Transcription
CLINICAL RESEARCH STUDYEtiology and Diagnosis of Systolic Murmurs in AdultsSteven McGee, MDPrimary and Specialty Medical Care, Department of Veterans Affairs Medical Center, Seattle, Wash; Department of Medicine,University of Washington, Seattle.ABSTRACTBACKGROUND: It is unknown whether echocardiography can provide insights into the origin of systolicmurmurs and the modern value of bedside cardiovascular diagnosis.METHODS: The author examined 376 inpatients and compared their physical findings to transthoracicechocardiography, exploring the associations between echocardiography and systolic murmurs and investigating the diagnostic accuracy of physical examination for pathologic murmurs.RESULTS: Four echocardiographic variables predict the presence of systolic murmurs: peak aortic velocity(P .001); mitral regurgitation severity (P .001); mitral valve E-point velocity (P .09); and absence ofpericardial effusion (P .09). When diagnosing murmurs, the most helpful finding is its distribution on thechest wall with respect to the 3rd left parasternal space, a landmark that distinguishes murmurs into 6patterns. The “apical-base” pattern indicates increased aortic velocity (likelihood ratio [LR] 9.7; 95%confidence interval [CI]; 6.7-14): a delayed carotid upstroke (LR 6.8; 95% CI; 4.0-11.5); absent S2 (LR12.7; 95% CI; 5.3-30.4); and humming quality to the murmur (LR 8.5; 95% CI; 4.3-16.5) further increasethe probability of aortic valve disease. The “broad apical” murmur pattern suggests significant mitralregurgitation (LR 6.8; 95% CI; 3.9-11.9); and the “left lower sternal” murmur pattern indicates significanttricuspid regurgitation (LR 8.4; 95% CI; 3.5-20.3): additional bedside observations refine these diagnoses.Nonetheless, this study shows that some classic physical findings are no longer accurate, that physicalexamination cannot reliably distinguish severe aortic stenosis from less severe stenosis, and that classicphysical findings, despite having proven value, are absent in many patients with significant cardiac lesions.CONCLUSIONS: In the diagnosis of systolic murmurs, physical examination has limitations but alsounappreciated value. A simple system using onomatopoeia and classifying systolic murmurs into 1 of 6patterns is diagnostically helpful. 2010 Published by Elsevier Inc. The American Journal of Medicine (2010) 123, 913-921KEYWORDS: Heart auscultation; Heart murmurs; Physical diagnosisIn his Treatise on the Diseases of the Heart and GreatVessels,1 published in 1832, just 11 years after Laennec’sinvention of the stethoscope, the British physician JamesHope fully described the characteristics of systolic murmurs, attributing them to either abnormal forward flow oversemilunar valves (eg, aortic or pulmonic valve) or regurgi-Funding: None.Conflict of Interest: There are no financial or personal relationshipsthat could have inappropriately biased this work.Authorship: The author performed all aspects of the study and analysisof its results.Requests for reprints should be addressed to Steven McGee, MD,Seattle-Puget Sound VA Health Care System (111M), 1660 South Columbian Way, Seattle, WA 98108.E-mail address: steven.mcgee@med.va.gov0002-9343/ -see front matter 2010 Published by Elsevier Inc.doi:10.1016/j.amjmed.2010.04.027tation of blood from high pressure chambers into low pressure ones (eg, mitral or tricuspid regurgitation). His observations—along with those of Austin Flint (1812-1886),Graham Steell (1851-1942), and others using phonocardiography during the 1950s and 1960s—form virtually ourentire knowledge base about systolic murmurs, includingthe classic teaching that pathologic systolic murmurs areidentifiable by their location on the chest wall and by additional abnormalities of the neck veins, precordial pulsations, arteries, and heart tones.During recent decades the diagnosis and treatment ofheart disease have changed significantly, and it is unknown whether these classic tenets remain true. For example, original observations were mostly of young patients with rheumatic and congenital heart disease andnormal ejection fractions; modern patients, in contrast,
914The American Journal of Medicine, Vol 123, No 10, October 2010are frequently elderly and more often have ischemic,Statistical Methodscalcific, or degenerative heart disease with reduced venUsing echocardiographic parameters as the independenttricular function.variable and either presence of systolic murmur or theEchocardiography has been widely applied to modernspecific murmur pattern as the dependent variable, the aucardiovascular diagnosis, yet few if any studies providingthor conducted both univariate analysis (2-sided t-test foradditional insights into systoliccontinuous variables; chi-squaredmurmurs have appeared. The purtest for categorical variables) andpose of this study is to carefullymultivariate analysis (logistic reCLINICAL SIGNIFICANCEexamine a series of hospitalizedgression with SPSS 13 software;patients and compare their physiSPSS Inc., Chicago, IL). In the Four echocardiographic findings are ascal findings to transthoracic echomultivariate analysis, variablessociated with systolic murmurs: 1) aorcardiography, thereby investigatentered the model if P .05 andtic valve velocity, 2) mitral regurgitaing both the etiology of systolicremained if P .10. Diagnostiction severity, 3) absence of pericardialmurmurs and the modern diagnosticaccuracy was expressed usingeffusions, and 4) mitral valve E-pointvalue of the bedside examination.likelihood ratios (LRs).3velocity.METHODS When diagnosing systolic murmurs, themost helpful physical finding is its distribution on the chest wall with respectto the 3rd left parasternal space.RESULTSThere were 409 patients examined,aged 22 to 94 years (mean SD,Between 2001 and 2006, the au69 12 years); 399 (97%) werethor examined 409 inpatients atmen. The indications for echocar Additional classic cardiovascular findthe Seattle Veterans Affairs Meddiography included l Center. These patients were afor structural heart disease (59%),aresometimesabsentinpatientswithconvenience sample, principallyprogression of preexisting valvularsignificant cardiac pathology.of non-intensive care unit patientsdisease (16%), source of arterialundergoing echocardiography duringemboli (8%), suspected endocarditheir hospital stay. With only 14tis (7%), or suspected pericardialexceptions, the author was undisease (2%). Only 7% of the echocardiograms were orderedaware of the patient’s diagnosis, indication for echocardito diagnose unexplained murmurs. Thirty-three patientsography, or echocardiographic results. Using a standardizedwere excluded from analysis because they had diastolic orform, the author recorded the patient’s vital signs, arterialsystolic/diastolic murmurs (n 18) or lacked completeand venous pulsations (contour, velocity, waveforms), preechocardiograms (n 15), leaving 376 patients, 221 (59%)cordial pulsations (location, velocity, amplitude), heartof whom had systolic murmurs.tones (first, second, third, fourth, and extra heart sounds andtheir characteristics), and murmurs (systolic, diastolic, orAssociations between Echocardiography andboth). Examination of the arteries, veins, and precordiumPresence of Systolic Murmurpreceded auscultation. The anterior chest from apex toAs displayed in Table 2 (online), over 20 echocardiographicclavicles was examined, and radiation of murmurs wasfindings were associated with systolic murmurs, but aftercompletely described. Although most patients were exmultivariate analysis only 4 variables remained: aortic valveamined in 3 positions (ie, supine, left lateral decubitus,(AV) peak velocity (P .001), E-point velocity (P .092),and upright positions), reported findings refer only to themitral regurgitation severity (P .001), and absence ofsupine patient.pericardial effusion (P .090). In addition, tricuspid regurMurmurs were defined as continuous sounds that pergitation severity was independently associated with the “leftsisted during inspiration and expiration, although their inlower sternal border” murmur pattern (P .001). Pericardialtensity could vary during the respiratory cycle. In contrast,effusions diminished the probability of all 6 murmur patcontinuous sounds that completely disappeared during interns (ie, 60% of patients without pericardial effusions hadspiration or expiration were called rubs. All murmurs weremurmurs vs. only 25% of those with effusions; most effucharacterized using onomatopoeia and conventional gradingsions were clinically unimportant). Increasing E-point ve(Table 1)2 and were sorted into 6 predetermined topolocity also was associated with all 6 systolic murmur patgraphic patterns (Figure 1). All echocardiograms were interns, and its association persisted after excluding patientsterpreted by a cardiologist independent from the bedsidewith increased AV velocity or mitral regurgitation (ie, in theexamination. Echocardiographic regurgitation was signifi106 patients with AV velocity 1.8 m/sec and withoutcant only if moderate or severe.mitral regurgitation, 43% with E-point velocity ⱖ0.9 m/secThe study protocol was approved by the institutionalhad systolic murmurs vs. 21% with E-point velocity 0.9review board at the Seattle-Puget Sound Veterans AffairsMedical Center.m/sec, P .03).Study Protocol
McGeeEtiology and Diagnosis of Systolic MurmursTable 1Definitions of Physical FindingsCharacteristicTiming of sound*MidsystolicEarly systolicLong systolicHolosystolicLate systolicQualityBlowingCoarseIntensity – loudestgrade recorded†123Carotid upstroke‡DelayedBriskRightventricular (RV)rockDefinitionBoth S1 (lub) and S2 (dup) distinct:Lub shsh dupS1 indistinct, S2 distinct; gap before S2Shshsh dupPushsh dupS1 indistinct, S2 distinct; no gapbefore S2:ShshshshshdupPushshshshdupS1 and S2 shshshshshPS1 distinct, S2 indistinct:Lub shshshPPure high frequency, mimicked by thesounds ahahah or shshsh (soundsproduced in the front of themouth)Mixture of frequencies, mimicked by thesound of clearing the throat(produced farther back in themouth)Faint, heard with special effortRecognized readily after placing thestethoscope on the chest wallVery loud, but lacks palpable thrillDefinite slow increase in carotidupstroke, occupying much ofsystole and different from the earlytapping sensation of the normalcarotidUnusually brisk carotid upstroke,different from the early tappingsensation of the normal carotidSimultaneous systolic retraction of theapical area and outward motion ofthe lower sternum (this precordialmotion results from a dilated rightventricle at the apex ejecting bloodinto the dilated right atrium andliver near the sternum)*Characteristics of S1 and S2 are based on distinctness of heartsounds at the location where the murmur is loudest.†All murmurs in this study lacked palpable thrills and were thus grade3 or less.2‡Both carotids were examined at the anterior border of the sternocleidomastoid muscle in the mid neck, using the examiner’s left thumb(on the patient’s right carotid) or right fingertips (on the patient’s leftcarotid).915Correlations between Murmur Pattern andEchocardiographyPeak aortic velocity, mitral regurgitation, and tricuspid regurgitation were the 3 principal echocardiographic variablesassociated with specific murmur patterns. Because manypatients had combinations of these abnormalities, Figure 2presents isolated lesions to simplify analysis. As AV peakvelocity increases from 1.3 m/sec to ⱖ4 m/sec, the frequency of murmurs increases from 19% to 100%: the “isolated base” pattern appears at AV peak velocities of 1.3-2.1m/sec (see later), the “isolated apical” and “small apicalbase” patterns at 1.5-2.5 m/sec, and the “broad apical-base”pattern at ⱖ2.1 m/sec. As mitral regurgitation increasesfrom none to severe, the frequency of murmur increasesfrom 29% to 100%: the “broad apical” pattern is the mostcommon pattern, although some patients with severe regurgitation have the “broad apical-base” pattern and otherswith moderate regurgitation have the “isolated apical” pattern. As tricuspid regurgitation increases from none to severe, the frequency of murmur increases from 21% to100%: the “left lower sternal” pattern is the only associatedpattern.Table 3 summarizes the combinations of increased AVvelocity, mitral regurgitation, and tricuspid regurgitation inall patients with each murmur pattern. Peak AV velocity isdivided into 5 groups: 1.8 m/sec (normal AV velocity);1.8-2.4 m/sec (increased AV velocity without obstruction);and 2.5-2.9 m/sec, 3-3.9 m/sec, and ⱖ4 m/sec, velocitiescorresponding to mild, moderate, and severe aortic stenosis,respectively. Twenty percent of all patients had aortic stenosis (ie, AV velocity ⱖ2.5 m/sec), 20% had mitral regurgitation (moderate or worse), and 18% had tricuspid regurgitation (moderate or worse).Diagnostic Accuracy of Physical ExaminationAll Patients. The most useful finding, applicable to allpatients, is the specific murmur pattern detected. The “broadapical-base” pattern increases the probability of AV velocity ⱖ2.5 m/sec (LR 9.7), the “broad apical” pattern increases the probability of mitral regurgitation (LR 6.8),and the “left lower sternal” pattern increases the probabilityof tricuspid regurgitation (LR 8.4). The absence of systolic murmur greatly decreases the probability of AV velocity ⱖ2.5 m/sec (LR 0.05), but only slightly decreasesthe probability of regurgitation (LRs 0.4 and 0.6 for mitraland tricuspid regurgitation, respectively) (Table 4).Additional findings increasing the probability of AVvelocity ⱖ2.5 m/sec are inaudible S2 at the left 2nd parasternal space, radiation of the murmur to both sides of the neckand clavicles, humming murmur quality, delayed carotidupstroke, inaudible S1 at the apex, and coarse murmurquality (LRs 3.3-12.7, see Table 4). Additional findingsdecreasing the probability of AV velocity ⱖ2.5 m/sec (andthus arguing against aortic stenosis) include mid-systolictiming, absence of radiation into the neck, grade 1 intensity,and “broad apical” pattern (LRs 0.05-0.2).
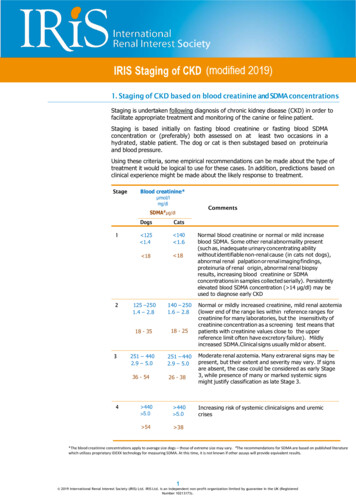
916The American Journal of Medicine, Vol 123, No 10, October 2010Figure 1 The 6 murmur patterns are distinguished by their distribution with respect toa key landmark, the 3rd left parasternal interspace (indicated by “ ” on each drawing).Two patterns (broad apical-base pattern and small apical-base pattern, top 2 rows) extendabove and below this landmark, usually to both sides of the sternum. The “broad apicalbase” pattern extends at least from the first right parasternal space to the apex (ie, 4thintercostal space at the midclavicular line [MCL]), whereas the “small apical base” patterndoes not extend this far. Three patterns are confined entirely below this landmark (leftlower sternal pattern, broad apical pattern, and isolated apical pattern, 3rd through 5throws); 1 pattern is confined entirely above this landmark (isolated base pattern, bottomrow). The vertical line over the left chest in each drawing depicts the MCL.Additional findings increasing the probability of mitralregurgitation (LRs 2.9-4.7) are a loud S2 at the left 2ndparasternal space, unchanging murmur intensity despite anirregular rhythm, and chaotic pulse rhythm (ie, atrial fibrillation). Findings supporting a diagnosis of significant tricuspid regurgitation (LRs 10.9-31.4) are early systolic out-
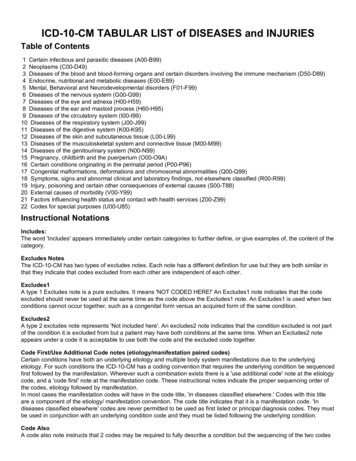
McGeeEtiology and Diagnosis of Systolic Murmurs917Figure 2 Murmur patterns of isolated lesions. The figure presents the murmur patterns reflecting isolated aortic velocity (top row; 247patients without significant mitral or tricuspid regurgitation), isolated mitral regurgitation (middle row; 174 patients with AV peakvelocity 1.8 m/sec and without significant tricuspid regurgitation), and isolated tricuspid regurgitation (bottom row; 161 patients withAV velocity 1.8 m/sec and without significant mitral regurgitation). See text.ward movement in the neck veins (ie, CV wave), lowersternal pulsations, hepatic pulsations, and a “right ventricular rock.” All pathologic murmurs had long systolic orholosystolic timing or, in some patients with mitral regurgitation, late systolic timing.Patients with “Broad Apical-base” Pattern. The mostcommon murmur pattern was the “broad apical-base” pattern (n 92, 25% of all patients). Ninety-eight percent ofthese patients had increased AV velocity (ⱖ1.8 m/sec, Table 3): 28% had increased aortic flow without stenosis, 42%had mild or moderate aortic stenosis, and 28% had severeaortic stenosis. In patients with the “broad apical-base”pattern, several findings accurately detect aortic stenosis (ie,AV velocity 2.5 m/sec, Table 4): humming quality, delayed carotid upstroke, and inaudible S1 or S2; others indicate increased flow without stenosis (ie, AV velocity 1.8-2.4m/sec): mid-systolic timing, brisk carotid upstroke, grade 1intensity, and blowing quality. Nonetheless, few findingsaccurately diagnose severe aortic stenosis (AV velocity 4 m/sec): only blowing quality and early-systolic timing decrease the probability of this diagnosis (LRs 0.1for both).In patients with the “broad apical-base” pattern, a loud S2increases the probability of mitral regurgitation (LR 3.3), adiagnosis otherwise difficult to make because the “broad apical-base” pattern circumscribes the “broad apical” pattern.Patients with Other Murmur Patterns. Seventy-four percent of patients with the “small apical-base” pattern havemodest increases in aortic velocity (AV velocity 1.8-2.4m/sec, Table 3), but aortic stenosis is rare. In patients withthe “isolated apical” pattern, 35% have mildly increasedaortic velocity and 28% have mitral regurgitation, but no
918Table 3The American Journal of Medicine, Vol 123, No 10, October 2010Characteristics of Various Patterns*Murmur t lPatternIsolatedBasePatternnAortic velocity (m/sec)† 1.81.8-2.42.5-2.93.0-3.9ⱖ4Mitral regurgitation‡Tricuspid 5)(28)(11)23600022(79)(21)(7)(7)*All values n (%, of total in column).†These aortic velocities correspond roughly to normal velocity ( 1.8 m/sec), increased flow without obstruction (1.8-2.4 m/sec), mild aortic stenosis(2.5-2.9 m/sec), moderate aortic stenosis (3.0-3.9 m/sec), and severe aortic stenosis (ⱖ4 m/sec).‡Regurgitation, moderate or worse.additional finding distinguishes these patients. The “isolatedbase” pattern is associated with modestly increased aorticvelocity (21% have AV velocity 1.8-2.4; Figure 2, Table 3),but many of these murmurs are probably extracardiac (eg,arteriovenous fistula or great artery stenosis), because theyfrequently radiate to distant sites over the neck or clavicleand because 53% of patients had either hemodialysis fistulae or asymmetry of the carotid or radial pulses.Frequency of FindingsInspection of the “frequency of finding” column (Table 4)indicates that many patients lack anything diagnostic otherthan a specific murmur pattern. For example, in patientswith the “broad apical-base” pattern, a delayed carotid upstroke argues for AV velocity ⱖ2.5 m/sec (LR 6.3) and abrisk carotid upstroke argues against this diagnosis(LR 0.05), but 61% of patients with this pattern have anormal carotid upstroke, a finding of little diagnostic value(LR 0.7). Therefore, although classic findings have provenaccuracy, they are frequently absent.DISCUSSIONThis study leads to 3 important conclusions. First, althoughit confirms the classic teaching that systolic murmurs areassociated with increased AV velocity, mitral regurgitation,and tricuspid regurgitation, it identifies 2 additional variables associated with systolic murmurs: the absence of pericardial effusions and increased E-point velocity. Pericardialeffusions (even if small) decrease the probability of systolicmurmurs, probably just as pleural effusions impair transmission of lung sounds. The role of E-point velocity is lessobvious because it measures early diastolic flow over themitral valve. Increased E-point velocity may reflect elevatedfilling pressures, which tense the ventricular walls and ren-der them more susceptible to vibrations producing sound,similar to the way a tense violin string is more likely tovibrate than a relaxed one.Second, systolic murmurs are distinguished into 6 diagnostic patterns, based on the murmur’s distribution aboutthe 3rd left parasternal space (the landmark overlying bothaortic and mitral valves). Inspection of the boundary surrounding all 6 murmur patterns suggests that the primarydeterminant of sound radiation is not necessarily the direction of blood flow but instead the orientation of bony thorax,specifically the left lower ribs, sternum, and clavicles (Figure 3). Increased flow across a semilunar valve or through aregurgitant leak generates vibrations in the ventricles, greatarteries, or both, which— depending on their location, amplitude, and ease of conduction to the bones of the bodywall— produce 1 of the 6 different murmur patterns. In fact,one of the best arguments that bone conduction—and notdirection of blood flow— governs distribution of sound isthe murmur of mitral regurgitation: in this lesion, bloodflows from the left ventricle rightward and upward to theleft atrium, yet the murmur radiates almost perpendicular tothis, along the left lower ribs to the axilla.Finally, despite changing etiologies and treatments ofheart disease, many classic physical findings remain accurate today (carotid upstroke, murmur radiation and quality,venous waveforms, and others). A new observation is theassociation between a loud S2 at the left base and significantmitral regurgitation. S2 may be loud in mitral regurgitationbecause of pulmonary hypertension, absence of a loud contiguous murmur obscuring S2 (ie, mitral regurgitation murmurs are confined below the 3rd rib), a freely mobile aorticvalve (ie, no calcific aortic disease) or, in patients withassociated aortic disease, a shorter left ventricular ejectiontime (thus shortening the associated aortic murmur andrevealing a loud S2).
McGeeTable 4Etiology and Diagnosis of Systolic Murmurs919Diagnostic Accuracy of Bedside ExaminationLikelihood Ratio (95% CI), for Detecting*:FindingAll patientsMurmur pattern“Broad apical-base” pattern“Small apical-base” pattern“Left lower sternal” pattern“Broad apical” pattern“Isolated apical” pattern“Isolated base” patternNo murmurArterial pulseCarotid upstroke delayedCarotid upstroke normalCarotid upstroke briskPulse rhythmRegularChaoticVenous pulsationEarly systolic outward movement (CV wave)Precordial pulsationLower sternal pulsationHepatic pulsationRV rockHeart tonesS1 inaudible, apexS2 inaudible, 2nd left parasternal spaceS2 loud, 2nd left parasternal spacePatients with systolic murmursMurmur radiationNo radiation to neckRadiation to right clavicle, right neck, or bothRadiation to clavicles and neck on both sidesMurmur qualityBlowing qualityCoarse qualityAdded humming qualityMurmur timingMidsystolicEarly systolicLong systolicHolosystolicLate systolicMurmur gradeGrade 1Grade 2Grade 3If pulse rhythm irregular, murmur intensity samein the beat after a pausePatients with “broad apical-base” murmursArterial pulseCarotid upstroke delayedCarotid upstroke normalCarotid upstroke briskFrequency ofFinding (%)AV Peak Velocityⱖ 2.5 4-4.5)(0.1-2.4)(0.1-1.6)(0.4-1.0)148246.8‡ (4-11.5)0.6‡ (0.5-0.8)0.3 (0-2.2)2.0‡ (1.1-3.5)0.9 (0.8-1.0)0.6 (0.1-2.5)1.4 (0.7-2.6)1.0 (0.9-1.1)0.2 (0-2.8)66191.0 (0.8-1.2)1.1 (0.6-1.8)0.5‡ (0.4-0.7)2.9‡ (1.9-4.2)0.6‡ (0.4-0.8)3.0‡ (2.0-4.4)9.10.9‡ (5.5-22)431.12.5‡ (4.1-38)12.1‡ (3.3-44)31.4‡ (1.6-600)208135.1‡ (3.5-7.4)12.7‡ (5.3-30.4)1.7 (0.9-3.1)1.4 (0.9-2.2)0.5 (0.2-1.6)4.7‡ (2.7-8.3)1.0 (0.6-1.7)1.4 (0.6-3.3)3.6‡ (2.1-6.3)4511130.2‡ (0.1-0.3)2.4‡ (1.1-5.2)12.4‡ (4.5-34)1.6‡ (1.2-2.1)0.7 (0.3-1.8)0.5 (0.2-1.3)1.5‡ (1.2-2.0)0.8 (0.3-2.2)0.4 (0.1-1.3)1.5‡ (1.2-1.8)0.5‡ (0.3-0.8)0.7 (0.4-1.5)1.4‡ (1.2-2.8)0.5‡ (0.3-0.9)1.3 (0.7-2.4)5743210.3‡ (0.2-0.4)3.3‡ (2.4-4.5)8.5 � (1.6-24.5)0.7‡ (0.5-0.9)0.05‡ (0-0.9).
920Table 4The American Journal of Medicine, Vol 123, No 10, October 2010ContinuedLikelihood Ratio (95% CI), for Detecting*:FindingHeart tonesS1 inaudible, apexS2 inaudible, 2nd left parasternal spaceS2 loud, 2nd left parasternal spaceMurmur characteristicsRadiation to clavicles and neck on both sidesNo radiation lateral to mid clavicular lineBlowing qualityAdded humming qualityMidsystolic timingGrade 1 intensityFrequency ofFinding (%)4822183016253877AV Peak Velocityⱖ 2.5 ��3.3‡ (1.5-7.4)15.7 (1.0-251)1.1 (0.4-3.1)0.7 (0.4-1.3)0.2 (0-1.5)3.3‡ -6.5)(0.1-0.7)(0.2-0.6)(1.9-474)(0-0.6)(0-0.7)CI confidence interval; RV rock right ventricular “rock” (definition in Table 1).*Values are likelihood ratio (95% confidence interval).†Regurgitation, moderate or worse.‡The point estimate is statistically significant (ie, confidence interval excludes the value of 1.0).This study also provides evidence supporting the hypothesis that observation of murmur intensity during irregularrhythms is diagnostically helpful.4 After pauses in the heartrhythm (from atrial fibrillation or extrasystoles), the nextventricular beat has increased contractility, increased filling,and decreased afterload relative to prior beats. In patientswith aortic flow murmurs, these hemodynamic changes in-Figure 3 Boundary of murmur patterns. The 3rd left parasternal space overlies both the aortic and mitral valves. If the ventricles vibrate sufficiently to produce sound, murmurs are generatedbelow this landmark. Vibrations of the right ventricle produce the“left lower sternal” pattern, whereas those of the left ventricleproduce the “isolated apical” pattern, larger apical patterns (leftexample of “broad apical” pattern, Figure 1) or, if of sufficientintensity, murmurs along the left ribs from sternum to axilla(right example of “broad apical” pattern, Figure 1). Should thegreat arteries vibrate sufficiently to make sound, the bonesabove this landmark vibrate and murmurs radiate from theupper sternum to clavicles and neck (“isolated base” pattern).With increased velocity across the aortic valve, both the leftventricle (lower ribs) and great arteries (upper sternum andclavicles) vibrate, causing the “apical-base pattern” and itsvariations.crease aortic flow and thus murmur intensity. In regurgitantlesions, however, blood is flowing in 2 directions, and thediminished afterload increases aortic flow but leaves regurgitant volume and murmur intensity unchanged.5In contrast to classic teachings, mitral regurgitation is nolonger associated with a brisk arterial pulse (the historical“small water hammer pulse”), probably because modernpatients are older and lack the supranormal ejection fractions and compliant vessels of younger, historical subjects.Also, the sustained apical impulse and displaced apicalimpulse are not specific for aortic stenosis or mitral regurgitation, respectively, because these findings, when found instudy patients with murmurs, often signified alternativenonvalvular etiologies (eg, cardiomyopathy). Also, in contrast to descriptions of rheumatic aortic valve disease thatemphasized murmurs located at the upper right sternum (theclassic “aortic area”), this study demonstrated that aorticvalve murmurs radiate symmetrically above and below the3rd left parasternal space, in an oblique direction to bothsides of the sternum, in a pattern sometimes resembling asash worn over the right shoulder (“broad apical-base” pattern). Finally, classifying the timing of murmurs using onomatopoeia (Table 1) proved useful, demonstrating holosystolic and long systolic murmurs as more significant thanearly systolic or mid-systolic ones. Onomatopoetic descriptors are also easier to convey to students than older terms(eg, “diamond-shaped,” “crescendo-decrescendo”), probably because they communicate what clinicians actuallyhear, not what was seen on a phonocardiographic tracing.Limitations of this study include a population almost entirely of men; whether the female breast alters the radiation ofthe sound and the conclusions of this study is unknown. Also,patients consisted of a convenience sample and their examinations were necessarily detailed (about 20 minutes per exami-
McGeeEtiology and Diagnosis of Systolic Murmursnation): results may not apply to uncooperative or sicker patients, noisy environments, or more cursory examinations.Even so, traditional cardiovascular examinations have alwaysbeen performed systematically in quiet settings, and the timerequired is similar to that for a complete echocardiogram.Finally, examinations were conducted by a single observer,raising the possibility of poor reproducibility, but many studieshave previously shown good interobserver agreement for mostcard
continuous variables; chi-squared test for categorical variables) and multivariate analysis (logistic re-gression with SPSS 13 software; SPSS Inc., Chicago, IL). In the multivariate analysis, variables entered the model if P.05 and remained if P.10. Diagnostic accuracy was expressed using likelihood ratios (LRs).3 RESULTS There were 409 .