptideNesiritide is a synthetic form of human BN
Beta adrenergic agonists short term treatment E.g.:-dopamine, dobutamine
Cardiac glycosides Eg ; Digoxin Slow the ventricular rate, improves cardiac function Optimum therapeutic level os digoxin in serum is 1-1.5ng/ml Toxic level is above 2ng/ml
Calcium channel blockers Vasodilator Anti ischemic effects Eg: Verapamil, diltiazem, amlodipine
Phosphodiesterase inhibitors:Eg: amrinone,milrinone Antidysrhythmic drugse.g.adenosine, digoxin, ibutilide, magnesium
Devices Implantable cardiac defibrillators andresynchronization therapy
Ventricular assist devices
Extracorporeal membrane oxygenator
Surgery Heart transplantationCoronary revascularizationDynamic cardiomyoplastyPartial left ventriculectomy( Batista procedure)AneurysmectomyMitral annuloplasty and mitral valve repair
Newer evolving therapies Gene therapy To increase the myocardial contractility at molecularlevel Genes expressing SERCA2a are increased by usingadenovirus transfection of myocytes
NURSING ASSESSMENT
Nursing diagnosisDecreased cardiac output r/t heart failure,dysrhythmia or both Assess blood pressure for hypotension orhypertension Assess heart rate and rhythm Document rhythm strips q8h Auscultate heart rate q2h Monitor lung sounds
Monitor intake and outputAssess for change in mental statusAdminister prescribed medicationsEncourage physical and mental supportEncourage client to eat small frequent feeds
Excess fluid volume related to cardiac failureas evidenced by edema ,dyspnea on exertion,increased weight gain Monitor intake and output chartAssess for presence of peripheral edemaAssess for jugular vein distentionFollow low sodium or fluid restrictionAuscultate breath soundsAdminister diuretic therapy
Impaired gas exchange related to increased preload,mechanical failure or immobility as evidenced byincreased respiratory rate, shortness of breath, anddyspnea on exertion Auscultate breath sounds q2hAssess respiratory rateAsses for cyanosisMonitor pulse oximetryPosition the client to facilitate breathingAdminister diuretic therapy
Ineffective tissue perfusion related to decreasedcardiac output Note colour and temperature of the skin q4hMonitor peripheral pulsesq4hProvide a warm environmentEncourage active rang of motionMonitor urine output
Activity intolerance related to fatiguesecondary to cardiac insufficiency andpulmonary congestion as evidenced bydyspnea,shortness of breath ,weakness,increased in heart rate on exertion space nursing activitiesSchedule rest periodsMonitor the clients response to activitiesInstruct the client to avoid activities thatincrease cardiac workload
Anxiety r/t to dyspnea or perceived threat of death asevidenced by restlessness, irritability Deficient knowledge related to disease process asevidenced by questions about the disease and prognosis
References KV Krishnadas. Text book of Medicine. 5thedition.Jaypee publications.New Delhi.2008 Marscall S. Runge. Georege A.Netter’sCardiology .2nd ed. USA .2014 Nicki R.Colledge,Brian R. Walker,StuartH.Ralston.Davidson’s Principles and Practiceof Medicine 21st edition 2010 Churchil LivingstoneElsevier page no 542-550 Richard Hatchett, David R Thompson. CardiacNursing. Elsevier publications. USA.2007
Heart failure Heart Failure is the inability of the heart to pump sufficient blood to meet the needs of the tissues for oxygen and nutrients. It is otherwise known as Congestive Cardiac Failure. Heart failure results in intravascular and interstitial volume overload and poor tissue perfusion. causes Reduced ventricular contractility