Transcription
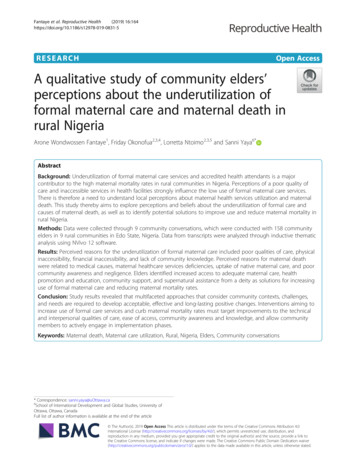
Fantaye et al. Reproductive Health(2019) EARCHOpen AccessA qualitative study of community elders’perceptions about the underutilization offormal maternal care and maternal death inrural NigeriaArone Wondwossen Fantaye1, Friday Okonofua2,3,4, Lorretta Ntoimo2,3,5 and Sanni Yaya6*AbstractBackground: Underutilization of formal maternal care services and accredited health attendants is a majorcontributor to the high maternal mortality rates in rural communities in Nigeria. Perceptions of a poor quality ofcare and inaccessible services in health facilities strongly influence the low use of formal maternal care services.There is therefore a need to understand local perceptions about maternal health services utilization and maternaldeath. This study thereby aims to explore perceptions and beliefs about the underutilization of formal care andcauses of maternal death, as well as to identify potential solutions to improve use and reduce maternal mortality inrural Nigeria.Methods: Data were collected through 9 community conversations, which were conducted with 158 communityelders in 9 rural communities in Edo State, Nigeria. Data from transcripts were analyzed through inductive thematicanalysis using NVivo 12 software.Results: Perceived reasons for the underutilization of formal maternal care included poor qualities of care, physicalinaccessibility, financial inaccessibility, and lack of community knowledge. Perceived reasons for maternal deathwere related to medical causes, maternal healthcare services deficiencies, uptake of native maternal care, and poorcommunity awareness and negligence. Elders identified increased access to adequate maternal care, healthpromotion and education, community support, and supernatural assistance from a deity as solutions for increasinguse of formal maternal care and reducing maternal mortality rates.Conclusion: Study results revealed that multifaceted approaches that consider community contexts, challenges,and needs are required to develop acceptable, effective and long-lasting positive changes. Interventions aiming toincrease use of formal care services and curb maternal mortality rates must target improvements to the technicaland interpersonal qualities of care, ease of access, community awareness and knowledge, and allow communitymembers to actively engage in implementation phases.Keywords: Maternal death, Maternal care utilization, Rural, Nigeria, Elders, Community conversations* Correspondence: sanni.yaya@uOttawa.ca6School of International Development and Global Studies, University ofOttawa, Ottawa, CanadaFull list of author information is available at the end of the article The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, andreproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link tothe Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication o/1.0/) applies to the data made available in this article, unless otherwise stated.
Fantaye et al. Reproductive Health(2019) 16:164Plain English SummaryNigeria has one of the highest rates of maternal deathsduring pregnancy, childbirth and after childbirth in thedeveloping world. The worst rates are seen in ruralNigerian communities. The major contributor to suchhigh rates in rural Nigeria is the underuse of maternalservices in health facilities. Instead, many rural Nigerianwomen use traditional services that are unsafe and notbased on scientific evidence. With the traditional influence of community elders’ perceptions and opinions onreproductive health decisions, such as the decision toseek delivery care in a hospital, it is important to understand what they think is causing underuse of healthfacilities and death during maternity, and to identifypotential solutions for their communities.Informal focus group discussions (community conversations) were conducted with influential communityelders in 9 different rural communities in Nigeria. Theybelieved that women underused maternal health servicesin health facilities because of poor care quality, difficultyof getting to health facilities, high costs of receiving care,and lack of knowledge about maternal health. Theybelieved that medical illnesses, poor availability of certain services, reliance on native maternal care and poorawareness caused maternal deaths. Increasing the accessibility of health facility services, promoting positivehealth behaviors, community support, and help fromGod were suggested as solutions for increasing theuptake of health facility services and reducing maternaldeath rates.BackgroundAccounting for nearly 66% of the global maternal mortality, many sub-Saharan African countries failed toachieve Millennium Development Goal (MDG) 5A ofreducing the maternal mortality ratio (MMR) by 75% between 1990 and 2015 [1]. Today, there is a renewedcommitment to Sustainable Development Goal (SDG)3.1 in achieving the target of less than 70 maternaldeaths per 100, 000 live births by 2030 [2]. Africa’s mostpopulous country, Nigeria, failed to meet MDG 5A witha percentage change in MMR of only 39.7% between1990 and 2015 [1]. Recent epidemiological data forNigeria approximates 58,000 maternal deaths per year,which accounts for the highest absolute number ofmaternal deaths in the world [1]. Although most maternal deaths are preventable, the inaccessibility andunderutilization of formal maternal healthcare servicesand trained health professionals sustains the high mortality rates across Nigeria and sub-Saharan Africa as awhole [1, 3]. Formal maternal healthcare services referto evidence-based services provided throughout the continuum of maternal care by accredited health professionals, often in a health facility setting [3]. Less thanPage 2 of 17half of Nigerian women make four or more formal antenatal care visits during their pregnancy, while approximately 60% of childbirths have taken place at homesince the 1990s [3]. During the postpartum period, onlyabout 33% of Nigerian women have utilized formal postnatal care since 2003 [3]. Costs of services, distance tohealth facilities, long waiting times and poor treatmentfrom professional attendants often deter Nigerianwomen from utilizing formal maternal healthcareservices [4].All parts of the country are affected, but there are majorurban-rural disparities in maternal health outcomes, inthat most maternal deaths occur in rural communities [5].Disparities are often the result of the unequal distribution,physical inaccessibility and financial inaccessibility of adequate maternal healthcare services and infrastructure inrural Nigeria [6–8]. Physical inaccessibility refers to distance, transportation, infrastructural, topographical, andresource availability-related barriers to receiving facilitybased care, while financial inaccessibility can include highcosts of transportation to facilities, high costs of medicalsupplies and services, and high costs of emergency care.The provision of maternal health care is the responsibilityof three tiers in the hierarchical system. The first point ofcontact and main source of formal maternal healthcareservices, which refer to evidence-based, maternal healthservices provided by accredited health professionals, is aprimary healthcare center (PHC) [9]. Rural populationsare significantly underserved in Nigeria, which highlightsthe inequity in their ability to access and use adequatePHC services, and ultimately the higher likelihood of maternal deaths in rural Nigeria [8, 10]. Accordingly, ruralwomen in Nigeria use modern contraceptives less andhave more abortions, and receive far less formal antenatal,childbirth and postnatal maternal care than urban women,putting them at higher risks for maternal mortality [3, 11].The continuation of the current trends in healthcareutilization amongst rural populations will impede Nigeriafrom meeting SDG 3.1 by 2030.According to Moore and the World Health Organization[12], respect for elders, approval by elders, and adherenceto elders’ advice is traditionally believed to be important inrural communities. In many rural African communities,chiefs and other community elders act as the main opinionleaders and primary decision makers, exerting the most influence on the daily life of community members [12, 13]. Inthe context of maternal health, such stature at the community, household and even individual level enables elders tohold traditionally-sanctioned influence over care-seekingwomen and their decisions from family planning to puerperium [13–20]. In parts of Nigeria, women’s decisions onmaternity care are largely within the traditional purview ofleaders in the household and/or in the local community[21, 22]. Community perceptions about health programs
Fantaye et al. Reproductive Health(2019) 16:164and health services affect utilization of health facilities [23].The perspectives and beliefs of elders can therefore have acritical influence on whether women seek and utilize evidence based maternal care. Their influence on maternalhealth indicates that Nigeria must incorporate influentialcommunity elders in maternal health strategies to helppush towards the SDG 3.1 target [24].Currently, the lack of evidence and poor understandingof the perceptions of influential elders on maternal healthcontributes to the poor maternal healthcare development,promotion, access and uptake in many rural communities.Consequentially, this has hindered the impact and successof national, regional and local maternal healthcare programs and services, and thereby the improvement of maternal health outcomes throughout Nigeria. This studyexplored community elders’ perceptions on the poor useof formal maternal care by women and causes of maternaldeath in rural communities in Edo State, Nigeria. It alsoaimed to identify potential solutions that can increaseutilization of evidence-based maternal care and reducematernal mortality. Literature on community interventions indicates that mobilizing community members totake charge of needs and tailoring programs to addressidentified community needs can increase their local acceptability and effectiveness [25, 26]. The study will helpus understand the local challenges, needs, and priorities,as well as the support that communities can provide forwomen to better access and utilize facility-based care. Inturn, this can help inform new or existing interventionsand increase their acceptability and effect in targeted Nigerian communities. Ultimately, findings will help improvethe utilization rates of evidence-based maternal care andreduce maternal mortality in study communities, andthereby Nigeria as well.Page 3 of 17community-based interventions across the country. Thispaper focuses on and reports findings on elders’ perceptions on maternal healthcare utilization and maternaldeath, which was a component from the qualitative segment of the project. A qualitative approach with aphased analytic plan that elicits themes was employed.This study was reported based on the Consolidated criteria for reporting qualitative research (COREQ) (seeattachment).Research settingNigeria has a population of over 190 million people,making it the seventh most populous country in theworld [27]. With one of the fastest population growthrates in the world, Nigeria has a total fertility rate of5.42 (live births per woman). Nigeria’s population is projected to rise to 411 million by 2050, which would makeit the third most populous country [27]. About 50% ofNigeria’s current population is rural [28]. Edo State,which is in the South-South geo-political zone, is one ofNigeria’s 36 federating States. It has approximately 4million people residing in 18 Local Government Areas(LGAs) [29]. Two of the predominantly rural LGAs inEdo State have been selected for this study: Esan SouthEast (ESE) and Etsako East (EE). Located in the riverineand rural parts of the state, the two LGAs combined fora projected population of 399,917 in 2015, with ESE accounting for a projected 212,055 and ETE accountingfor a projected 187,862 [30]. In addition to their rurality,these LGAs were selected following the preliminarybaseline assessments of the larger project due to relatively high maternal mortality rates and low PHCutilization rates among Edo State LGAs.Participants and recruitmentMethodsStudy designThe qualitative data reported in this study were extracted from within a larger, original project being carried out in Edo State Nigeria by The Women’s HealthAction Research Center and the University of Ottawawith the aid of a grant from the Innovating for Maternaland Child Health in Africa initiative- a partnership ofGlobal Affairs Canada (GAC), the Canadian Institutes ofHealth Research (CIHR) and Canada’s InternationalDevelopment Research Center (IDRC). The goal of theproject is to reduce maternal mortality in Nigeria bystrengthening the availability, accessibility, and use ofmaternal primary health care services by vulnerablewomen. The project is designed as a community-based,multi-site, and multi-disciplinary cluster randomizedtrial that uses a mixed methods approach. It wasdesigned to maximize community participation andownership in the design and implementation ofAt the baseline stage of the larger project, a geographicmapping of different communities was conducted duringa preliminary and scoping survey in ESE and ETE. As thefirst points of contact for maternal care, PHCs in ESE andETE were identified. Nine study communities determinedto have traditional age-based hierarchies across the twoLGAs were selected for community conversations, with 4having a local PHC and 5 not having a local PHC. Positivesocial changes in communities require the identificationand incorporation of the community members who have asignificant influence on local decision-making [31, 32].For this study, community elders ( 50 years of age) whowere locally recognized as influential opinion leaders werethe targeted participants. Their position in the traditionalhierarchy can help garner support for community initiatives, influence modernization of traditional beliefs andpractices surrounding maternal health, and improve theacceptance, effectiveness and success of maternal healthprograms.
Fantaye et al. Reproductive Health(2019) 16:164Study participants were recruited through purposive sampling using locally accepted methods of communication,which included meeting community chiefs or traditionalrulers before commencing recruitment of communitymembers. Accordingly, purposive sampling helped to ensure inclusion of elders who were considered local healthinfluencers and motivators. First, IDRC-affiliated projectleaders identified trusted indigenous guides in each community, who then introduced the project and the IDRCaffiliated local research team to the traditional ruler of theircommunity. Afterwards, the local research team met withthe traditional ruler of each community to explain researchpurposes, to obtain consent for the research, and to requesta meeting with elders. Community rulers scheduled meetings with community elders for data collection and helpedintroduce researchers to the participants. Recruitment of elders was continued until data saturation was reached [33].Data collectionThis study conducted community conversations (CCs) withcommunity chiefs and other elders who have a substantialinfluence on local practices. A CC involves members of acommunity coming together and holding discussions abouta concern, followed by the construction of resolutions tobring about social changes [34]. In accordance, this form ofdata collection has been found to be effective in someAfrican communities in resolving difficult social problemsand getting affected communities to control the process ofchange relating to those problems. CCs have helped raiseawareness and address a range of issues, such as the following: HIV testing and prevention, female genital cutting, andchild marriage [35], as well as mental health stigma amongethnic minorities [36] and health issues in rural NativeAmerican populations [37]. An assessment of CCs as acommunity engagement tool found that the method helpedincrease awareness among community members, provideda voice for members to share concerns, and facilitateddiscussions about significant topics [38]. CCs effectivelycreated a participative environment, promoted relationshipbuilding and collaboration among community membersand between community members and external stakeholders in discussing potential solutions to identified problems, as well as planning future actions [38]. In ruralcommunities, CCs are especially common and effective fortransferring information, driving social interactions andchange, and altering local beliefs [34, 37, 39].For this study, the conversations were designed to enableelders to share and discuss their views and concerns aboutmaternal mortality and use of facility-based maternal healthcare, as well as to proffer potential solutions. These conversations helped to identify local needs, priorities and thesupport that communities in the LGAs can provide and require for women seeking evidence-based services. Proposedsolutions to the identified maternal health problems lay aPage 4 of 17foundation for intervention components that would be acceptable to specific rural communities. The CCs were conducted in Pidgin English and a few in local languages (Ishanand Etsako) by trained IDRC project-affiliated investigators,including FO and LN. During the baseline phase, prior tothe formative phase of the project, a baseline study was conducted in 20 randomly selected communities in Etsako Eastand Esan South East LGAs (10 from each LGA). Nine studycommunities were selected from the 20 communities basedon the presence and residence of influential elders, as wellas the traditional rulers ruling these communities. A total of9 CCs were conducted with 6 in ESE and 3 in ETE. Thenumber of participants in each CC ranged from 12 to 21,small enough to allow all members to speak, but largeenough to maximize conversations from elders with different opinions. The CCs were conducted outdoors by themeans of a CC topic guide designed to gather perceptionsabout maternal health related topics. The guide was developed by a technical committee in charge of preparing research instruments for the larger project. The members ofthe committee were familiar with the cultures of the projectcommunities and the pertinent questions for the conversations. All the research instruments and procedures, including the CC topic guide, were piloted in a suburb of Benincalled Oluko with 12 men ( 50 years of age). Meetings hadfacilitators who guided the conversations with the topicguide, which was also designed to involve the participants inproblem solving. The facilitators were IDRC project- affiliated field supervisors who held traditional positions, such aschieftaincy, or were conversant with the traditions of studycommunities. These facilitators were experienced qualitativeresearchers who spoke Standard English, Pidgin English,Ishan and Etsako. Facilitators received project specific training in qualitative data collection and in facilitating CCsbefore field work. FO and LN were senior IDRC project investigators who oversaw the recruitment and data collectionstages in ESE and ETE.At the start of meetings, traditional methods of meeting with the community leader were used, including thesharing of kolanuts and requests for traditional prayersfor research success. The reasons for conducting theproject were then explained, after which the elders wereengaged to share existing problems in maternal care.They were encouraged to partake in creating solutionsto identified problems and in community relevant andappropriate action plans to help improve maternalhealthcare utilization. Discussions in the CCs lasted forapproximately 90 min to give all the participants achance to express their thoughts. The discussions endedwhen no further topics arose (point of saturation). Afterclosure of the meetings, resolutions were itemized andread to the elders for respondent validation. The eldersreviewed the resolutions and thereafter gave feedback onthe itemized resolutions. Proceedings in the meetings
Fantaye et al. Reproductive Health(2019) 16:164were audio-recorded, transcribed and reviewed for clarity and accuracy of the transcription. Participants’ responses were either transcribed verbatim if theyresponded in English or translated if they responded inPidgin English and one of the local languages. Literaltranslation (word-by-word) was used to preserve theparticipants’ responses and provide readers with an understanding of their mentality [40]. They were assignedcodes to remove any identifying information that couldjeopardize their anonymity and privacy.Data analysisPrior to commencing analysis, audio-recorded conversations were transcribed with the assistance of translators.Data from transcripts were analyzed through inductivethematic analysis using NVivo 12 software. Braun &Clarke’s [41] guide for conducting a thematic analysis wasfollowed as it enables a transparent and rigorous analysisthat produces pertinent information required for thestudy’s research approach. The theoretical flexibility ofthematic analysis enabled us to analyze different aspectsof the research objectives, developing or extending understanding of elders’ perceptions. It also helped reflect therichness, the detail and the in-depth nature of the qualitative data collected in the study [41]. The primary and corresponding author independently read the transcriptsrepeatedly to get immersed into the raw data and makenote of initial topics and ideas relevant to the researchquestion. The transcripts were coded in an iterative manner, revisiting the transcripts and altering and modifyingthe codes as reflected by the data and the emerging patterns. Excessively detailed word-by-word or line-by-linecoding reduces the ability to see patterns among and between pieces of data [42]. Lines of text were thereby codedbroadly, often ranging from a sentence to several sentences, to ensure that the intentions in the participants’views were not lost. Many references under each code alsoincluded some surrounding data to ensure the context ofmeaning was intact, acknowledging that some texts can becategorized into different codes. The primary author(AWF) and corresponding author (SY) then discussedtheir codes and resolved any differences in coding, afterwhich a final consensus agreement was reached. Themesand subthemes were developed from the codes and thedataset after making sense of the patterns in the codeddata relative to the research question [41]. The finalthemes were validated and were accepted as being representative of the data within the context of the researchquestion. The final themes were named to tell the story ofthe categorized codes. Selected quotes in the reporting offindings are chosen to represent a typical response relativeto the reflected theme. Given the inductive nature of thedata analysis, saturation was achieved when no morecodes or patterns emerged from the data.Page 5 of 17TrustworthinessTrustworthiness of qualitative research is crucial for ensuring a rigorous study that produces findings capable ofmaking an impact on policy or practice [43]. Multipleauthors are involved in data collection and analysis.Following data collection from the CCs, FO and LNemployed member-checking in order to receive validation and ensure credibility of the proffered solutions.Multiple coders (AWF and SY) were used to independently code the data and then to collaboratively refinetheir proposed codes and thematic patterns. Feedbackwas received from field investigators FO and LN, whohave ample experience in reproductive health researchin rural sub-Saharan Africa and are involved in the larger project as principle investigators. Clarifications, project issues, thematic misinterpretations, contradictions,factual errors, and reporting of study findings wereraised and discussed. A colleague with qualitative research experience was also engaged by the primary author to serve as an external auditor and further ensuredependability.To ensure confirmability, the decisions made in the research process starting from the research objectives tothe interpretation of findings are thoroughly described,along with examples of data to support findings andconclusions [44]. Data is collected from male elders andfemale elders, the latter having had more direct experiences with maternity in their life course. Data is also collected from multiple locations in the two LGAs, therebyinvolving different elders in each community. This datatriangulation helped enrich and deepen the understanding of study findings [43, 44].EthicsEthics approval for the larger project was granted by the National Health Research Ethics Committee of Nigeria(NHREC) – number NHREC/01/01/2007–18/04/2017. Ethics approval for this qualitative study was received from theUniversity of Ottawa Research Ethics Board (REB) on 18/03/2019. Participants were voluntarily enrolled in the studyon the basis of a free and informed consent. Participantswere informed that information collected from the researchproject would be used to understand the current communityneeds, to improve the future usage of evidence-based maternal health services, and to improve maternal health outcomes in their community and Edo State. Participants werethen informed that once they chose to participate, theycould withdraw at any time and/or refuse to answer anyquestions, without suffering any negative consequences. Permission to audio-record the community conversations wassought and obtained before data collection. Processes formanaging and storing the audio files from the CCs were putin place to further ensure confidentiality of study participants. All personal identifiers were removed from transcripts
Fantaye et al. Reproductive Health(2019) 16:164and in quoted texts below. However, participants were informed that information shared in CCs is exposed to otherparticipants and may be a limit to their overall confidentiality due to the inability to completely control the actions ofothers. Written informed consent was obtained from all participants prior to their participation.ResultsCharacteristics of study participantsA total of 151 men and 7 women aged 50–101 years ofage participated in the community conversations. Mostof them attained post-primary education, whereas a fewhad no education. The majority were farmers and artisans. Majority of the participants were Christians, and afew declared no religious affiliation.Reasons for underutilization of formal maternal careQuality of careThe elders mentioned various reasons related to qualityof care, perceived or actual, that contributed to the reduced uptake of facility-based care. A recurrently statedreason was understaffing in health facilities, and the corresponding inability of such facilities to meet the needsof their clientele. The lack of health professionals inPHCs and even some hospitals was a major deterrent.Several elders exclaimed that understaffing issues werethe consequence of posted nurses and doctors skippingtheir work duties at the facility. The absence of nursesand doctors prevented community members from receiving skilled care from health professionals:“this is Nigeria, it is poorly equipped, even the so-calledgeneral hospital, I can’t say it’s a no go area, but we allknow what happens there when you get there, it’s eitherthe doctor is absent or the nurses are absent” (CC 02,ETE, Male).“may God keep you all, the health center that they saidis here there is no nurse where three nurses are supposedto be on duty - it is only one nurse you will see, in a weekyou will not see them - if someone sustains any injuryand is rushed there you will not see nurses unless you goto the next community which is Ewohimi or Ubiaja fortreatment” (CC 08, ESE, Male).Elders expressed their frustrations with the perceivedunprofessionalism of health professionals, includingthose who were absent from workplace duties. They criticized them for not seeming to take their jobs seriously,and instead carrying out personal tasks, such as shopping, during work hours:“the habit of absenteeism is very common among themlet’s say you ask a nurse to wait for you she will go to themarket until the later hours before she comes back oruntil the next day. For example, there was a patientbrought to the health center, there was no nurse to givePage 6 of 17treatment. The next thing was to take the person to thenearby chemist [collective laughter]” (CC07, ESE, Male).Some health professionals were said to display patientfavoritism when deciding which patient to treat first.There were also accusations of financial status discrimination in which patients with higher wealth status andinfluence received more prompt treatment and attentionthan patients with lower wealth status. Nurses were particularly accused of not following protocol and fulfillingduties, including referrals of patients to their own homesfor care and abandonment of their facility duties duringwork hours:“It is not because of the charges, I have never seen anyone who comes back after good care and complains thatthe money is too much and tells other women not to go.The reasons are the nurses are not always on duty fortheir primary assignment, and even if they are there onduty they will take you to their home for treatment orthey will refer you to a place where by the time you getthere, it is the same person who referred you that you willmeet there” (CC 07, ESE, Male).Some patients who were rushed to a health center dueto an accident were said to
services provided by accredited health professionals, is a primaryhealthcarecenter(PHC)[9]. Rural populations are significantly underserved in Nigeria, which highlights the inequity in their ability to access and use adequate PHC services, and ultimately the higher likelihood of ma-ternal deaths in rural Nigeria [8, 10]. Accordingly, rural