Transcription
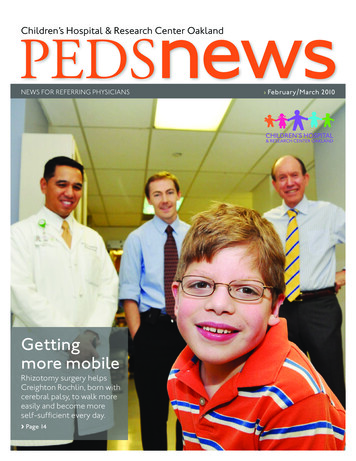
PEDSnewsChildren’s Hospital & Research Center OaklandNEWS FOR REFERRING PHYSICIANSGettingmore mobileRhizotomy surgery helpsCreighton Rochlin, born withcerebral palsy, to walk moreeasily and become moreself-sufficient every day.› Page 14› February/March 2010
› Feature:Section nameCerebral palsy and movement disordersGetting more mobileWRITTEN AND PHOTOGRAPHED BY TOM LEVYCreighton Rochlin, a preemie born with cerebral palsy, lived six weeks on a ventilatorbefore leaving the hospital. Now he’s 9, and thanks to a rhizotomy surgery, he can walkmore easily, with or without crutches, and becomes more self sufficient every day.mommy, look; my feet“ Looklook just like yours now,” saidCreighton Rochlin, 6. It was the firsttime since surgery to correct severespasticity in his legs that Creightonhad gone into the hospital bathroomto urinate standing up. His mother,Jennifer, was there to help.“I was down on my knees in thebathroom, helping to hold him upand totally crying. It was the first timehis feet had ever been flat on the floor.Unless his feet had been in a brace,he’d been on his toes his whole life.”It was the latest milestone in thelife of a boy born very prematurely—at 25 weeks gestation—who lost histwin sister Morgan shortly after birth.Creighton also overcame six weeks ona ventilator and repair of a prematurely fused skull suture and knotted14 › FebrUAry/MArC H 2010intestine, even before he underwentsurgery to combat his spastic legmuscles—caused by cerebral palsy.He didn’t do it alone. Also inthis young fighter’s corner were anolder sister, Emma, a grandmother,two very focused parent-advocates—Stephen and Jennifer—and a teamof clinicians at Children’s Hospital &Research Center Oakland.“Now he can walk independently,with no canes,” said Jennifer. “Andhe’s doing it on his own; he initiatesit on his own. That’s huge, and that’sreally because of the selective dorsalrhizotomy (SDR) surgery he got atChildren’s Hospital.”The most serious symptom ofCreighton’s cerebral palsy is spasticdiplegia. It caused some of his legmuscles to contract so tightly, theiropposing muscles couldn’t activateat all. That turned Creighton into atippy-toe scissors walker.During a six-hour surgery threeyears ago, Children’s neurosurgeonPeter Sun, MD, corrected much ofthat problem by selectively snippingdorsal nerve rootlets determined tobe improperly balancing brain andmuscle signals in his legs.The goal of rhizotomy is to allowmuscle pairs immobilized by spasmcausing brain signals to once againfunction as teams smoothly coordinating walking movements.Hardest part: two-month rehabBut the surgery was only the beginning. The hardest part for Creightonand his family lay ahead: eightweeks of inpatient rehabilitation at
› Section nameCreighton Rochlin, at home in Sonoma withhis family, sat at the kitchen table with hisfather, Stephen, and his sister, Emma.
Creighton and his motherat home in Sonoma.Creighton worked veryhard during eight weeksof inpatient rehabilitationtherapy at Children’sHospital in the region’sonly inpatient pediatricrehabilitation unit.Children’s Hospital, featuring intensework with physical and occupationaltherapists, like Kathryn Rivera-Garcia,PT.“After surgery, children likeCreighton have to do multiple reps ofstrengthening exercises in what we hopethey’ll think of as a game,” said RiveraGarcia. “To see how far he’s come andwhat he’s able to do is really delightful.”Being able to walk with his feet flaton the ground, with or without crutches, doesn’t mean Creighton will eventually be able to throw away his crutchesor wheelchair. But it does mean he canbecome more stable and safer on hisfeet, whether walking unaided, transferring from chair to standing, or evenwhen using walking aids.Creighton now has more potentialthen ever to live life on his own terms, tobe more independent and more mobile.16 › February/Ma rch 2010Journey began at age 1 yearCreighton’s journey through Children’sbegan only a couple of months pasthis first birthday. That’s when he wasreferred to Children’s CraniofacialCenter for metopic synostosis, a prematurely closed skull suture beneath hisforehead. Craniofacial surgeon BryantToth, MD, and Dr. Sun led the teamthat repaired Creighton’s skull during afive-and-a-half-hour surgery.“That surgery went perfectlywell,” said Jennifer. “Sue Ditmyer,RN, PNP—a key member of theNeurosurgery department—came outherself to give us updates and told uswhat was really happening in there. Itreally affected us a lot; the attention sheand the team gave to our family’s pointof view was better than we’d ever had.”A couple of years later, whenCreighton was about 3½, the Rochlinsfollowed up on the Neurosurgery team’srecommendation to connect withChildren’s spasticity clinic. This relationship is what ultimately led to theirdecision to go with SDR surgery.Help from unique clinical teamDuring their first visit to the spasticityclinic they met a clinical team uniquein the western United States.Neurosurgeon Dr. Sun, Orthopedicssurgeon Scott Hoffinger, MD, andRehabilitation Medicine physiatristJacob Neufeld, MD, MSPH, lead amultidisciplinary Children’s Hospitalteam in consultation with the modernday developer of selective rhizotomysurgery, Warwick Peacock, MD, formerchief of Pediatric Neurosurgery at theUniversity of California, Los AngelesMedical Center, and later, at theUniversity of California, San Francisco.
Together, the team meets patientslike Creighton, observes their movement and cognitive abilities, anddiscusses their case histories. Beforemaking a recommendation, the teamconsiders not only whether a rhizotomymay be appropriate, but whether thepatient and family are up to the challenges of the eight-week inpatient rehabilitation that follows the surgery, notto mention the eight-month outpatientrehabilitation that follows release fromthe hospital.“I highly recommend the rhizotomy surgery for anyone who’s a goodcandidate, but I would tell them it’sharder on the family than you realize,”said Jennifer. “We had a year to digestwhat SDR was and whether it was gooddecision for us. Taking into accounthow much we valued Dr. Sun’s skillsand opinions, I was ready to follow himanywhere.”The hard part of the eight weekswas how it stressed the Rochlin family.One parent was virtually full-time withCreighton, the other juggled work,home and their daughter Emma. Thegood part was seeing what Creightonwas able to do as he progressed.“It took a lot of physical therapyto get him on the path to functioning again, to walking,” said Stephen,Creighton’s father. “They even taughthim how to dress himself. That washuge.”correctly, strengthening those musclesas well as enhancing their flexibility.Toe walkers are not only lessstable, they use more energy just to getthrough the day. Learning to walk withfeet flat on the floor after rhizotomysurgery also helps children learn how toget through a full day without endingup exhausted.“It was a lot of fun working withCreighton,” said Mai. “When he visitsnow he loves showing off. ‘I can walkwithout my crutches,’ he shouts. But Istill give him piggy-back rides, just like Iused to do when he was my patient.”After eight weeks of Creighton’sintense rehab therapy with Children’sclinicians like Mai and RiveraGarcia, Creighton’s parents were “allyippy-skippy” and ready to go home.Creighton thought he was too.But when the time came to leave, heburst into tears. “I know I’ve missed allmy friends from school, but now I’vemade all these friends at the hospital,”said Creighton. “And now I have toleave these friends too.”Later, Creighton and his motherran into one of those friends while ona Sonoma-area bike path near theirhome. It was Dr. Neufeld, out for aweekend bicycle ride.“Hey Creighton, what’s up man,”said Dr. Neufeld. “Do you brush yourteeth every night? Do you put yourown socks on?”“Yes I do,” replied Creighton.Creighton and his sister, Emma, share a light-filled play areaand bedroom in the family’s Sonoma-area home.Supported by all at Children’sBut in spite of the hard work and family stresses, the Rochlins felt supportedby everyone at Children’s, especially thephysical and occupational therapists.After all, they spent three hours a day,six days a week doing therapy withCreighton.Physical therapist Tuan Mai, DPT,ATC, CSCS, was an intern while working with Creighton. He was helping reteach Creighton’s muscles how to workP e DS NeWS › 17
› Section nameDuring Children’s monthly spasticityclinic in December 2009, WarwickPeacock, MD, modern founder ofselective dorsal rhizotomy surgery,helped Creighton demonstrate hisability to put his feet flat on the floor.This ultimately will help Creightonbecome more mobile and selfsufficient, especially as he grows intoadulthood.
Peacock Center for Cerebral Palsy and Movement DisordersThe rhizotomy surgery and intensive inpatient rehabilitation Creighton Rochlinreceived are only two of the manyservices available at the Peacock Centerfor Cerebral Palsy and MovementDisorders.This comprehensive, multidisciplinary program brings togetherChildren’s Hospital Oakland specialists in Neurosurgery, Orthopedics andRehabilitation Medicine. The programalso includes specialists in physical andoccupational therapy, as well the onlypediatric inpatient rehabilitation unit inNorthern California.It’s the only center west of KansasCity to offer such a wide range of services and expertise.The center is named after WarwickPeacock, MD, the founder of modernselective rhizotomy surgery, who hasbeen working with the center’s clinicalteam for nine years. “My hope was therewould be a center that would take oncerebral palsy and movement disorderswith the same enthusiasm that I had,”said Dr. Peacock. “I’ve been to clinics allover the world. This one’s got it all.”In 2001, Dr. Peacock agreed to become a consultant to Children’s spasticity/movement disorders clinic.There he operated with Children’sNeurosurgery chief, Peter Sun, MD, during rhizotomy procedures.But now, Dr. Peacock focuses onthe patient evaluation process. “I justgo to the clinic now because the mostdifficult part of treating children withcerebral palsy with surgery is selectingthe right patient,” said Dr. Peacock.During monthly clinics, Dr. Peacockand the rest of the team observepatients, in the exam room and whilepatients demonstrate their walkingabilities. Later, the group discusses eachpatient, making decisions by consensusabout what recommendations to offerpatient families.Clinic options for patients Selective dorsal rhizotomyBaclofen pumpDeep brain stimulationOrthopedic surgical proceduresBotox treatments for spasticityOther medical treatmentRehabilitation services includinginpatient and outpatient physical andoccupational therapyPrincipal cliniciansWarwick Peacock, MD; consultantRenee Graham, OT; occupationaltherapy coordinatorRobert Haining, MD; associate directorof Rehabilitation MedicineScott Hoffinger, MD; chief ofOrthopedics and Sports MedicineJacob Neufeld, MD, MSPH; chief ofRehabilitation MedicineKathryn Rivera-Garcia, PT; physicaltherapy coordinatorPeter Sun, MD; chief of NeurosurgeryFor more information or to make a referral, call 510-428-3655.Warwick Peacock, MD: A life devoted to movementInspired by his childhood fascination with biology and animal movement, Warwick Peacock, MD, knewfrom an early age that he wanted tobecome a physician. He grew up andcompleted medical training in SouthAfrica, and later completed a PediatricNeurosurgery Fellowship at theHospital for Sick Children in Toronto.Warwick Peacock, MDHe then returned to South Africato practice. Inspired by pediatrician Leila Arens, MD, a cerebralpalsy expert, Dr. Peacock began looking at how to improve existing surgical procedures for helping children with cerebral palsy.“I saw that removing certain abnormalities from within theirmovement pattern allowed them to move much more freelyand made life so much easier for them,” said Dr. Peacock.By 1986, Dr. Peacock had done more than 100 selectiverhizotomies. In the process, he became internationally recognized for developing rhizotomy into a safe, effective surgicalprocedure for treating spasticity in children with cerebral palsy.Dr. Peacock developed a method for carefully choosing andmonitoring which nerves to cut. This prevents the commoncomplications of earlier, less careful surgical procedures.In 1986, Dr. Peacock also moved to the United States, tohead Pediatric Neurosurgery at the University of California,Los Angeles School of Medicine (UCLA). Since then, he’sperformed many more rhizotomies, all without any significantcomplications.In 1997, he became chief of Pediatric Neurosurgery at theUniversity of California, San Francisco School of Medicine (UCSF).While he no longer does surgery, Dr. Peacock continues toteach. At UCLA he teaches anatomy to surgical residents and atUCSF he teaches Neurosurgery residents. “I don’t have to operate any more; I can operate through the hands of the peoplethat I’m teaching.”In 2001, Dr. Peacock became a consultant to Children’s spasticity program.“I would like my work with rhizotomy and movement disorders to be handed down,” said Dr. Peacock. “It is something Ibelieve in, something I think makes a big difference in many children’s lives. It would be nice to see it go on and the one placewhere I can best share my experience is Oakland Children’s.”
Creighton. Physical therapist Tuan Mai, DPT, ATC, CSCS, was an intern while work-ing with Creighton. He was helping re-teach Creighton's muscles how to work correctly, strengthening those muscles as well as enhancing their fl exibility. Toe walkers are not only less stable, they use more energy just to get through the day. Learning to walk with