Transcription
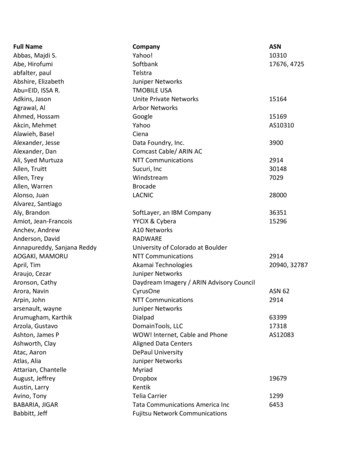
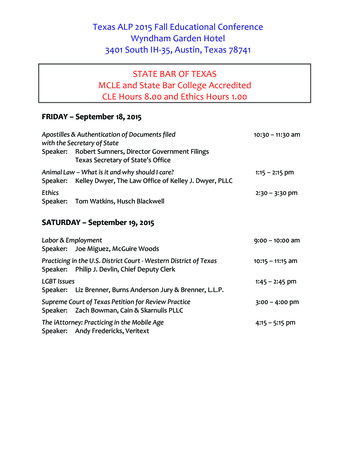
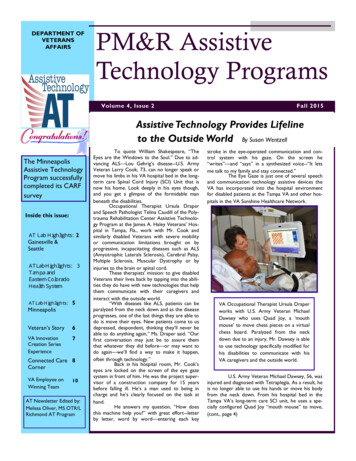
DEPARTMENT OFVETERANSAFFAIRSPM&R AssistiveTechnology ProgramsVolume 4, Issue 2Fall 2015Assistive Technology Provides Lifelineto the Outside World By Susan WentzellThe MinneapolisAssistive TechnologyProgram successfullycompleted its CARFsurveyInside this issue:AT Lab Highlights: 2Gainesville &Seattle3AT Lab Highlights:T ampa andEastern ColoradoHealth SystemAT Lab Highlights:5MinneapolisVeteran’s Story6VA InnovationCreation SeriesExperience7Connected Care 8CornerVA Employee onWinning Team10AT Newsletter Edited by:Melissa Oliver, MS OTR/LRichmond AT ProgramTo quote William Shakespeare, “TheEyes are the Windows to the Soul.” Due to advancing ALS—Lou Gehrig’s disease--U.S. ArmyVeteran Larry Cook, 73, can no longer speak ormove his limbs in his VA hospital bed in the longterm care Spinal Cord Injury (SCI) Unit that isnow his home. Look deeply in his eyes though,and you get a glimpse of the formidable manbeneath the disabilities.Occupational Therapist Ursula Draperand Speech Pathologist Telina Caudill of the Polytrauma Rehabilitation Center Assistive Technology Program at the James A. Haley Veterans’ Hospital in Tampa, Fla., work with Mr. Cook andsimilarly disabled Veterans with severe mobilityor communication limitations brought on byprogressive, incapacitating diseases such as ALS(Amyotrophic Laterals Sclerosis), Cerebral Palsy,Multiple Sclerosis, Muscular Dystrophy or byinjuries to the brain or spinal cord.These therapists’ mission: to give disabledVeterans their lives back by tapping into the abilities they do have with new technologies that helpthem communicate with their caregivers andinteract with the outside world.“With diseases like ALS, patients can beparalyzed from the neck down and as the diseaseprogresses, one of the last things they are able todo is move their eyes. New patients come to usdepressed, despondent, thinking they’ll never beable to do anything again,” Ms. Draper said. “Ourfirst conversation may just be to assure themthat whatever they did before—or may want todo again—we’ll find a way to make it happen,often through technology.”Back in his hospital room, Mr. Cook’seyes are locked on the screen of the eye gazesystem in front of him. He was the project supervisor of a construction company for 15 yearsbefore falling ill. He’s a man used to being incharge and he’s clearly focused on the task athand.He answers my question, “How doesthis machine help you?” with great effort--letterby letter, word by word—entering each keystroke in the eye-operated communication and control system with his gaze. On the screen he“writes”—and “says” in a synthesized voice--“It letsme talk to my family and stay connected.”The Eye Gaze is just one of several speechand communication technology assistive devices theVA has incorporated into the hospital environmentfor disabled patients at the Tampa VA and other hospitals in the VA Sunshine Healthcare Network.VA Occupational Therapist Ursula Draperworks with U.S. Army Veteran MichaelDawsey who uses Quad Joy, a ‘mouthmouse’ to move chess pieces on a virtualchess board. Paralyzed from the neckdown due to an injury, Mr. Dawsey is ableto use technology specifically modified forhis disabilities to communicate with hisVA caregivers and the outside world.U.S. Army Veteran Michael Dawsey, 56, wasinjured and diagnosed with Tetraplegia. As a result, heis no longer able to use his hands or move his bodyfrom the neck down. From his hospital bed in theTampa VA’s long-term care SCI unit, he uses a specially configured Quad Joy “mouth mouse” to move,(cont., page 4)
Page 2PM&R Assistive Technology ProgramsAT Lab Highlights.GainesvilleDuring the month ofSeptember, the GainesvilleSpeech Pathology staff hosted anAT Open House. Six vendorswere present and demonstratedaugmentative communicationdevices (AAC) and environmentalcontrols (ECU) for the hospitalbased home care, spinal cordinjury, and ALS teams. Socialwork, nursing, primary care physicians, neurologists, occupationaltherapists, and physical therapistsparticipated in the event andwere partnered with staff formthe Prosthetics Service to rotateto each room and to experiencehow a patient would utilize eachdevice. The Open House wasfollowed by interdisciplinary teammeetings to share thoughts regarding the best AT options forsessment and trial period withthe patients and their families.current homebound cases.For those disciplines familiarwith AAC and ECU it was achance to discuss newer devices and software available.For the medical and prosthetics staff it was an opportunityto learn about the range andcomplexity of devices availableand to better understand theimportance of a careful as-AT Lab Highlights SeattleSeattle is making greatprogress in developing our Assistive Technology Clinic. We extended our services to a clinic atthe American Lake campus inTacoma. The team there is led byWendy Woods (SLP) and MaryGraddon (OT).We presented at thePVA Summit in September, highlighting our success in 2 casepresentations.We hosted our firstannual Assistive Technology Fairto the Rehab Care Service line tointroduce therapists and providers to our services and technology tools.Two site visits from thenational AT leads from the University of Pittsburgh have energized our team and expanded ourknowledge. The first visit focusedon program development andwheeled mobility/seating and positioning, and the second focusedon AAC and computer access.The University of Pittsburgh teamoutfitted our AT clinic with atoolkit with very exciting optionsfor computer access. We are verygrateful their ongoing support andleadership.Three of our team members(Cathy Covey, Laura Hardy, andWendy Woods) are presenting atthe Washington Speech-LanguageHearing Association annual conference in October on how tobuild an interdisciplinary AT team,and another on a case study involving a patient with ALS whohas benefitted from this interdisciplinary approach.Upcoming goals includeexpanding services to other regions by sharing expertise withour collagues at the Spokane VAwho serve veterans in largely ruralareas of Eastern Washington,Eastern Oregon, and Idaho.We continue our campaign to educate providers and therapists aboutour services by reaching out toMental Health, Primary Care, andother services via Grand Rounds,brochures, and personal contact.We have 4 staff memberson our team who are currently/stillstudying for their ATP and intendon taking the exam by the end ofthe year: Cathy Covey, MOTR/L;Laura Hardy, MS, CCC-SLP, WendyWoods, MS, CCC-SLP and VirginiaKudritzki, DPT
Volume 4, Issue 2Page 3AT Lab Highlights.TampaACCOMPLISHMENTS AT was highlighted in a recent article including two patient storiesand the positive effects of technology within their lives. The articlewill be featured in the VISN 8VOICE e-newsletter, on the VISN 82015 Annual Report, on the VISN 8Internet site as well as the TampaVAMC Internet site. Tampa now has 7 RESNA ATPcertified clinicians AT was instrumental in the TampaSCI Program’s receipt of the Leader of Innovation Interactive PatientCare Award at the Get Well Network (GWN) Conference whichwas featured on the GWN, PVAand JAHVA Facebook pagesCOMMUNITY OUTREACH AT is presenting in collaborationwith colleagues at facilities withinVISN 8 for this month’s educationseries focused on clinical implications of telehealth AT has been selected to present atthe Assistive Technology IndustryAssociation (ATIA) Orlando 2015 AT has been selected to present atthe Association of Veterans AffairsSpeech Language(AVASLP) 2016Pathologists AT continually fields emails and phonecalls from clinicians nationwide re: variousAT questions and concernsPROFESSIONAL DEVELOPMENTAT coordinated an 8-hour seminarby Permobil for the rehab department to increase staff expertise andprovide for free CEU opportunities AT coordinated vendor demonstrations for the rehab department toinclude products such as Lingraphica,Autonome, and Hive Home Automation TELEHEALTH AND PROGRAMEXPANSION AT continues to provide CVT-Hm toincrease access to services with suchdata reflected within Speech and OTworkload. Additionally, AT assistswith access to CVT-Hm by installingJabber on mobile devices and trainingpatients and caregivers on the procedures for placing a video call. We have completed 6 E-consultsfrom within our facility and 24 VISN8 IFC E-consults We have completed 2 VISN 8 IFCCVT consults We have completed 1 VISN 8 IFCconsultAT Lab Highlights.Eastern Colorado Health Care SystemThe Eastern ColoradoHealthcare System Assistive Technology Program has put a strong emphasis on collaborating with the SCI-D/ALS program to identify early ATintervention. This has resulted inearlier evaluation and education forVeterans, stakeholders and community partners.ECHCS welcomed a newOccupational Therapist who is dedicated to the Assistive Technology/Wheelchair team and a new Speechand Language Pathologist to the ATteam as well. The hiring of new employees helps to fortify and recognizethe value of an outpatient interdisciplinary team of specialists.The second annual AT DeepDive was held in Denver, Colorado in May2015 and went off without a hitchthanks our partnership with the University of Pittsburgh RSTCE! Close to 20 individuals gained valuable hands-on experience with all facets of assistive technology,adaptive recreation, wheeled mobility andadaptive driving.
Page 4PM&R Assistive Technology ProgramsAssistive Technology Provides Lifeline to the Outside World , cont.chess pieces on a touch screen, adding to his enjoyment of playing virtual chess with people from as faraway as Italy and Saudi Arabia. Before using theQuad Joy, he hadn’t used a computer in years.At James A. Haley, this assistive technology is integrated into the GetWellNetwork (GWN),an in-room interactive patient care system thatoperates from a TV monitor at the patient’s bedside. Using his Quad Joy, Mr. Dawsey can “sip andpuff” to control his room lights, call a nurse, adjusthis bed and also send e-mail, surf the web, watchmovies and TV., listen to music, and of course, hisfavorite, to play video games.The GWN system is now in all hospitalsin the VA Sunshine Healthcare Network. Besidesproviding on-line entertainment and internet, the all-in-one system also gives patients customized healtheducation as well as information on hospital services, medications, patient safety and pain management right at their bedside.“We take communication for granted-greeting someone in the morning, telling someoneVA Speech-Language Pathologist Telina Caudill assistsU.S. Army Veteran Larry Cook at the James A. HaleyVeterans’ Hospital, long-term care Spinal Cord Injuryunit. Mr. Cook suffers from advanced ALS disease thathas left him paralyzed and without the use of his voice.To communicate with his caregivers and family, he useshis eyes to move the keys on the Eye Gaze, an eyeoperated communication and control system. This andother assistive technologies have opened the world toseverely disabled Veterans, providing new and alternative means to stay active and connected.you love them. But for these Veterans, it’s theirone and only way to communicate. Besides socialization, communicating their basic medicalneeds is really important when they’re in pain,need to be moved or have difficulty breathing.These devices are also very important to theVeteran and his family to communicate end-oflife desires,” explains Ms. Caudill.Sometimes people believe Veteranswith these kinds of severe disabilities are not‘there” anymore, according to Ms. Caudill.Nothing could be further from the truth, sheasserts. ALS, for example, does not affect aperson’s ability to see, smell, taste, hear or recognize touch. “These devices help a Veteran’spersonality show through. They are a lifeline forsome of our most severely disabled Veterans.”
Volume 4, Issue 2Page 5AT Lab Highlights Minneapolistherapy which may include structuredvisual, auditory, tactile, vestibular, olfactory, and taste stimulation. Patients aremonitored for responses to these stimuliboth informally by nursing and therapystaff and formally using standardizedmeasures such as the Disorders of Conscience Scale and Coma Recovery Scale –Revised. Treatment teams currently target therapy time for when patients appearto be more aware of the surroundings.Assistive Technology used with this population has included EEG and eyegaze controlled communication devices. Previouslyapplied technologies require patients tobe partially or fully emerged from comaso that the technology interface can becalibrated relative to the patient. ForRESNA CredentialingDr. Brian Fay received the E E GSeating & Mobility Specialist (SMS) credential from RESNA in April 2015. Dr.Fay serves as the Director of the Minneapolis VA Assistive Technology Program.The Minneapolis AssistiveTechnology Program received a fullthree year accreditation from CARFInternational.Patient EducationThe Minneapolis AT Programhas recruited a group of clinicians including OT, PT, SLP, MD, and SW tobegin a year-long effort to develop patient education resources regardingassistive technology commonly prescribed as part of rehabilitation programs for traumatic brain injury (TBI).These resources will be composed ofprint and online resources.Emerging Consciousness (EC) Program CollaborationPatients who incur a severe TBI andremain in coma are often enrolled in theEC Program at Minneapolis. These patients currently receive multisensoryrecognition to analyze the EEG of patients,EEG is collected during a restful state and during the currently applied multisensory therapyusing an Intendix amplifier (Cortech, Wilmington, NC). The data collection procedures toobtain these EEG recordings do not vary fromthose currently employed. These proceduresare non-invasive and involve the patient wearing a skull cap not unlike a shower cap. ThisEEG focuses on bilateral, bipolar, longitudinalmontages. The EEG recordings will be evaluated to determine whether the patient’s EEG isindicative of arousal in response to multisensory therapy.Eyegaze: Eyegaze tracking can now be donewithout the calibration routine previouslydescribed. Previous technologies were notworn by the patient, but mounted to a nearbycomputer. The new technology from SMIGmbH (Teltow, Germany) is embedded inglasses that are worn by the patient. Smallsensors in the glasses enable quantification ofpupil direction and cameras facing outwardfrom the glasses record head orientation.These measures allow quantification of eyegazeregardless of head or pupil position. Dataoutput can be viewed as the two-dimensionalpath of eye fixation and will be used to determine the degree of visual response to stimulacommunication devices, the patient mustbe able to interact with a display screen tion.by watching for a specific alpha characteras all alpha characters flash on the screen.In the case of eyegaze communicationdevices, the patient must be able to tracka 25mm dot with the eyes as it movesabout the screen. Both of these tasks arebeyond the typical patient who is in comaor a minimally conscious state.As part of a Quality Improvement (QI)Project, the EC treatment team is introducing new technology and methodswhen considering EEG and eyegaze systems with EC patients. These technologyand methods are more amenable toproviding the clinical staff with information about the alertness of the patientemerging from coma.EEG:Rather than employ character
Page 6PM&R Assistive Technology ProgramsVeteran’s Story Douglas VitaleMr. Douglas Vitale, a 28y/o retired Marine Sergeant,served as an infantry rifleman andleader of his squad. While leadinghis squad on foot patrol in the fallof 2011 in Afghanistan, Sgt. Vitalestepped on an IED. As a result ofthis, he suffered catastrophic injuries that included severe TBI,bilateral CVAs, bilateral above theknee amputations, right hemiparesis and neglect as well as left hemiballismus. A testament to his character, this Marine underwent extensive rehabilitation at the JamesA. Haley Veteran’s Hospital inTampa before transferring back tohis hometown of Pittsburgh in late2013. He continues his amazingrehabilitation journey at the VAPittsburgh Healthcare System withhis wife, Alexis, and service dog,Partner.In January of 2014, Mr.Vitale was introduced to his outpatient rehabilitation team, whichincluded Physiatry, PT, OT, SLP,and our PT specialist in mobility,among others. His initial goalsincluded increased sustained attention and endurance, improvement of attention to right visualfield, identification of a reliablefunctional communication system, and increased functional useof his upper extremities for tasksand recreational activities. Hebegan attention work and eyepointing with a plexi-glass boardwith speech pathology along withpassive and active range of motionand targeting activities with PT/OT.Six months into his outpatient therapy, Doug was practicing eye control and tracking with aTobiiDynavox i15 and beginningto specify preferences in simplefunctional page sets, limited to afield of 4 pictures and orientationof items on the left of the screen.He was sitting on the plinth withsupport from a therapy ball andtherapist to remain upright. BySeptember 2014, PT/OT utilizedthe Arjo MaxiSky 600 ceiling liftwith walking jacket allowing Dougto stand with his bilateral aboveknee prosthetics. Less thanthree months later, Doug, withmaximal team assistance, tookten steps.Now, four years afterhis catastrophic event, Doug isusing his i15 to practice resisting salient distractions andreduce perseveration in his leftvisual field while using it functionally for specification ofsome preferences such as themusic he would like to hear orthe exercises he would like tocomplete in PT/OT. His needfor cueing while using the device has decreased such that heis able to cross midline with hisHOW DO YOU FEEL ASSISTIVE TECHNOLOGY HASENHANCED DOUG’S RECOVERY?His wheelchair has providedhim the ability to practice functionaltasks, such as standing, before he hadthe opportunity to do it. His actiontrack chair gives him the chance toparticipate in outdoor activities withfriends and family, and the in-homeceiling lift now allows me to care forhim independently. Since we are ableto connect his Tobii to his chair, wecan use it in multiple places. His Tobiihas given him the ability to have somesay in his life we can know that hemeans certain things, not just assume.He was a poet prior to his injury andnow with use of the Tobii (and hispersonal page sets), is able to read/recite his work. You can see his pridewhen he “reads” his work and whenhe is able to stand on his legs. Theteam working together has enhancedhis interactions, strength, endurance,monitoring of his position in space, andpride.WHAT FUNCTIONAL IMPROVEMENTS HAVE YOUSEEN IN HIS DAILY INTERACTIONS AS A RESULT OFHIS REHABILITATION?gaze when provided with verbalencouragement or directionalcues in selection fields up to 16pictures/words. He is generalizing his skills to cue himself toorient right when salient stimuliare present. He is now able tostand, aided only by the ceilinglift, in the parallel bars for up to30 minutes, benefitting fromencouragement and some assistance with repositioning after 5minutes.As Doug remains non-verbal, I asked a key memberof his rehabilitation team, hiswife Alexis, a few questionsabout how assistive technologyhas impacted their lives.Doug’s attention is longer.He is able to engage with everyone(regardless of where they are in theroom) and be a part of the conversations. He responds (with facial expression) and his moods are great! When Iwake up in the morning, he is staringat me, and I’m on his right! He neverused to do that!As with any case of someone who has suffered severe braininjury, Doug has good days and bad,but he is able to shake it off, comingback better each time. The character and determination of this DevilDog challenges us, as therapists, tothink outside the box and each daybring our best to the veterans weserve. As for the progress Dougcan make, I suspect that it is onlyin our wildest dreams.
Volume 4, Issue 2Page 7Live Changing Event impacting Veterans andthe Community as a Whole Melissa Oliver, MS OTR/LOn July 28-29, 2015 at McGuire VA Medical Center inRichmond, Virginia, the Assistive Technology Program partneredwith the VA Office of Innovation to bring together innovators inventors problem solvers to create solutions for challengesour Veterans face every day. I could not have imagined the lasting impact the VA Innovation Challenge Make-A-Thon wouldhave on all of those involved.The Make-A-Thon began with several Veterans sharingtheir challenges through Their story Veteran Eric Young had the participants envision a roadrunning through the mountains of Colorado and how itwould feel as you drove your motorcycle down that road then imagine not being able to do it because of the loss ofyour arm. Mr. Young, “I want and I will ride my motorcycleon that road through the mountains of Colorado.”Veteran Kim Matthews spoke about how everyday thingsthat women do to get ready in the morning are taken forgranted but is a challenge for her because of her hand tremors. The tremors make it more difficult to put on make-up,fix her hair and button her blouse to the point that she doesnot go out as much anymore. It is isolating.These are a just a few of the stories that were sharedwhich touched participants so much that those that came asspectators decided to jump in and attempt to solve the problemand others who came as participants it added to the inspiration.We had about a dozen challenges that needsolutions.21 teams formed with 1 focus tocreate the solution for that individual whichwould impact their quality of life. What aPowerful Mission?! The synergy in theroom as the team emerged and ideas weredeveloping was so intense that it is difficultto describe other than to say it like the“Energizer Bunny times 1,000.” Teamsrange in age to expertise with a team member being 10 years old to a team member with 30 years of professional expertise in engineering. The diversity on the teamsand the collaboration was incredible as they worked towardsthat one goal.Teams were problem solving, mentors were guiding,veterans were consultingand prototypes were printing. And the expertise inthe room was AMAZING mentors fromToyota, GE, 3D Systems,Stratasys, CAD programexperts, the AssistiveTechnology Program,McGuire VA Medical Center’stherapy and prosthetics staff, software engineers and physicians.The designs were thensent to one of the fourteen 3DPrinters for the prototypes toprint overnight – you could hearthe humming of the machines asthey worked hard to create thedifferent teams’ visions turningthem into possible solutions.Day 2 brought just asmuch energy if not more, as theteams’ only had a few hours tofinalize their creations it was arush to the very last minute with team members running aroundtrying to find tools, consult with mentor and create the finalpresentation.As part of the judging criteria, all of the teams had toupload their designs to the NIH 3D Print Exchange where thedesigns are open source meaning that anyone, Veteran or nonVeteran, would have access to their designs that could potentialimpact their everyday which in turnsimprovestheirquality of life.How Cool is that!The Make-A-Thonnot only changedour Veterans’ livesbut the public as awhole.Now itwas time for the teams to present their solutions in 3 minutes talk about time crutch. I was not presenting but I could feel thepressure to say everything they wanted and showcase their design in such a short amount of time. After 21 presentations andalmost 2 hours, the judges had the Huge Undertaking of decidingthe ultimate winning design.And the winner is, drum roll please Team Spline withtheir coupler design for Veteran LisaMarie Wiley who lost her leg belowthe knee from a bomb blast. Theywon 20,000 from Google.com. Therewere six other winners of prize money as well.Everyone’s lives were impacted and changed. There is nothingmore I can say but Thank you to everyone involved.“Thank you forthisopportunity”- A Participant
Page 8PM&R Assistive Technology ProgramsConnected Care CornerAs technology has continued togrow and expand for assistive technology,so have the options for connecting withour veterans, their families/caregivers, andfellow VA staff. The “Connected CareCorner” will be a series of articles describing ways to utilize technology toassure a smooth continuum of care forsome of our most complex cases. ThisAT Lab issue will focus on a case utilizingvideo conferencing and clinical video telehealth tools for a dependent in a ruralsetting.The Speech Pathology Clinicreceived a consultation to evaluate a veteran’s daughter (dependent) for an augmentative communication device. The 38year old female presented with severespastic dysarthria and moderate cognitivecommunication problems secondary toanoxia at birth. She had had speech pathology and occupational therapy servicesduring her elementary, junior and seniorhigh school years but, no further treatment or technology options have beenexplored during the past 20 years. Thedependent lives at home with her mother.The mother has physical limitations dueto progressive visual losses and a recenthip fracture. The father, a career Airforce pilot, had passed away approximately six months ago and the mother wasvery concerned about her daughter’sability to communicate in the event shemay not be available. The Social Workerthought that the dependent would benefitfrom a device to assist with communication. The dependent and the mother live2 ½ hours away from the closest VAmedical center and 20 minutes from theclosest community outpatient clinic(CBOC). The mother did not drive andbecause the dependent was not eligiblefor travel pay, they relied upon friends toprovide transportation.The PrimaryCare Team requested that services beprovided during a Telehealth visit.Pat Ryan, retired Assistant Director, Office of Telehealth, taught usnot to focus on the telehealth technologyavailable but, to clearly define “Who,What, When, Where, and Why” youwant to utilize the telehealth technology.After defining the task you want to do,then select the appropriate telehealth forvisit. This has been a guiding principle fordevelopment of many telehealth pro-grams. Here is an example of how theinterdisciplinary team answered questions for the teleconsultation and follow-up home telehealth visit.Who will be involved in the teleconsultation?1. 38 yr. old female, severe dysarthriawith cognitive deficits2. mother3. and don’t forget the staff at theCBOC (telepresenter, nurse, primary care)4. vendors (at least 2 vendors to trialdevices)What do you want to accomplish duringthe visits?1. Interdisciplinary meeting and education for the CBOC staff prior tothe teleconsultation2. interview with the mother3. teleconsultation visit (2 hours) a)clinical exam and b) trial with devices including vendors4. home visitWhen do you want to complete the visit(s)? Interdisciplinary team meeting withthe CBOC staff followed by aninterview with the mother/daughter within the next twoweeks (Note: 1 hour time difference between the medical centerand the CBOC) Teleconsultation within two weeksafter the interview. Note: dependent, mother, telepresenter, andvendor(s) will need to be in theroom. Home visit for assessment andfollow-up to be determined afterthe interview and purchase of adevice.Where do you want to complete the visit(s)? CBOC Dependent’s homeWhy or what is the purpose of telehealthvisits?To select assistive technology,communication device, in the absenceof a caregiver and for independence andto provide follow.Then review possible telephone or telehealth options for visits.Utilize the same principles for selecting thebest assistive technology for a patient. Consider the advantages and disadvantages foreach option. Don’t forget the FacilityTelehealth Coordinator will play an vitalrole in assisting in the selection of the telehealth equipment, knowledge about theequipment at each OPC, CBOC, and Medical Center, and capturing workload. Thelink to locate your local Facility gov/roles/ftc/index.asp,Telehealth Services home page is http://vaww.telehealth.va.gov/, the link to thetelehealth documents is /Forms/AllItems.aspx, and the link for /clinic/index.asp.In this case, the team decided toutilize 3 of the VA telehealth options. Initially the AT Lab specialist clinician completed a videoconference with the CBOC staffto review plans for the Teleconsultationand to describe the equipment and suppliesthe clinician would be sending for the visitwith the dependent. In addition, discussedplans for two vendors to come to theCBOC with equipment. The videoconferencing system was also utilized for the initial interdisciplinary team meeting to interview the mother and to determine thegoals for the Teleconsultation. The education cart with the document reader andexam camera was moved to the conferenceroom to allow for greater space for thedevices, vendor, and mother to be presentin the room during the evaluation. Finally,the TES unit was utilized twice in homeonce with the interdisciplinary team couldassure the equipment was set up properlyand once to follow-up with dependent andmother to assure they understood how touse the communication device.
Volume 4, Issue 2Page 9Technology ConsideredPlain old telephone (POTS)ConsiderationsLand line in the homeVideophone to POTSPatient may purchase for use in thehome.Mobile telephoneMother has a mobile phone, androidwith a limited data plan, and doescurrently utilize any apps.Patient Device/Jabber Software (CVTHm)(Dependent/Mother Computer)Old desktop apple computer in thehome, no webcam, no high speedinternetVideoconferencing at the CBOCLink for more ehab/trehb/index.aspCBOC has one medium sizeconfer
Eastern Colorado Health System 3 . Minneapolis progresses, one of . 5 . Veteran's Story. 6 . VA Innovation Creation Series Experience do . 7 Corner 8 . VA Employee on Winning Team . 10 . AT Newsletter Edited by: Tampa VA's long Melissa Oliver, MS OTR/L Richmond AT Program . Assistive Technology Provides Lifeline to the Outside World