Transcription
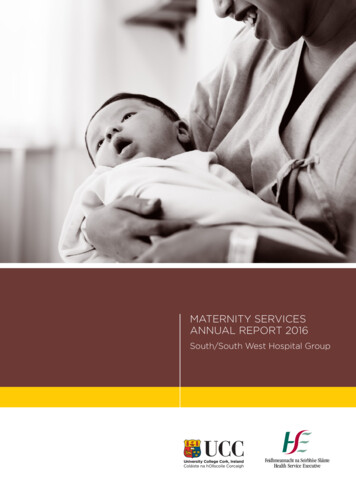
MATERNITY SERVICESANNUAL REPORT 2016South/South West Hospital Group
ContentsForeword1Introduction3Our Hospitals4Obstetric Report6Maternal Mortality9Very Low Birthweight Infants17StaffResearch and Innovation2021
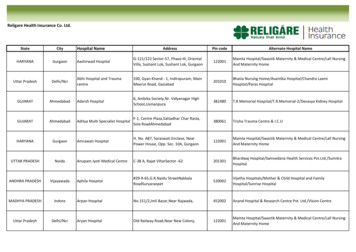
Maternity Services Annual Report 2016CLINICAL DATA – LIST OF TABLES AND FIGURESMaternal and Delivery CharacteristicsTable 1.0:Frequency (N) of maternities and births 2014 – 2016Table 1.1a:Distribution of maternal and delivery characteristics 2016Table 1.1b:Distribution of maternal and delivery characteristicsTable 1.2:Distribution of spontaneous and instrumental vaginal birth for all infants, 2016Table 1.3:Incidence of caesarean delivery for all maternities, 2016Table 1.4:Incidence of maternal high dependency unit admission and hospital readmissionPerinatal MortalityTable 2.0:Perinatal deathsTable 2.1:Perinatal mortality ratesTable 2.2:CUMH StillbirthsTable 2.3:CUMH case review – Intrapartum deathsTable 2.4:CUMH case review – Antepartum deathsTable 2.5:CUMH - Early neonatal deathsTable 2.6:CUMH case review – Early neonatal deathsTable 2.7:CUMH case review – Late neonatal deathsTable 2.8:CUMH case review – Infant deathsTable 2.9:STGH StillbirthsTable 2.10: STGH case review – StillbirthsTable 2.11:STGH – Early neonatal deathsTable 2.12: STGH case review – Early neonatal deathsTable 2.13: UHK case review – StillbirthsTable 2.14: UHK case review – Antepartum deathsTable 2.15: UHK – Early neonatal deathsTable 2.16: UHK case review – Early neonatal deathsTable 2.17: UHW StillbirthsTable 2.18: UHW case review – Antepartum deathsTable 2.19: UHW – Early neonatal deathsTable 2.20: UHW case review – Early neonatal deathsTable 2.21: UHW case review – Late neonatal deathsTable 2.22: UHW case review – Infant deathTable 2.23: Autopsy RateVery Low Birthweight InfantsTable 3.0:Number of admissions to the Neonatal unit by yearTable 3.1:VLBW Infants born to the Neonatal unitTable 3.2:Number of VBLW infants 2014 – 2016Table 3.3:Gestational age of VLBW infants admitted to the NNU 2014 – 2016Table 3.4:Birthweight of VLBW infants admitted to the NNU 2014 – 2016Table 3.5:Additional Clinical demographics of VLBW Infants 2014 – 2016Table 3.6:Summarises respiratory support for VLBW infants 2014 – 2016Table 3.7:Major Morbidities amongst VLBW infants admitted to NNU 2014 – 2016Gynaecology Outpatient ActivityTable 4.0: Gynaecological Outpatient ActivityStaffTable 5.0:Overall SSWHG Staff NumbersFigure 1.1:Distribution of maternal and delivery characteristics – NationalityFigure 1.2: Research Income in the Department of Obstetrics and Gynaecology 2007 – 20163
South/South West Hospital Group Maternity Services Annual Report 2016ForewordIn welcoming our third consolidated annual report (2016) on maternity servicesin the South/South West Hospital Group. I wish to acknowledge the growingcooperation within the group. This year, we include additional information on ourneonatology services as they continue to develop a group-wide neonatology serviceacross Waterford, South Tipperary, Cork and Kerry. The Report sets out service andperformance data for 2016 and places before the public a wide array of numericinformation on the maternity and neonatology services of the South/South WestHospital Group. As we move into our third year, we can begin to identify trends thatin future years will enable us to discern our direction of development and measure itagainst similar national and international comparators.Towards the end of the year, the South/South West Hospital Group established a groupclinical directorate for maternity services embracing neonatology and gynaecology.This fulfils the expectation expressed in our last report and represents a major initiativein clinician management that will strengthen what the National Maternity Strategy*describes as “the sharing of expertise within (maternity) networks” and “the operationalresilience of smaller units”. Work is ongoing on codifying governance and managementstructures and setting down protocols and procedures for the new Directorate.It is my pleasure to acknowledge the continuing work and dedication of our staff whodeliver services for women and their newborn infants in our four units in Waterford,Clonmel, Cork and Tralee, of the managers who support them and the primary carepractices who refer to us. I offer sincere thanks to you all.Professor Geraldine McCarthyChairperson of the South/South West Hospital Groupand Professor Emeritus, University College Cork.*Creating a Better Future Together: National Maternity Strategy 2016-20261
Maternity Units of the South/South West Hospital GroupSouth TipperaryGeneral HospitalUniversity HospitalKerryUniversity HospitalWaterfordCork UniversityMaternity Hospital2
Maternity Services Annual Report 2016IntroductionThe South/South West Hospital Group serves apopulation of over 800,000 people and every daymore than 8,800 staff contribute to our results incare, cure, research and education.2016 was the year that saw the continueddevelopment of the South/South West Hospitalgroup as the corporate management entity overthe nine hospitals in the group and the growth of amore integrated approach to the delivery of acuteservices. It is of course a work in progress but eachyear brings the reality of a unified hospital trustthat much closer. There are four maternity unitsin our group, namely Cork University MaternityHospital, University Hospital Waterford, UniversityHospital Kerry and South Tipperary GeneralHospital. In 2016 there were 11,745 mothers whodelivered 12,011 babies in SSWHG maternity unitswhich translates to an average of 33 births per dayacross the group. This represents approximately19% of all births in the Republic of Ireland. Thisfigure is similar to 2015 and slightly higher than thenational drop in births of 3% from to 65,909 (2015)to 63,897 (2016).neonates at 28 weeks or less to the regional centreare working satisfactorily. This is only possibleif the referring units accept back responsibilityfor the neonates once they are old enoughand healthy enough and this is indeed what ishappening. In this report we are able to includedata on Very Low Birthweight Infants as definedby the Neonatal Intensive Care Outcome andResearch Evaluation (NICORE) Ireland groups;that definition is “any infant who is born alive atyour hospital/in your hospital group and whosebirth weight is between 401 and 1500 grammes orwhose gestational age is between 22 weeks 0 daysand 29 weeks 6 days (inclusive).”Data on perinatal mortality is included again thisyear. Next year’s report will be able to reportsignificant progress on gynaecology waiting listmanagement. As of 2016 however, it continues tobe our biggest clinical risk.Sincere gratitude is offered to the staff of ourfour Maternity Units in providing the data for thisreport. Their commitment and time to this processis ever appreciated.Admissions to our neonatal units include manyof the most demanding cases we care for. Thenew national standards requiring the transfer of3
South/South West Hospital GroupCork University Maternity HospitalSouth Tipperary General HospitalUniversity Hospital KerryUniversity Hospital WaterfordOur HospitalsCork University Maternity HospitalCork University Maternity (CUMH) Hospitalopened in 2007 and involved the amalgamationof maternity services from Erinville Hospital, St.Finbarr’s Maternity Hospital, Bon Secours MaternityUnit and gynaecology services from Cork UniversityHospital. In 2016 CUMH delivered 7,629 babies andover 16,000 patient contacts were recorded ingynaecology and colposcopy clinics.CUMH maternity services comprises of: 12 bedded delivery suite 87 bedded postnatal ward 31 bedded antenatal ward 24 bedded gynaecology ward(16 gynaecology and 8 other) Stand alone outpatients department for antenatal,gynaecology, urodynamics, colposcopy &midwifery led scanning department.4Maternity Services at CUMH support the educationof undergraduate Nursing & Midwifery Studentsfrom University College Cork (UCC).Medical students from UCC also gain clinicalexperience as part of their placement and thislends to an interdisciplinary teaching environment.Facilities in the Department of Obstetrics andGynaecology at CUMH allow students to participatein lectures with study space and video conferencingfacilities to link with their colleagues at other sites.The educational team of the Centre for MidwiferyEducation, CUMH is committed to the developmentand provision of programmes of education andtraining for registered Midwives and Nurses, tosupport service delivery. All programmes supportthe on-going maintenance of clinical competenceand promote evidence based care.
Maternity Services Annual Report 2016South Tipperary General HospitalSouth Tipperary General Hospital (STGH) openedin 2008. This hospital provides acute hospitalservices for the population of County Tipperary.In 2016, STGH delivered 1,032 babies and providedgynaecology and colposcopy clinics.Maternity Services at STHG support the educationof undergraduate Medical students from UniversityCollege Cork and University of Limerick andundergraduate Nursing & Midwifery students fromUniversity College Cork.STGH Maternity Services comprises of: 2 bedded delivery suite and obstetric theatre 28 bedded maternity ward 10 bedded gynaecology ward Stand-alone outpatients department for antenatal,gynaecology, urodynamics, colposcopy &midwifery led scanning department.Facilities allow students to participate in lectureswith study space and video conferencing facilitiesto link with their colleagues at other sites.University Hospital KerryUniversity Hospital Kerry (UHK) opened in 1984. Thehospital provides acute general hospital services tothe population of Co. Kerry. In 2016, UHK delivered1,410 babies and 1,326 patients contacts wererecorded in gynaecology clinics.UHK maternity services comprises of: 4 bedded delivery suite 24 bedded postnatal/gynaecology ward 9 bedded antenatal ward Stand-alone outpatients department for antenatal,gynaecology, urodynamics, & midwifery ledscanning department.Maternity Services support the education ofundergraduate Nursing Students from the Instituteof Technology Tralee (ITT).Medical students from UCC also gain clinicalexperience as part of their placement and thislends to an interdisciplinary teaching environment.Facilities at UHK allow students to participate inlectures with study space and video conferencingfacilities to link with their colleagues at other sites.University Hospital WaterfordUniversity Hospital Waterford (UHW) opened in1952 (Ardkeen Hospital) and is one of the busiestregional hospitals in the Country. In 2016, UHWdelivered 1,940 babies and over 10,041 patientcontacts were recorded in gynaecology andcolposcopy clinics.UHW Maternity Services comprises of: 4 bedded delivery suite with a 3 bedded1 stage room Obstetric theatre on delivery suite with arecovery room 24 bedded postnatal ward 32 bedded antenatal gynaecology ward thathouses the early pregnancy unit and a specificallynominated bereavement room Stand-alone outpatients department forantenatal, gynaecology, urodynamics, colposcopy& midwifery led scanning department.Maternity Services at UHW support the educationof undergraduate Midwifery Students from theUniversity of Limerick (UL) and undergraduateNursing Students from Waterford Institute ofTechnology (WIT) as well as elective placementsof Postgraduate Midwifery Students from Cork(UCC) & Dublin to the Integrated Hospital andCommunity Midwifery Service (IHCMS) to completethe midwifery and nursing education programme inWaterford.Medical students from University College Cork(UCC) and Royal College of Surgeons Ireland(RCSI) also gain clinical experience as part of theirplacement and this lends to an interdisciplinaryteaching environment. Facilities allow students toparticipate in lectures with study space and videoconferencing facilities to link with their colleaguesat other sites.5
South/South West Hospital GroupObstetric ReportMaternal and Delivery CharacteristicsTable 1.0: Frequency (N) of maternities and births 2014 - 2016SSWHGCUMHSTGHUHKUHWMothers delivered 201611,7457,4421,0171,3891,897Mothers delivered 201512,3437,9031,0541,3891,997Mothers delivered 201412,4737,8781,4341,0872,074Babies born 500g 201612,0117,6291,0321,4101,940Babies born 500g 201512,6208,1131,0621,4062,039Babies born 500g 201412,7468,0711,4541,1022,119Figure 1.1: Distribution of maternal and delivery characteristics 2016 - NationalityIrishNon-Irish EU NationalOther*STGH data not included6
Maternity Services Annual Report 2016Table 1.1a: Distribution of maternal and delivery characteristics quencyUHWFrequencyN (%)(N 11,745)N (%)(N 7,442)N (%)(N 1,017)N (%)(N 1,389)N (%)(N nsTable 1.1b: Distribution of maternal and delivery uencyUHKFrequencyUHWFrequencyN (%)(N 11,745)N (%)(N 7,442)N (%)(N 1,017)N (%)(N 1,389)N (%)(N 81(67.0)937(67.5)1,191(62.8)7
South/South West Hospital GroupTable 1.2: Distribution of spontaneous and instrumental vaginal births for all infants, 2016SSWHGCUMHSTGHUHKUHWN (%)(N 12,011)N (%)(N 7,629)N (%)(N 1,032)N (%)(N 1,410)N (%)(N 1,940)Vaginal delivery 43(74.4)Spontaneous )55(3.8)Combined instrumental57(0.7)57(1.1)–––Vaginal breech51(0.6)40(0.7)3(0.5)1(0.1)7(0.5)Table 1.3: Incidence of caesarean delivery for all maternities, 2016SSWHGCUMHSTGHUHKUHWN (%)(N 11,745)N (%)(N 7,442)N (%)(N 1,017)N (%)(N 1,389)N (%)(N 1,897)Caesarean 49.7)265(54.2)227(48.5)Elective and emergency figures are calculated on the total number of caesarean deliveriesTable 1.4: Incidence of maternal high dependency unit admission and hospital readmissionSSWHGCUMHSTGHUHKUHWN (%)(N 11,745)N (%)(N 7,442)N (%)(N 1,017)N (%)(N 1,389)N (%)(N 1,897)Admission to HDU508(4.3)487(6.5)013(0.9)8(0.4)Readmission after delivery309(2.6)258(3.5)0051(2.7)Admission StatusNo HDU unit in STGH8
Maternity Services Annual Report 2016Maternal MortalityThere was one maternal mortality recorded in 2016.Mortality A was the case of a patient who died secondary to a Road Traffic Accident(Classification: Coincidental)Perinatal MortalityTable 2.0: Perinatal deathsPerinatal deathsSSWHG(N 12,011)CUMH(N 7,629)STGH(N 1,032)UHK(N 1,410)UHW(N 1,940)Antepartum deaths3821269Intrapartum deaths22000Stillbirths4023269Early neonatal deaths2012314Late neonatal deaths62004Infant deaths32001** Stillbirth: Baby delivered without signs of life from 24 weeks gestation or with a birthweight 500g.1Early neonatal death: Death of a live born baby occurring within 7 completed days of birth.Late neonatal death: Death of a live born baby occurring after the 7th day and within 28 completed days of birth.1Stillbirths Registration Act, 1994.**As used by the National Perinatal Epidemiology Centre9
South/South West Hospital GroupTable 2.1: Perinatal mortality ratesSSWHG(N 12,011)CUMH(N 7,629)STGH(N 1,032)UHK(N 1,410)UHW(N 1,940)Overall perinatal mortalityrate per 1000 births5.04.64.85.06.7Perinatal mortality ratecorrected for congenitalanomalies3.02.62.92.84.6Stillbirth rate per1000 births3.33.01.94.34.6Stillbirth rate correctedfor congenital anomalies2.01.61.92.83.1Early neonatal death rateper 1000 births1.71.62.90.72.1Early neonatal death ratecorrected for congenitalanomalies1.01.11.00.01.6All infants weighing 500g and/or over 24 weeks’ gestation are reported.All mothers who booked and delivered are includedCUMH Case ReviewsTable 2.2: CUMH Stillbirths (n 23)CauseTotalsCongenital anomalies11Placental abruption2Placental (all causes)7Fetal3Table 2.3: CUMH case review – Intrapartum deaths (n 2)10ParityGestation(Wks.)Mode ofdeliveryBW(g)Conclusion037 6SVD2100Trisomy 18039 4Instrumental3410Meconium induced myonecrosis
Maternity Services Annual Report 2016Table 2.4: CUMH case review – Antepartum deaths (n 21)ParityGestation(Wks.)Mode ofdeliveryBW(g)Conclusion224 3SVD540Placental insufficiency Hypercolied umbilicalcord with fetal vascular malperfusion137 6SVD2860IUFD due to feto-maternal haemorrhageoccurring on a background of pregnancyvulnerability due to the presence ofplacental distal villous immaturity2 337Elective C/S1980Trisomy 181 136 6SVD1680Trisomy 131 239 4SVD2680Placental insufficiency caused by acombination of placental hypoplasia,delayed villous maturation and fetalvascular malperfusion0 133 4SVD2100Placental insufficiency caused by acombination of hypercoiled umbilical cord,fetal vascular malperfusion and delayedvillous maturation226 4SVD740Trisomy 182 135/40Elective C/S1300Trisomy 18137SVD210Trisomy 182 136 5SVD29803 126 5C/S3602 135 4SVD2960Single dysplastic kidney, pulmonaryhypoplasia, HLHS, thymic hypoplasia231 1SVD1500IUD due to fetal vascular malperfusion as aresult of acute thrombosis of an umbilicalartery136 6SVD2840Placental abruption124 2SVD540Abnormal- Trisomy 213 429 6Breech1260Renal agenesis226 4SVD1040Non-immune hydrops with anaemia andheart failure secondary to suspectedfetomaternal haemorrhagePlacental abruption, clinical and placentalevidenceTwin-twin transfusion syndrome026Breech480Placental insufficiency due to maternalvascular malperfusion, fetal vascularmalperfusion and retroplacentalhaemorrhage026SVD600Multiple congenital abnomalies withplacental insufficiency028 1SVD690Abnormal-Trisomy 18237 4SVD2440Diffuse severe delayed villous maturation,fetal vascular malperfusion with ahypercoiled cord11
South/South West Hospital GroupTable 2.5: CUMH Early neonatal deaths (n 12)CauseTotalsCongenital anomalies4NEC/Perf1Prematurity3Pulmonary hypoplasia1Non Immune Hydrops1Hypovolemic shock 2nd to Vasa Previa1Potters Sequence1Table 2.6: CUMH case review – Early neonatal deaths (n 12)GABW(g)Age(days)Cause of DeathPlace2466036 (mins)Extreme PrematurityCUMH34–3NEC/PerfCUMH382120100 (mins)Trisomy 18CUMH22 46201Extreme PrematurityCUMH35 5300340 (mins)Non Immune HydropsCUMH37 218801Trisomy 18CUMH38174010 (mins)AnencephalyCUMH258001PrematurityCUMH26 27001Potters SequenceCUMH3718004EncephaloceleCUMH36 227301Hypovolemic shock 2nd to Vasa PreviaCUMH29 414202Pulmonary hypoplasiaCUMHTable 2.7: CUMH case review – Late neonatal deaths (n 1)GABW(g)Age(days)Cause of DeathPlace2362010Extreme PrematurityCUMHTable 2.8: CUMH case review – Infant deaths (n 2)12GABW(g)Age(days)Cause of DeathPlace orTransferred to24 6–38Extreme PrematurityCUMH41 43560110LissencephalyCUMH
Maternity Services Annual Report 2016STGH Case ReviewsTable 2.9: STGH Stillbirths (n 2)CauseTotalsCord2Table 2.10: STGH case review – Stillbirths (n 2)ParityGestation(Wks.)Mode ofdeliveryBW(g)Conclusion1 033 2EmergencyC/STwin1 1980Cord entanglement in mono-amniotic1 033 2EmergencyC/STwin2 2340Cord entanglement in mono-amnioticTable 2.11: STGH – Early neonatal deaths (n 3)CauseTotalsCongenital anomalies2APH1Table 2.12: STGH case review – Early neonatal deaths (n 3)GABW(g)Age(days)Cause of DeathPlace of death38 624402hrs 15 mins oldTransposition of the greatarteriesSTGH32 316809hrs oldThanatophoric Dysplasia APHSTGH30 414701 day 5 hrs oldAPH Velementous CordInsertion @ 30 4 WksNMH13
South/South West Hospital GroupUHK Case ReviewsTable 2.13: UHK – Stillbirths (n 6)CauseTotalsCongenital anomalies2Query IUGR1Placental Abruption1Fetal1Unexplained1Table 2.14: UHK case review – Antepartum deaths (n 6)Gestation(Wks.)Mode ofdeliveryBW(g)Conclusion37 5SVD–No Fetal Heart on admission. PM normal. Histologyretroplacental haematoma. Cytogenetics normal35 5SVD2930Poorly controlled diabetic. No FH on routine a/nvisit.2.93kg. histology single uterine artery in cord. GBSisolated. Cytogenetics Trisomy 21.Term 3SVD–Admitted with pains and FM’s. No FH on admission.Normal histology, cytogenetics, placental swabs.Unexplained35 1SVD–Presented with PPROM and pains. No FH. Hx FM’sreported. Declined PM. Normal male infant. Severeacute Chorioamnionitis.24SVD–Poor obs hx. PM done. Cytogenetics abnormalchromosome 2037 6SVD2640Presented with no FM’s and no Fh present. Dietcontrolled gest diabetic. PM, Cytogenetics histologyswabs done. Result Normal Female fetus, normalKaryotype. Normal histology. Query IUGRTable 2.15: UHK – Early neonatal deaths (n 1)CauseTotalsCongenital anomalies1Table 2.16: UHK case review – Early neonatal deaths (n 1)14GABW(g)Age(days)Cause of DeathPlace of death36 4–6PPROM 30hrs: Hypoplastic leftHeart – not suitable for surgeryCrumlin
Maternity Services Annual Report 2016UHW Case ReviewsTable 2.17: UHW – Stillbirths (n 9)CauseTotalsCongenital anomalies3Placental abruption1Placental (all causes)1 APHFetal2Infection (GBS)1Unexplained / Unclassified1Table 2.18: UHW case review – Antepartum deaths (n 9)ParityGestation(Wks.)Mode ofdeliveryBW(g)Conclusion2 037 3CaesareanSection2750Abruption3 034 5CaesareanSection1030Congenital diaphragmatic hernia1 039 3SVD2753Unexplained0 135 3SVD665CNS Anomoly2 035 2SVD2090Antepartum haemorrhage1 028 3SVD310LBW unknown1 040 4SVD3630Fetal Vasculitis2 025 6SVD610LBW unknown1 027 6Vaginal Breech310Trisomy 18Neonatal deathsTable 2.19: UHW – Early neonatal deaths (n 4)CauseTotalsCongenital anomaly1Prematurity315
South/South West Hospital GroupTable 2.20: UHW case review – Early neonatal deaths (n 4)GABW(g)Age(days)Cause of DeathPlace of death22 6 weeks6301 hrPrematurityUHW32 weeks18201 HrCongenital anomaliesUHW22 6 weeks52030 minsPrematurityUHW26 5 weeks9101 dayPrematurity with IVHNMHTable 2.21: UHW case review – Late neonatal deaths (n 4)GABW(g)Age(days)Cause of DeathPlace of death39 130009Fetal Maternal HaemorrhageNMH39345017Spinal Muscular Atrophy (SMA)CUMH42350013HIE Maternal SepsisCUMH40 4398010Metabolic DisorderTemple StreetTable 2.22: UHW case review – Infant death (n 1)GABW(g)Age(days)Cause of DeathPlace of death25 382533PrematurityTemple streetPerinatal pathologyTable 2.23: Autopsy 4 (60.0)18 (78.3)0 (0)4 (66.7)2 (22.2)Early Neonatal Deaths8 (40.0)7 (58.3)1 (33.3)0 (0)0 (0)Overall autopsy rate for Stillbirths and Early Neonatal Deaths is 53.3%16
Maternity Services Annual Report 2016Neonatal ReportTable 3.0: Number of admissions to the Neonatal Unit by year201620152014SSWHGN(%)(N 12,011)CUMHN(%)(N 7,629)STGHN(%)(N 1,032)UHKN(%)(N 1,410)UHWN(%)(N 1,940)2,170 (18.1)1,187 (15.6)241 (23.4)295 (20.9)447 (23.0)SSWHGN(%)(N 12,620)CUMHN(%)(N 8,113)STGHN(%)(N 1,062)UHKN(%)(N 1,406)UHWN(%)(N 2,039)2,340 (18.5)1,363 (16.8)305 (28.7)247 (17.6)425 (20.8)SSWHGN(%)(N 12,746)CUMHN(%)(N 8,071)STGHN(%)(N 1,454)UHKN(%)(N 1,102)UHWN(%)(N 2,119)2,252 (17.7)1,328 (16.5)271 (18.6)234 (21.2)419 (19.8)Very Low Birthweight Infants (VLBW)As per the Neonatal Intensive Care Outcome and Research Evaluation (NICORE) Ireland groups, thedefinition of VLBW is any infant who is born alive at your hospital/in your hospital group and whosebirth weight is between 401 and 1500 grams or whose gestational age is between 22 weeks 0 daysand 29 weeks 6 days (inclusive).Table 3.1: VLBW Infants born to the Neonatal UnitSSWHG(N 356)CUMH(N 259)STGH(N 9)UHK(N 23)UHW(N 65)201611290281220151319548242014113743729Table 3.2: Number of VBLW infants 2014 – 2016SSWHGN(%)(N 6,762)CUMHN(%)(N 3,878)STGHN(%)(N 817)UHKN(%)(N 776)UHWN(%)(N 1,291)356 (5.3)259 (6.7)9 (1.1)23 (3.0)65 (5.03)17
South/South West Hospital GroupTable 3.3: Gestational age of VLBW infants admitted to NNU 2014 – 2016SSWHG*N(%)(N 353)CUMHN(%)(N 259)STGH**N(%)(N 9)UHKN(%)(N 23)UHWN(%)(N 65)22 – 23 613 (3.7)12 (4.6)1 (11.1)0 (0)0 (0)24 – 26 679 (22.4)63 (24.3)2 (22.2)3 (13.0)11 (16.9)27 – 29 6130 (36.8)96 (37.1)0 (0)9 (39.1)25 (38.5)30 – 31 6100 (28.3)68 (26.3)2 (22.2)4 (17.4)26 (40.0) 3231 (8.8)20 (7.7)1 (11.1)7 (30.4)3 (4.6)*Note 3 cases missing for 2014 Data **2014 Data unavailable for STGHTable 3.4: Birthweight of VLBW infants admitted to NNU 2014 – 2016SSWHG*N(%)(N 353)CUMHN(%)(N 259) 5016 (1.7)6 (2.3)501 – 75057 (16.1)751 – 1000STGH**N(%)(N 9)UHKN(%)(N 23)UHWN(%)(N 65)0 (0)0 (0)0 (0)49 (18.9)3 (33.3)1 (4.3)4 (6.2)67 (19.0)53 (20.5)0 (0)4 (17.4)10 (15.4)1001 – 125085 (24.1)56 (21.6)1 (11.1)9 (39.1)19 (29.2)1251 – 1500138 (39.1)95 (36.7)2 (22.2)9 (39.1)32 (49.2)*Note 3 cases missing for 2014 Data **2014 Data unavailable for STGHTable 3.5: Additional clinical demographics of VLBW infants 2014 – orn32524361858Male19214241234Prenatal Care1808862363Chorioamnionitis98001Maternal Hypertension52271321Antenatal Steroids29821441961C-Section19112751643Antenatal Magnesium Sulphate1431012634Multiple Gestation58362317Congenital Malformation61041Small for Gestational Age411721012Measure*Note 3 cases missing for 2014 Data **2014 Data unavailable for STGH18
Maternity Services Annual Report 2016Table 3.6: Summarises respiratory support for VLBW infants 2014 – ubation in delivery suite1411005927Surfactant (in delivery suite)132905730Surfactant (at any time)21315461142Mechanical Ventilation19714661035High Frequency Ventilation5653003CPAP (at any time)27522131239Initial CPAP and subsequent intubation81540918Nitric Oxide3131000Intervention*Note 3 cases missing for 2014 Data **2014 Data unavailable for STGHTable 3.7: Major morbidities amongst VBLW infants admitted 2014 – UHK(23)UHW(65)Admission temperature 36 C53272915Pneumothorax1716100Oxygen at 28 days1531271520Oxygen at 36 weeks CGA9685038Postnatal steroid therapy3024006Home oxygen1814022Ibuprofen for PDA2921017PDA ligation55000NEC2118003NEC surgery87001Coagulase negative Staph. in blood culture22100111Fungal infection11000Grade 3 or 4 IVH2319013Cystic PVL42011Neurosurgery10001Retinopathy of prematurity (any stage)48342012Retinopathy Surgery1611104*Note 3 cases missing for 2014 Data **2014 Data unavailable for STGH19
South/South West Hospital GroupGynaecology Outpatient ActivityGeneral and specialist Gynaecology care is provided throughout the SSWHG. Clinicsare run at the four main hospital units as well as outreach clinics in different areas.The following clinics/services are provided in the SSWHG region; General Gynaecology & Telephone Follow UpUrogynaecologyGynaecological OncologyColposcopyPaediatric/Adolescent GynaecologyInfertilityAmbulatory GynaecologyPostmenopausal BleedingHereditary Gynaecological CancersPerinealPre-Operative AssessmentEndometriosisHysteroscopyPostmenopausal Bleeding ClinicContinence AdviceSmear ClinicsTable 4.0: Gynaecology Outpatient ActivityClinicsTotal Outpatient activityincl. Colposcopy ,041*CUMH figures include CUMH/SIVUH/Outreach **data was unavailable for STGHStaffTable 5.0: Overall SSWHG Staff NumbersOverall SSWHGConsultants*MidwivesNCHDsTotal .506726121613*includes Cons Ob/Gyn 12.5 WTE (17), Cons Neonatologists 420
Maternity Services Annual Report 2016Research andInnovationDepartment of Obstetrics and Gynaecology, UCCThe department is located on the fifth floor of Cork University Maternity Hospital. It provides formalundergraduate teaching to UCC medical students. The department also provides a unique postgraduateprogramme namely the MSc in Obstetrics and Gynaecology programme aimed at clinical trainees in thespecialty. The aim of the department is to lead the development of teaching and research in obstetricsand gynaecology in Ireland and to become a centre of excellence internationally. This academic agendais fully integrated with the delivery of clinical care in Cork University Maternity Hospital, thus providing ahigh quality academic service across a broad range of clinical, educational and research 1/2012Figure 1.2:Research Incomein the Departmentof Obstetrics ,21,00000,800000,600000,0000,40020* Does not includeincome from INFANT2010/201121
South/South West Hospital GroupThe National Perinatal Epidemiology Centre (NPEC)The National PerinatalEpidemiology Centre (NPEC)collaborates with Ireland’smaternity services to translateclinical audit data andepidemiological evidence intoimproved maternity care forfamilies in Ireland.The NPEC has a national focus,working in collaboration withall 19 of Irelands’ maternity andneonatal units: it reviews theirpractices in order to derive learningand make recommendations forimprovements in care based onthat learning.The NPEC has been collecting,analyzing and reporting onperinatal data since 2008.Publications Corcoran P, Manning E, O’Farrell IB, McKernan J, MeaneyS, Drummond L, de Foubert P, Greene RA, on behalf of thePerinatal Mortality Group. Perinatal Mortality in Ireland AnnualReport 2014. Cork: National Perinatal Epidemiology Centre, 2016. Manning E, Corcoran P, O’Farrell IB, de Foubert P, DrummondL, McKernan J, Meaney S, Greene RA, on behalf of the SevereMaternal Morbidity Group. Severe Maternal Morbidity in IrelandAnnual Report 2014. Cork: National Perinatal EpidemiologyCentre, 2016. Meaney S, Waldron M, Corcoran P, Greene RA, Sugrue S. PlannedHome Births in Ireland Annual Report 2014; HSE National HomeBirth Service provided by Self Employed Community Midwives.Cork: Health Service Executive, 2016. Twomey A, Murphy BP, Drummond L, Corcoran P, O’Farrell I,Greene RA, on behalf
The South/South West Hospital Group serves a population of over 800,000 people and every day more than 8,800 staff contribute to our results in care, cure, research and education. 2016 was the year that saw the continued development of the South/South West Hospital group as the corporate management entity over