Transcription
ORIENTATION TO THEGI UNITS FOR THEANESTHESIAPROVIDERA survival guide for working in the GI units at BIDMCEswar SundarDirector ofClinicalAnesthesia-East
Welcome to the largest gastroenterology unit in the nation! On average about 120 GIprocedures are performed across the four locations in BIDMC every day. About half ofthem with an anesthesia provider! I am hopeful that this manual will help younavigate your day in the GI units.The GI UnitsBIDMC has 4 GI units. GI3 or ST3 is located in the East campus Stoneman building, on the third floor. It is on thesame floor as the Feldberg ORs . In GI3 almost all the cases are upper endoscopies orcolonoscopies. No advanced endoscopies are performed in the GI3 suite. Two procedural roomsin GI3 are devoted to anesthesia cases. Moderate sedation cases also go on in other roomswithout anesthesia involvement. GI4 or ST4 is also located in the East campus Stoneman building. It’s directly above the ST3(GI3) unit. GI4 can be accessed by walking through the double doors next to the AnesthesiaOffices on the 4th floor. GI4 is the unit that performs most of the advanced endoscopiesincluding, ERCP, Single Balloon Enteroscopies (SBE), Endoscopic Ultrasound (EUS), esophagealand colonic stent placements, radiofrequency ablation and cryoablation of esophageal dysplasiaand Obera (Intragastric balloons for weight loss) placement and removal. Simple EGD andcolonoscopies are also performed on patients deemed “high-risk.” Moderate sedation cases arerarely performed in GI4 because of the nature of procedures. West Procedural Center (WPC). This unit is located on the West campus on thefirst floor of the Farr Building. There are two procedural rooms in the WPC, with onepredominantly used by anesthesia. Upper endoscopies, colonoscopies and EUS procedures aredone in the WPC. Moderate sedation cases also simultaneously go on in other rooms. Harvard Vanguard Medical Associates at Kenmore (HVMA). This is anoffsite location in Kenmore square. It’s walking distance from the main campus, but you canalso drive there and park at a nearby garage. Cases are composed of EGDs, colonoscopies, andendo-colons. Patients are generally healthy, and turnover is pretty rapid. There is no facility forGAs at HVMA.We shall address the workflow in each of these units separately.NOVEMBER 30, 20201
GI3Start TimesGI3 units start cases at the following times. Please page the floor manager for all issues that lead todelays.Start 09:007:307:30PM12:307:3012:30There are two procedural rooms in GI3. Looking out from the nurses counter down the corridor, thefirst room on the right is Rm1 and the one on the left is Rm2. On most days there are separateendoscopist lists for the morning and afternoon. Usually solo anesthesia attendings are posted in theserooms.Harvard Vanguard or Atrius endoscopists are usually assigned Rm2, while other BIDMC endoscopists arein Rm1.Patient preparationPlease check the machine and other critical equipmentbefore the start of the day. Anesthesia tech support can berequested by paging 30951 (Anesthesia Tech East Remote).Patients are listed on the “Anesthesia” white board withthe bay number in which they are situated. A nursepractitioner is usually available in the holding area to do ahistory and physical, while a GI nurse places an IV. Theanesthesia provider is required to review the H&P printoutor on the lap top screen in AIMS and make amendments asneeded. A BP cuff is usually placed on the patient’s arm in the holding area. Sometimes nursing mightrequest MAC for a patient originally booked under moderate sedation. The GI resource nurse will talk toan endoscopist and make room/time for that patient.The anesthesia provider gets consent and moves the patient into the procedure room. Sometimes theendoscopists will get the consent in the room. In all cases, please ensure that all consents are signedbefore sedation is initiated.Anesthesia in GI3Please see section under Anesthesia for GI procedures for general guidelines.Specific to GI3, procedures are generally limited to EGD, colonoscopy or a combined EGD/colonoscopy.Sometimes cardiology may perform TEEs as an add-on procedure in the afternoon.NOVEMBER 30, 20202
A TALIS computer terminal, anesthesia machine, monitors,and an omnicell are present in both rooms. The GI nurse whois present with you during the procedure can help put themonitoring leads and BP cuff on. All equipment, includingnasal cannulas, is available inside the correspondingOmnicell drawer.Endoscopies are done with the patient’s head orientedtowards the door, while colonoscopies are done with thehead of the stretcher away from the door. If it’s an endocolon, you can detach the monitoring brick and rotate thestretcher for the colonoscopy. Almost invariably most patient’s get MAC anesthesia in GI3. Occasionalpatients will require either planned or unplanned general anesthesia.Optimally, patients should be arousable as soon as possible after completion of the procedure.Discharge within 30 min of arrival to the recovery room is part of the anesthesia care goals. The BP cuffshould be left on the arm as it will be used in the recovery room. Please continue to administer oxygenwhile transporting to the recovery area.RecoveryThe GI nurse will accompany you to the recovery area and help reestablish monitoring. Please ensurethat the patient is stable and arousable before leaving the patient to go to the designated AIMS laptopto open and print the case record.A brief handoff to the recovery nurse must include drugs administered and any anesthetic issues orconcerns. If appropriate, please complete the post anesthesia paper note before leaving the patient.You can walk back to the holding area to see your next patient. If a patient has had a GA, the patientwill need to be transported to the Feldberg PACU with the GI nurse. Please remember to call aheadbefore leaving the room to book a bay.NOVEMBER 30, 20203
GI4Start TimesGI 4 units start cases on the following times.Start :457:307:30There are 2 rooms (ERCP1 and ERCP2) that have fluroscopic capabilities and one room that does not(EUS Room). These rooms may be staffed by 3 solo anesthesia attendings, one attending supervisingthree CRNA’s, or two attendings with one covering two residents.It is important that at least one anesthesia attending sits in at rounds with the GI physicians and fellowsat 7:00 to discuss the patients for the day. Please be ready to add any anesthesia concerns on anypatient, especially the ones that might need GA or need ICU care. Other providers can set up rooms andsee patients. An anesthesia tech is available on pager 30951 (Anesthesia Tech East Remote). Pleaseensure the suction tubing reaches the patient and a small suction tip is available.As previously noted, the GI4 suite performs a wide variety of endoscopic procedures. (Next section.)Patient preparationPatient’s going into your room (EUS, ERCP1, or ERCP2) will be posted on the white board, along with thebay they are in. Drugs are available in the Omnicell in the room and in the large Omnicell in the holdingarea for less frequently used drugs.A nurse practitioner is usually available in the holding area todo a history and physical, while a GI nurse places an IV. Theanesthesia provider is required to review the H&P printout oron the laptop screen in AIMS, make amendments as needed,and obtain consent. A BP cuff is usually placed on thepatient’s arm in the holding area. The anesthesia providermoves the patient into the procedure room. Sometimes theendoscopists will get the consent in the room, so pleaseensure that all consents are signed before sedation is initiated.GI4 procedures and default anesthesiaPlease see section under Anesthesia for GI procedures.Please ensure that all lines and cables can reach the patient. Our GI 4 unit is a referral center for some ofthe sickest patients from around the state requiring an advanced endoscopic procedure. Obesity,smoking, OSA, cholangitis, bowel obstructions, as well as a host of other significant comorbidities andfailed sedation are typical for patients in this unit. Despite these issues most patients do well with MAC.NOVEMBER 30, 20204
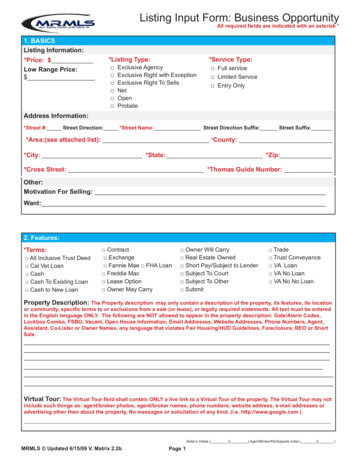
Listed below are the common GI procedures, the type of anesthesia and typical patient position.However, always use your clinical judgment and/or discuss with your colleagues, if you feel a patient’sneeds may be better served by an alternate form of anesthesia. Please always ask the GI nurse with youwhere the patient is going to be, in what position, or if GA is required. Most CRNAs and anesthesiaattendings with you are pretty experienced and will be able to guide you through the position andanesthetic RMACStretcherLeft lateralEUSMACStretcherLeft lateralColonoscopy/EMRMACStretcherLeft lateralERCPMACFluro tableProneSPYMACFluro tableProneSBEMACStretcher or FlurotableLeft LateralSBE ERCPMAC or GAFluro tableProneDuodenal oresophageal StentMAC or GAFluro tableLeft lateralColonic StentMACFluro tableLeft lateral, but headwill be away from theanesthesia machine!CryotherapyMACStretcherLeft lateralRF ablationMACStretcherLeft lateralObera placementMACStretcherLeft lateralObera removalGAStretcherLeft lateralPEGMACStretcherSupineF IGURE 1 ANESTHESIA TYPE, PLACE AND POSITION FOR ADVANCED ENDOSCOPIC PROCEDURESNOVEMBER 30, 20205
RecoveryAs in the operating room, please direct and help prone patients to roll over back on to the stretcher.Ideally, at the end of the procedure, the patient should be arousable. Among our anesthetic goals is theability to discharge patients within 30 min. of arrival to the recovery room. Please leave the BP cuff onthe arm, it will be used in the recovery room. Please administer oxygen while transporting to therecovery area.The GI nurse will accompany you to the recovery areaand help reestablish monitoring. Please ensure that thepatient is arousable and stable before leaving thepatient to go to the designated AIMS laptop to openand print the case record.A brief handoff to the recovery nurse must includedrugs administered and any anesthetic issues. Ifappropriate, please complete the post anesthesia papernote before leaving the patient.You can walk back to the holding area side to see yournext patient. If a patient has had a GA, the patient will need to be transported to the Feldberg PACUwith the GI nurse. Please remember to call ahead before leaving the room to book a bay.NOVEMBER 30, 20206
WPCStart TimesStart :458:007:30Patient preparationPlease check the machine and other critical equipmentbefore the start of the day. Please ensure the suctiontubing reaches the patient and a small suction tip isavailable. Anesthesia tech support can be requested bypaging 30950 (Anesthesia Tech West Remote).Patients are listed on the white board with the bay numberin which they are situated. A nurse practitioner is usuallyavailable in the holding area to do a history and physical,while a GI nurse places an IV. The anesthesia provider isrequired to review the H&P printout or on the laptopscreen in AIMS, and make amendments as needed. Sometimes nursing might request MAC for a patientinadvertently booked under moderate sedation. The GI resource nurse will talk to an endoscopist andmake room/time for that patient.The anesthesia provider gets consent and moves the patient into the procedure room. Sometimes theendoscopists will get the consent in the room, so please ensure that all consents are signed beforesedation starts.Unlike the other GI units the patient is moved to the procedural room by taking the entire monitoringbrick with the patient and reestablishing monitoring in the procedure room by inserting the brick intothe rack.AnesthesiaPlease see section under Anesthesia for GI procedures.EGD, colonoscopies, endocolon, EUS and PEG placementsare common procedures done in WPC. See table under GI4for positioning and anesthesia.A TALIS computer terminal along with anesthesia machinemonitors and an omnicell are available. The GI nurse who ispresent with you during the procedure can help put themonitoring leads on. Nasal cannulas and other equipmentare available inside the Omnicell.Endoscopies are done with the head away from the door,while colonoscopies are done with the head of the stretcher towards the door. If it’s an endocolon, youNOVEMBER 30, 20207
can detach the monitoring brick and rotate the stretcher for the colonoscopy. Almost invariably mostpatient’s get MAC anesthesia in WPC.Ideally, at the end of the procedure, the patient should be arousable. One of the anesthetic goals is tohave patients ready for discharge within 30 min of arrival to the recovery room. Please detach themonitoring brick and take it with the patient back to the same bay they came from. Please administeroxygen while transporting to the recovery area.RecoveryA brief handoff to the recovery nurse must include drugsadministered and any anesthetic issues. If appropriate, pleasecomplete the post anesthesia paper note before leaving thepatient.If a patient has had a GA, the patient will need to be transportedto the West PACU on the 5th floor of the Rosenberg building withthe GI nurse. Please remember to call ahead before leaving theroom to book a bay.NOVEMBER 30, 20208
HVMA at KenmoreHVMA is located off-site near Fenway Park. HVMA is walking distance from the hospital, although youcould drive and park at a designated garage. If you do park there, please remember to get your ticketvalidated, as otherwise it gets expensive!Anesthesia care is provided a few days a week.You will need to be credentialed separately atHVMA to work there. If you are assigned toHVMA please email Mary Ann Vann for moreinformation as to how things work out there.Most cases are EGDs and colonoscopies onrelatively healthy patients. There is no facilityto perform planned GA cases at HVMA.Propofol is the predominant drug used there.Cases are done with rapid turnover andeveryone usually breaks for lunch beforestarting an afternoon list. There are plenty ofrestaurants around!NOVEMBER 30, 20209
MAC anesthesia for GI proceduresMany excellent anesthesiologists and CRNAs perform great MACs on complicated patients using justPropofol. So timing and understanding the stages of a GI procedure are important.InsertionStabilizationCannulationRemoval For Upper GI procedures, this is often the most stimulating time. Patients may need a slight jawthrust to allow a large EUS or ERCP scope to enter. Insertion is complete when the scope reaches20 cm and the sedation level can then be reduced. For colonoscopy, insertion is also very stimulating and requires more sedation. Abdominal pressuremay be applied by nurses and may cause discommfort. Insertion is complete when thecaecum/ileocaecal valve is visualized. For EUS, SBE and ERCP procedures, the scope has to be maneuvered to a location tovisualize the ampulla or the head of the pancreas. This phase still requires some deepsedation though not as much as insertion. This is the process of getting a guide wire up the bile duct during ERCP and oftenis thelongest part of the procedure. Once the scope is in a stable position, sedation levels canbe decreased, as this phase is not very stimulating. However occasionally a patient canget bradycardic during balloon dilatation of the duct. Removal is lengthy during colonoscopy and sedation levels can be trimmed down as it'sgenerally not stimulating. At about 30-40 cm the scope has usually reached the sigmoidcolon and sedation can be turned off. Removal is also prolonged during SBE proceduresand not stimulating. For most upper GI procedure removal is quick and sedation may be stopped at that point.It’s not our intention to teach you how to do a MAC. However below is the list of some of the commondrug combinations, which anesthesiologists use.At BIDMC, routine spraying of the oropharynx with Benzocaine spray does not occur as it is consideredunnecessary for patients receiving deep sedation, leaves the patient with residual anesthesia, and canbe associated with methemoglobinemia in susceptible individuals. As providing sedation is the primaryobjective and painful stimuli are limited and transient, opioids are rarely used. Other drugs that may beneeded during the procedure are mainly to stabilize hemodynamics (labetalol, phenylephrine,ephedrine, glycopyrolate, etc.). Often during ERCP procedures, the endoscopists may request 0.2 mg ofglucagon IV. The GI nurses usually administer this. Glucagon helps with smooth muscle relaxation andNOVEMBER 30, 202010
reduces peristalsis. Antiemetics, NSAIDS, and opioids are not routinely given for GI procedures but maybe indicated in certain situations. Many patients after an ERCP who are at high risk for pancreatitis mayget an indomethacin suppository at the end of the procedure.Main drugPremed/adjuvantAdjuvantPropofol onlyPropofolMidazolam (1-2 mg)PropofolMidazolam (1-2 mg)PropofolKetamine 10-20 mg)Dexmedetomidine bolusWe are proud of our excellent expertise in GI anesthesia! Our GI docs and anesthesia group attract themost complicated and sick patients. Years of experience with MAC in this population has helped usprovide a safe and efficient service.For more information please contact Dr. Soumya Mahapatra. Director of GI Anesthesia.Let us know how we can improve this document and what other information may be useful to you!NOVEMBER 30, 202011
before the start of the day. Anesthesia tech support can be requested by paging 30951 (Anesthesia Tech East Remote). Patients are listed on the "Anesthesia" white board with the bay number in which they are situated. A nurse practitioner is usually available in the holding area to do a history and physical, while a GI nurse places an IV. The