Transcription
SCENARIO GUIDEBOOK
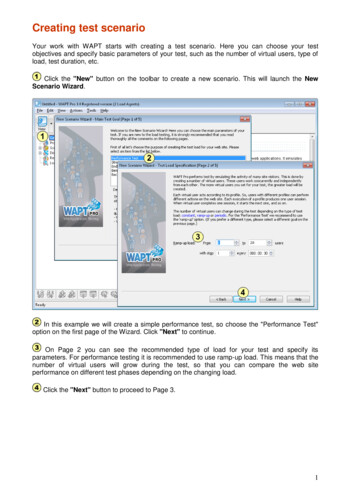
April 4, 2018Dear EMS Service Director and/or EMS Medical Director,In the summer of 2017, all Emergency Medical Services (EMS) agencies in Kansas completedthe National Emergency Medical Services for Children (EMSC) Data Analysis Resource Center(NEDARC) 2017-18 EMS Performance Measure Assessment. When assessed on EMSCperformance measure EMSC03; use of pediatric-specific equipment and how often providers withinyour service are required to demonstrate skills in a skill station, simulated event and/or fieldencounter, data collected showed room for improvement. These results can be found atwww.kdheks.gov/emsc under the EMS Survey tab. The Kansas EMSC program reached out toservices across the state regarding pediatric education and training. Those comments determined theneed for a resource to guide agencies and educators on pediatric call types.Along with members from the EMSC EMS Committee and pediatric advocates throughout thestate, the Kansas Pediatric Scenario Guidebook was developed. This resource will walk yourproviders through a scenario containing vital signs, pertinent patient and call information, graphics,considerations and links for additional educational opportunities surrounding that call type. The hopeis that this guidebook will encourage additional trainings and educational opportunities on pediatricsthroughout the year, while also increasing provider confidence when treating pediatric patients.The Kansas EMSC program is interested in your comments on the guidebook and look forwardto seeing an increase on pediatric training within your service. If you have any questions or needfurther guidance, please do not hesitate to contact the Kansas EMSC program!Tracy Cleary, CoordinatorKansas - Emergency Medical Services for ChildrenKansas Dept. of Health & Environment300 West Douglas Suite 700Wichita, Kansas 67202phone:316.337.6050cell: 785.213.1454tracy.cleary@ks.gov
INDEXMEDICAL . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Pages 5 – 27Accidental Overdose, 2-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 – 7Seizure, Febrile, 15-month-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8 – 9Seizure, Epilepsy, 4-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 – 11Diabetic, 15-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12 – 13Abdominal Pain, 14-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14 – 15Cardiac, 3-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16 – 17Sepsis, 2-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18 – 19Sepsis, PICC Line Infection, 15-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20 – 21Sudden Infant Death Syndrome (SIDS), 5-month-old . . . . . . . . . . . . . . . . . . . . . . . . . 22 – 23Code Blue, 3-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24 – 25Code Blue, 11-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26 – 27RESPIRATORY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Pages 29 – 39Asthma, 10-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30 – 31Croup, 4-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32 – 33Bronchitis, 9-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34 – 35Epiglottitis, 6-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 36 – 37Tracheostomy, 2-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38 – 39TRAUMA . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Pages 41 – 60Child Abuse, 2-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42 – 43Motor Vehicle Crash, 4-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44 – 45Near Drowning, 4-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46 – 47Burns, Smoke Inhalation, 16-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 48 – 49Burns, Accidental Scalding, 3-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50 – 51MV vs Pedestrian, 4-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52 – 53Abdominal Injuries, 10-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54 – 55Gun Shot Wound, 14-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56 – 57Hanging, Code Blue, 14-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 58 – 59Kansas Trauma Center Locations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 60-3-
INDEX, continuedCOMMUNICATIONS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Pages 61 – 68Language Barrier, 5-year-old . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 62 – 63Kansas EMSC EMS Communication Cards . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 64 – 68PEDIATRIC SAFE TRANSPORT. . . . . . . . . . . . . . . . . . . . . . . Pages 69 – 79NASEMSO Safe Transport of Children by EMS: Interim Guidance . . . . . . . . . . . . . . . 70 – 71Safe Transport, Uninjured/Not Ill . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 72 – 73Safe Transport, Ill/Injured but Requiring No Intensive Interventions/Monitoring. . 74 – 75Safe Transport, Ill/Injured Requiring Intensive Interventions/Monitoring. . . . . . . . . 76 – 77Safe Transport, Requiring Spinal Immobilization or Supine Transport . . . . . . . . . . . . . . . 78Safe Transport, Multiple Patients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 79ACKNOWLEDEMENTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Page 81This project is/was supported by the Health Resources and Services Administration(HRSA) of the U.S. Department of Health and Human Services (HHS) under grantnumber H33MC06726 Emergency Medical Services for Children. This information orcontent and conclusions are those of the author and should not be construed as theofficial position or policy of, nor should any endorsements be inferred by HRSA, HHS orthe U.S. Government.-4-
-5-
ACCIDENTAL OVERDOSEGoals/Objectives:Dispatch Information:A call was received from a frantic adult stating that her 2-year-old granddaughter Scene safetywas unresponsive on the bedroom floor. Patient is breathing, but not currently alert. Assess and secure airway Recognition and treatment forunresponsive state Recognition of transport necessity Chief Complaint:Additional Resources Requested:UnresponsivePolice and Fire Departments, ALSScene Description: Arrive at address and notice an older gentleman waving at you from the porch Home is clean, tidy and no animals are noted to be present. You are escorted to a basement bedroom The patient is lying on the carpeted floor with an older woman at her side. Woman identifies self as patient’s grandma Patient was reportedly nappingInitial Impression: Patient is dressed appropriately for time of year. You notice a pill bottle under the bed.Vital Sign – Set 1Physical ExamHPI: Patient has been puttingAVPU: Unresponsiveeverything in their mouth latelyHEENT:B/P: 80/palpationHead: No trauma notedS/S: UnresponsiveHR: 70, regularEyes: Sluggish and pinpointResp: 10, laboredEars: UnremarkableAllergies: NKDAO2 Sat: 90% (room air)Nose: UnremarkablePain:Oral Cavity: Lips noted to have white Medications: Daily VitaminGCS: 3 (1,1,1)substance on them. Half of a white pill isPmHx: RSV at 1 year of ageBGL:noted in the patient’s mouthVital Sign – (prior to Naloxone)Last Meal: Pizza and chips for lunchAVPU: UnresponsiveChest:B/P: 82/64Equal chest rise and fall notedEvents Prior: Napping in bedroom.HR: 78, regularClear equal in all lung fieldsWas checked on an hour previousResp: 10, laboredand was asleep in the bedO2 Sat: 94% (O2 applied)Back:No external trauma notedPain:Current on Immunizations? YesGCS: 3 (1,1,1)Abdomen/Pelvis:Patient Weight: 12kgsBGL: 84 mg/dlUnremarkableVital Sign – (after Naloxone)Notes:Grandmother advises that she wasAVPU: Alert, ConfusedExtremity:caring for a friend last week that hadB/P: 100/60Noexternaltraumanotedknee surgery. Her friend stayed in thisHR: 110, regularroom and was taking Lortab for post opResp: 18, nonlaboredOther:pain reliefO2 Sat: 98%Skin: Cool, pale and dryPain: 0Pill bottle found is for Lortab 7.5mLGCS: 14 (4,4,6)EKG: Sinus RhythmBGL:Suggested Treatment:Transport Consideration:After Naloxone administration:O2, Suction if necessary, Monitor,IV/IO, Administration of Naloxone Patient can maintain own airway Respirations return within normal limits Patient remain tired, Pupils now PERL-6-Secure patient properly on cotTransport in seated position secondaryto possible vomiting
ACCIDENTAL OVERDOSEAdditional Things to Consider about the Scene: Possibly have grandma call friend and inquire about number of pills missing Family centered careAdditional Things to Consider during Treatment/Transport: If dealing with an unknown medication, contact the Poison Control Center When administering Naxolone, it is a slow push and titrated to desired effect Keep back of ambulance lighting/temperature appropriate for patient comfort, low stimulation Transport to the nearest appropriate facility Contact patient’s legal guardian, if possibleAdditional Educational Resources to Consider: Poison Control Centero https://www.poison.org Kansas Poison Control Centero s/poison-controlThe University of Kansas Hospital Poison Control CenterUniversity of Kansas Medical Center3901 Rainbow Blvd., Room B-400Kansas City, KS 661601-800-222-1222Things to consider based on your EMS protocols, procedures and/or policies:Naloxone Dose:-7-
SEIZURE: FEBRILEGoals/Objectives: Assess and secure airway Recognition of risk and/orpresence of secondarytrauma Recognition of transportnecessityDispatch Information:Responding to a 15-month-old male having a seizure. Patient’s father called 911 after hebrought child into his room when child would not settle down. Father stated that patientkept thrashing around and then realized he was having a seizure.Chief Complaint:Additional Resources Requested:SeizurePolice and Fire Department, ALSScene Description:December 21st at 0100 Outside temperature is 25 degrees F with 1 inch of new snow on top of 2 inches of ice Patient’s father meets Fire and EMS in living room with child Home noted to be clean Initial Impression: Patient is in pajamas being held by father. Patient is sleepy and whimpers when moved.Vital Sign – Set 1Physical ExamHPI: See events prior belowAVPU: AlertHEENT:S/S: pale, GCS 11 initially; limp limbs,B/P: 80/50Head: Unremarkablebut will move to painHR: 124, regularEyes: Initially, Left – sluggish, Right - quickResp: 30, non-laboredAllergies: NKDAEars: UnremarkableO2 Sat: 94% (room air)Nose: UnremarkablePain:Medications: NoneOral Cavity: UnremarkableGCS: 11 (3, 4, 4)Patient able to clear and control own airwayPmHx: Ear infection three weeks agoBGL:Vital Sign – Set 2Chest:Last Meal: Dinner, 7hr agoEqual chest rise and fall notedAVPU: AlertLung sounds clearB/P: 96/52Events Prior: Patient’s mother is out ofNo external trauma notedHR: 138, regulartown, so father brought son into theirResp: 28, non-laboredroom to sleep. Patient awoke his fatherBack:when he was noted to be moaningO2 Sat: 98% (O2 applied)No trauma notedPain:Current on Immunizations? YesGCS: 12 (3, 4, 5)Abdomen/Pelvis:BGL: 107 mg/dlNo guarding noted upon quadrant palpationPatient Weight: 11kgsVital Sign – Set 3AVPU: AlertB/P: 90/70HR: 120, regularResp: 24, non-laboredO2 Sat: 98% (O2 applied)Pain:GCS: 13 (4, 4, 5)BGL:Suggested Treatment:O2, Monitor, Airwaymonitor/controlNo trauma notedPelvis stableNotes:Body Temp: 99.4Extremity:No trauma noted to legs or armsPMS x 4 (presumed, since child moves limbaway when pain applied)ECG: Sinus TachycardiaFather denies noting any recent feversOther:Skin: pale, warmNo step off’s or tenderness noted to neckTransport Consideration:Pupils noted to be PERL 10 minutes into callSecuring patient properly on cotGuardian ride along-8-
SEIZURE: FEBRILEAdditional Things to Consider about the Scene: Will family allow you to view where the seizure activity took place Family centered careAdditional Things to Consider during Treatment/Transport: Is or was patient taking any medications for his recent ear infection Is incontinence noted Was a cooling agent and/or activity done by family prior to your arrival Oral cavity can have trauma secondary to biting of the tongue Weigh the pros and cons of starting an IV on this patient Keep back of ambulance lighting/temperature appropriate for patient comfort, low stimulation Transport to the nearest appropriate facilityAdditional Educational Resources to Consider: Temperature Measurement in Pediatricso 18/Things to consider based on your EMS protocols, procedures and/or policies:*Graphic obtained from medguidance-9-
SEIZURE: E
providers through a scenario containing vital signs, pertinent patient and call information, graphics, considerations and links for additional educational opportunities surrounding that call type. The hope is that this guidebook will encourage additional trainings and educational opportunities on pediatrics throughout the year, while also increasing provider confidence when treating pediatric .


![Informatica Interview Questions and Answers [Scenario-Based]](/img/2/informatica-interview-questions-and-answers-scenario-based-1.jpg)