Transcription
Original ArticleComparison of two protocols for maxillary protraction: bone anchors versusface mask with rapid maxillary expansionLucia Cevidanesa; Tiziano Baccettib; Lorenzo Franchib; James A. McNamara, Jrc; Hugo De ClerckdABSTRACTObjective: To test the hypothesis that there is no difference in the active treatment effects formaxillary advancement induced by bone-anchored maxillary protraction (BAMP) and the activetreatment effects for face mask in association with rapid maxillary expansion (RME/FM).Materials and Methods: This is a study on consecutively treated patients. The changes indentoskeletal cephalometric variables from start of treatment (T1) to end of active treatment (T2)with an average T1–T2 interval of about 1 year were contrasted in a BAMP sample of 21 subjectswith a RME/FM sample of 34 patients. All subjects were prepubertal at T1. Statistical comparisonwas performed with t-tests for independent samples.Results: The BAMP protocol produced significantly larger maxillary advancement than the RME/FM therapy (with a difference of 2 mm to 3 mm). Mandibular sagittal changes were similar, whilevertical changes were better controlled with BAMP. The sagittal intermaxillary relationshipsimproved 2.5 mm more in the BAMP patients. Additional favorable outcomes of BAMP treatmentwere the lack of clockwise rotation of the mandible as well as a lack of retroclination of the lowerincisors.Conclusions: The hypothesis is rejected. The BAMP protocol produced significantly largermaxillary advancement than the RME/FM therapy. (Angle Orthod. 2010;80:799–806.)KEY WORDS: Class III malocclusion; Maxillary protraction; Bone anchors; Facial mask;Cephalometricsdental compensation components.1–5 To date, investigations have focused largely on treatment modalitiesand outcomes, with inconsistencies in the timing,duration, and type of treatment.5–19 The timing foreffective maxillary expansion and protraction withcombined rapid maxillary expansion and face masktherapy remains limited to the deciduous or earlymixed dentitions,16 while maxillary protraction withbone anchors and Class III elastics20–23 has beensuccessful in the late mixed or permanent dentitionphases. The present study evaluated the effects ofthese two treatment modalities during the ideal timingfor maxillary protraction with either therapy, providedthat all observed patients in either group wereprepubertal (a requisite for an orthopedic impact onmaxillary sutural structures15,24).Specifically, the purpose of this study on consecutively treated patients was to compare active treatmenteffects in the skeletal maxillary and mandibularstructures, and dentoalveolar compensations for twoprotocols for Class III treatment: bone-anchoredmaxillary protraction (BAMP) and face mask therapyin association with rapid maxillary expansion (RME/FM).INTRODUCTIONClass III malocclusions result from a spectrum ofcranial base, maxillary, and mandibular skeletal andaAssistant Professor, Department of Orthodontics, School ofDentistry, University of North Carolina, Chapel Hill, NC.bAssistant Professor, Department of Orthodontics, Universityof Florence, Florence, Italy; Thomas M. Graber Visiting Scholar,Department of Orthodontics and Pediatric Dentistry, School ofDentistry, University of Michigan, Ann Arbor, Mich.cThomas M. and Doris Graber Endowed Professor ofDentistry, Department of Orthodontics and Pediatric Dentistry,School of Dentistry; Professor of Cell and DevelopmentalBiology, School of Medicine; Research Professor, Center forHuman Growth and Development, The University of Michigan,Ann Arbor, Mich; Private practice, Ann Arbor, Mich.dAdjunct Professor, Department of Orthodontics, School ofDentistry, University of North Carolina, Chapel Hill, NC; Privatepractice, Brussels, Belgium.Corresponding author: Dr Tiziano Baccetti, Department ofOrthodontics, University of Florence, Via del Ponte di Mezzo, 4648, Florence, Italy 50127(e-mail: t.baccetti@odonto.unifi.it)Accepted: January 2010. Submitted: November 2009.2010 by The EH Angle Education and Research Foundation,Inc.GDOI: 10.2319/111709-651.1799Angle Orthodontist, Vol 80, No 5, 2010
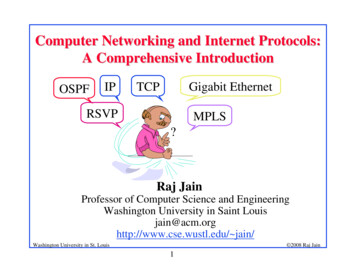
800CEVIDANES, BACCETTI, FRANCHI, MCNAMARA JR, DE CLERCKFigure 1. Synthetic lateral cephalogram generated from cone-beam computed tomography (CBCT).MATERIALS AND METHODSSubjectsThe sample consisted of Class III malocclusionpatients treated with BAMP or RME/FM. At the time ofinitial observation (T1), all patients in both groups hadClass III malocclusion in the mixed or permanentdentitions characterized by a Wits appraisal of 21 mmor less, anterior crossbite or incisor end-to-endrelationship, and Class III molar relationship. Allpatients were of White ancestry, with a prepubertalstage of skeletal maturity according to the cervicalvertebral maturation method (CS1–CS3).24 All patientswere treated at least to a positive dental overjetbefore discontinuing treatment; most patients wereovercorrected toward a Class II occlusal relationship.Angle Orthodontist, Vol 80, No 5, 2010Compliance with the instructions of the orthodontistand staff varied among the patients; variations due tocompliance were not assessed in this study.Twenty-one (11 girls, 10 boys) consecutive patientswere treated by a single operator (Dr De Clerck) withthe BAMP technique. Success of therapy at the end ofthe observation period was not a determinant factor forselection of patients because this sample was collected prospectively. An informed consent was signedby the parents of the patients before treatment. Conebeam computed tomograms (CBCTs) were takenimmediately following the placement of the miniplates(T1), and after approximately 1 year (T2). Scans wereacquired using an iCat machine (Imaging SciencesInternational, Hatfield, Pa) with a 16 cm 3 22 cm fieldof view. The CBCTs were used to generate synthetic
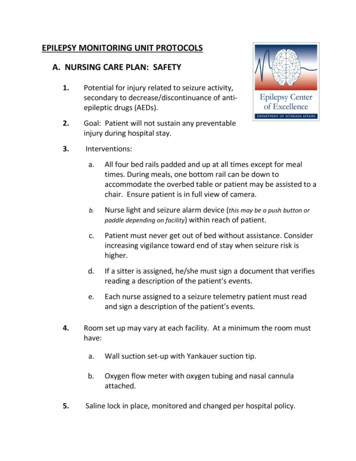
BAMPVS801RME/FMFigure 2. Class III correction achieved with the bone-anchored maxillary protraction (BAMP) orthopedic protocol.lateral cephalograms25–26 with magnification of 7.5%(Dolphin Imaging 10.5, Dolphin Imaging & Management Solutions, Chatsworth, Calif; Figure 1).Cephalometric records of 34 patients (20 girls, 14boys) who were treated consecutively with RME/FMtherapy were obtained from The Department ofOrthodontics and Pediatric Dentistry at the Universityof Michigan. All cephalograms of adequate qualitywere available at T1 and within 1 month after RME/FMtherapy (T2).Mean age for the BAMP sample at T1 was 11 years10 months 6 1 year 10 months, and at T2 it was12 years 10 months 6 1 year 10 months, with a meantreatment duration of 12 months. Mean age for theRME/FM sample at T1 was 8 years 3 months 6 1 year10 months, and at T2 it was 9 years 6 1 year10 months, with a mean treatment duration of10 months. The enlargement factor of the cephalograms in the two samples was very similar (about 8%),and no correction was made for enlargement in theanalysis of the films.BAMP ProtocolIn each patient, four miniplates were inserted on theleft and right infrazygomatic crest of the maxillarybuttress and between the lower left and right lateralincisor and canine. Small mucoperiosteal flaps wereelevated, and the modified miniplates (Bollard, Tita-Link,Brussels, Belgium) were secured to the bone by two(mandible) or three (maxilla) screws (2.3 mm diameter,5 mm length). The extensions of the plates perforatedthe attached gingiva near the mucogingival junction(Figure 2). Three weeks after surgery, the miniplateswere loaded. Class III elastics applied an initial force ofabout 150 g on each side, increased to 200 g after1 month of traction, and to 250 g after 3 months.The patients were asked to replace the elastics atleast once a day and to wear those 24 hours per day.In 14 patients, after 2 to 3 months of intermaxillarytraction, a removable bite plate was inserted in theupper arch to eliminate occlusal interference in theincisor region until correction of the anterior crossbitewas obtained. Placement and failure of miniplates aswell as patient and surgeon perceptions have beenpreviously described in the literature.21RME/FM ProtocolThe three components of the orthopedic face masktherapy used in this study were a maxillary expansionappliance, a face mask, and heavy extraoral elastics.16,27–28 Treatment began with the placement of abonded or banded maxillary expander to which wereattached vestibular hooks extending in a superior andanterior direction. Patients were instructed to activatethe expander once or twice a day until the desiredtransverse width was achieved.Patients were given face masks with pads fitted tothe chin and forehead for support immediately afterexpansion. Elastics were attached from the solderedhooks on the expander to the support bar of the faceAngle Orthodontist, Vol 80, No 5, 2010
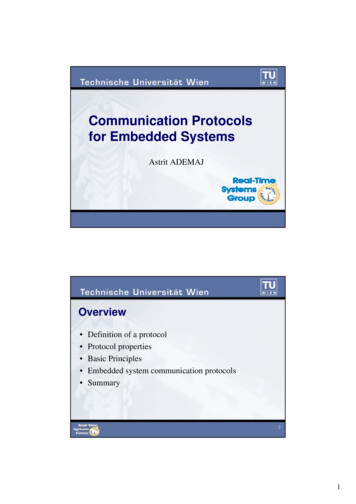
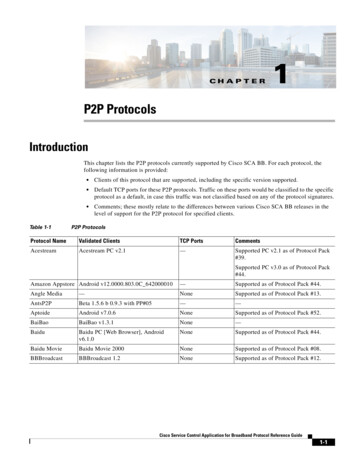
802CEVIDANES, BACCETTI, FRANCHI, MCNAMARA JR, DE CLERCKmask in a downward and forward vector, producingorthopedic forces of 300 g (first 2 weeks) to 500 g perside. The patients were instructed to wear the facemasks for at least 14 hours per day.Cephalometric AnalysisAll cephalograms were digitally traced by twoexaminers, using the Dolphin 10.5 and Viewbox softwares (Viewbox 3.1, dHal, Kifissia, Greece). Thecephalometric measures selected were based on apreviously described reference system15 traced throughcraniofacial stable structures, with addition of Pg toVertT, the inclination of the incisors to their respectivebases, the Wits appraisal, the maxillomandibular differential, and the mandibular angle Co-Go-Me (Figure 3).Before the cephalometric analysis, 15 lateral cephalograms were traced and measured two times within aweek by the same operator (Dr Baccetti). Theintraclass correlation coefficients (ICC) indicated excellent intraobserver agreement of the repeatedmeasurements (ICCs varied between 0.966 for theML-SBL angle and 0.995 for the inclination of themaxillary incisor to NL). Linear measurement errorsaveraged 0.4 mm (SD 0.8 mm), and angular measurements averaged 0.6u (SD 0.6u).Statistical AnalysisThe homogeneity between the two treatment groupsallowed for comparisons without annualizing the data.At exploratory analysis by Shapiro-Wilks test, the datarevealed a normal distribution. Therefore, parametricstatistics were applied. Significant differences betweenthe cephalometric variables (Mx-Md differential, Wits,NL-ML, ANS-Me, Co-Go-Me, Ovj, Ovb, and molarrelation) at T1 in the two treated groups were testedwith independent sample t-tests. Linear skeletalmeasures were not compared between the two groupsat T1 because of differences in age.Descriptive statistics were calculated for all measures at T1 and T2 for the two treated groups. T1–T2changes in both groups and statistical significance ofcomparisons on the changes between the two groupswere assessed with independent sample t-tests (SPSS12.0, SPSS Inc, Chicago, Ill). Statistical significancewas tested at P , .05, P , .01, and P , .001. Thepower of the study was adequate (greater than 0.85),calculated using the mean values and standarddeviations of A-VertT,15 at an alpha of .05, for a clinicaldetectable difference of 2.5 mm.RESULTSThe analysis of the dentofacial characteristics in thetwo treated samples at T1 revealed that there were noAngle Orthodontist, Vol 80, No 5, 2010Figure 3. Cephalometric measures. (A) Linear measures. (B)Angular measures.statistically significant differences between the twogroups at T1 for the analyzed parameters.The changes between T1 and T2 (Table 1) revealedsignificant differences between the two groups in termsof active treatment effects. In particular, both A-VertTand midfacial length (Co-A) showed an averagegreater improvement in the BAMP subjects over theRME/FM subjects of 2.3 mm and 2.9 mm, respectively.Intermaxillary skeletal variables revealed significantly greater improvements in the BAMP group, with
BAMPVS803RME/FMTable 1. Descriptive Statistics for T1–T2 Changes and ComparisonsaBAMP (n 5 21)A-VertT, mmCo-A, mmB-VertT, mmPg-VertT, mmCo-Gn, mmCo-Go, mmGo-Gn, mmWits, mmMx-Md differential, mmML-SBL, degreeNL-SBL, degreeNL-ML, degreeCo-Go-Me, degreeANS-Me, mmU1-NL, degreeL1-ML, degreeOvj, mmOvb, mmMolar relation, mmRME FM (n 5 2.810.63.31.81.91.5 2.3 2.9 0.6 0.5 0.6 1.1 0.9 2.322.322.321.322.922.521.320.3 6.220.9 0.3 *NS*************NS*NS***NSNS**aBAMP indicates bone-anchored maxillary protraction; SD, standard deviation; RME, rapid maxillary expansion; FM, face mask therapy; Sig,significance.* P , .01; ** P , .001; *** P , .0001. NS indicates not significant.both an increase in the Wits appraisal and areduction in the maxillomandibular differential of2.3 mm.No significant differences were found in the sagittalposition of the mandible in the BAMP group comparedwith the RME/FM group. However, control of themandibular vertical growth was statistically significantly different in the two groups. The BAMP groupshowed a slight closure of the angle between themandibular line and the stable basicranial line, of theangle between the nasal line and the stable basicranialline, as well as of the angle between the mandibularline and the nasal line. This treatment protocol alsoresulted in reduced increment in lower anterior facialheight, even though there was greater vertical ramalgrowth in the BAMP group.In the BAMP group, the molar relationship improvedsignificantly more (1.4 mm), and a significant difference in the amount of proclination was recorded for thelower incisors (6.2u more than the RME/FM group). Noother significant differences were found.DISCUSSIONThe present study is the first to compare dentoskeletal changes with RME/FM vs bone anchors forcorrection of Class III malocclusion. These
k, Brussels, Belgium) were secured to the bone by two (mandible) or three (maxilla) screws (2.3 mm diameter, 5 mm length). The extensions of the plates perforated the attached gingiva near the mucogingival junction (Figure 2). Three weeks after surgery, the miniplates were loaded. Class III .