Transcription
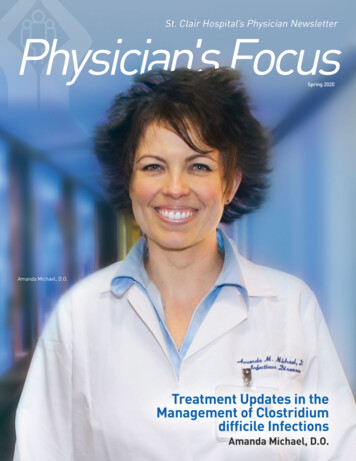
St. Clair Hospital’s Physician NewsletterPhysician's FocusSpring 2020Amanda Michael, D.O.Treatment Updates in theManagement of Clostridiumdifficile InfectionsAmanda Michael, D.O.
Treatment Updates in theManagement of Clostridiumdifficile InfectionsPhysician Lead: Amanda Michael, D.O.In February 2018, the Infectious Diseases Society of America (IDSA) and the Societyfor Healthcare Epidemiology of America (SHEA) released an update in clinical practiceguidelines for the treatment and management of Clostridium difficile infectionsin adults and children. Clostridium difficile (C. diff) is a gram positive, spore-formingAmanda Michael, D.O.bacteria associated with the development of diarrhea and colitis. Severe cases of CDIcan lead to pseudomembranous colitis, toxic megacolon, sepsis, and multi-organ failure. Risk factors for thedevelopment of CDI include antibiotic use, individuals older than 65 years, immunocompromised patients, recenthospitalizations, and a history of prior CDI.Physicians play a pivotal role in the prevention of CDI through the appropriate use of antibiotics. Inappropriateuse of antibiotics not only increases antibiotic resistance rates but can also increase the potential of adverseevents, such as CDI. Symptoms of CDI usually develop shortly after antibiotic use up to 90 days, with the highestrisk of development during the first month of antibiotic consumption. The use of extended spectrum antibiotics canfurther increase this risk of CDI development. These antibiotics classes include, but are not limited to: macrolides(clindamycin), 3rd/4th generation cephalosporins (ceftriaxone/cefepime), fluoroquinolones (ciprofloxacin/levofloxacin), and carbapenems (meropenem/ertapenem).In the updated clinical guidelines, metronidazole is no longer recommended as first-line therapy for the treatmentof CDI in adults. Oral vancomcyin and fidaxomicin are the supported first-line options for both severe and nonsevere initial episodes of CDI. IV metronidazole can be used in combination with oral or rectal vancomycin if an ileusor septic shock is present. Of note, fidaxomicin is non-formulary at SCH and will require an infectious diseasesconsult to evaluate use. Depicted below is suggested oral vancomycin dosing for the treatment of CDI in initialand recurrent episodes. SCH ASP order sets have been updated to reflect these guideline changes.Recommended Agents for the Treatment of Clostridium difficile Infection (CDI)Positive CDI, initial episode Vancomycin oral solution 125 mg PO Q6H x 14 daysPositive CDI, recurrent episode(s)Use prolonged taper dose if standard regimen was used for initial episode. For example: Vancomycin oral solution 125 mg PO Q6H x 10-14 days, followed by Vancomycin oral solution 125 mg PO BID x 7 days, followed by Vancomycin oral solution 125 mg PO daily x 7 days, followed by Vancomycin oral solution 125 mg PO every 48-72 hours for 2-8 weeksPatients with a listed vancomycin allergy (except anaphylaxis) can safely tolerate oral vancomycin.Treatment failure in CDI can occur in patients receiving antimicrobial therapy. Alternative therapy, such as fecalmicrobiota transplant, second-line antimicrobials, and monoclonal antibody therapy with bezloxtoxumab, is oftenused by providers trained in infectious diseases or gastroenterology in the outpatient setting.References: McDonald LC, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children:2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018.doi:10.1093/cid/cix1085.2Physician’s Focus Spring 2020
Glucose Sensorsand Insulin PumpsPhysician Lead: Camille Buonocore, M.D.Many more Type 1 and type 2 diabetic patients are being managed by glucosesensors with and without insulin pumps. The most common Continuous GlucoseMonitoring (CGM) devices, Medtronic, Dexcom, and FreeStyle, all have sensors onthe market for patient use. Sensors require a transmitter so the measured subcutaneousglucose can be communicated to the "receiving" device and seen by the patient and/orcaregiver. Transmitters are the most expensive part of a sensor and may be used forup to 6 months in certain cases, such as the Dexcom sensor.Camille Buonocore, M.D.X-rays and radiation can damage Continuous Glucose Monitoring (CGM) devices. It needs to be determinedif a patient is wearing an insulin pump and/or Continuous Glucose Monitoring (CGM) device at presentation to avoidany damage. Reusable transmitters should be removed prior to testing and left outside of the testing room andsensors should be thrown away. Implanted sensors under the skin can remain in place. After testing, a replacementsensor should be available (from patient home supply) for the patient to apply after the testing is complete.X-rays and radiation can also damage insulin pumps. For pumps with tubing, disconnect the pump and leaveoutside of the testing room. Soft infusion sets where no metal remains in the skin can be capped and remainin place for testing but infusion sets where a metal needle remains in the skin after insertions must be removedwhen having an MRI. For pumps without tubing, remove the pod/patch and leave it outside of the testing room.After testing, replace or reconnect the device (from patient home supply) after the testing is complete.If a patient chooses not to remove their insulin pump or CGM for testing, it may be damaged and no longerworked correctly. The patient would then be responsible for replacing the device.Per hospital policy, personalContinuous Glucose Monitoring (CGM)devices will only supplement standard,intermittent, point of care blood glucosemonitoring as ordered physicians.Because there is no way to validatethe accuracy of personal continuousglucose monitoring devices, the resultsobtained from the devices may beinaccurate during an acute illness.Insulin dosing and other treatmentswill only be based upon FDA hospitalapproved point of care blood glucosemonitoring device results and notpersonal Continuous GlucoseMonitoring devices.3
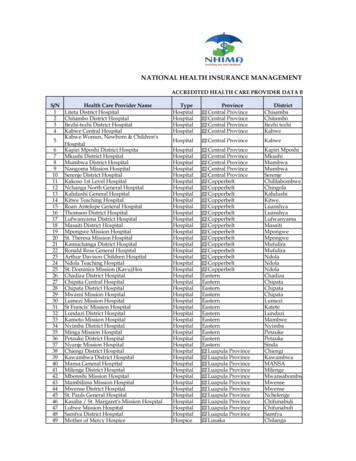
How to ReducePatient Surprise BillingI’m sure that all of you have heard a news story regarding“surprise medical billing,” when patients face oftenexorbitant costs after they unknowingly receive care froman out-of-network doctor or hospital. Another componentof surprise medical bills is known as “balance billing”which is an additional amount, perhaps representingfull charges, that the out-of-network physician or otherprovider may bill the patient directly. Because doctors haveno contractual obligation with an insurance company, patients can be liable for the “balance bill.” In addition to attentionfrom the media, surprise medical billing and its impact on patients has garnered regulatory interest by healthcarestakeholders, federal and state governments.In the past, St. Clair patients have not experienced the types of impact that attracted media attention. Each practicehas been very conscientious toward making sure they participate with insurances that match the needs of their patients.St. Clair previously communicated to you the various managed care products which St. Clair has a contract. Also, thetransparency initiatives on our website for Patient Estimates provides our patients with information on managed careproducts. We want to continue to achieve transparency and reach out to all physicians who have privileges at St. Clairto reiterate the plans that St. Clair accepts. Our patients would certainly benefit if we were able to completely eliminatesurprise billing.Please review the list of insurance contracts below to understand if your practice is in-network for services at St. Clair.A list of St. Clair’s Contracted Payers can also be found on our website (stclair.org). You can click on Billing & Insurancetab and then Participating Insurance Plans tab for a full list of contracted providers.St. Clair Out-Of-Network Insurance Products UPMC Advantage - Partner Network (Bronze/Silver/Gold/Platinum Plans) UPMC Advantage - Select Network (Bronze/Silver/Gold/Platinum Plans) Highmark - Together Blue EPO (Bronze/Silver/Gold Plans)St. Clair In-Network Insurance ProductsMedicare and Medicare Advantage Products Traditional Medicare Aetna/Coventry HealthAmericaAdvantra Plans AmeriHealth CaritasMedicare Advantage Cigna – bravo Health Springs Gateway HealthMedicare Assured Highmark:-Community Blue-Medicare HMO-Security Blue HMO-Freedom Blue HMO Humana Medicare Plans PA Health and WellnessHealthChoices Plan United HealthCare:-United Healthcare-Medicare Complete-United Healthcare Dual UPMC Health Plan:-UPMC for Life-UPMC for Life Dual-UPMC for Life HMO-Premier Rx Western PAMedicare AdvantageUPMC Community CaresMedicaid And Managed Medicaid Products Traditional Medicaid Medicaid HealthChoices Plan (Adult Benefit Package) Gateway Health Medicaid United Healthcare Community Plan UPMC for You UPMC Community HealthChoices Plan PA Health and Wellness Community HealthChoices Plan AmeriHealth Caritas Community HealthChoices PlanContinued to pg. 54Physician’s Focus Spring 2020
Continued from pg. 4St. Clair In-Network Contracts ContinuedCommercial/Employer Sponsored Products Aetna (individual/employer provided) Aetna Pennsylvania EmployeeTrust Fund (PEBTF) custom HMO network Cigna (individual/employer provided) Cigna Behavioral Health Community Care Behavioral Health HealthAmerica (individual/employer provided) Highmark including (individual/employer provided):-Community Blue (managed care plan)-Community Blue Flex-Connect Blue-DirectBlueFederal Marketplace Products (ACA) Aetna-Coventry (Bronze/Silver/Gold Plans) UPMC Advantage - Premium Network(Bronze/Silver/Gold/Platinum) United Healthcare:-UMR-Catalyst-Choice-Choice Plus-HRA-HSA-United Behavioral Health UPMC Health Plan (individual employer provided) UPMC My Care Advantage Value Options (behavioral health plan) Highmark:-Connect Blue-Blue Cross Blue Shield Shared Cost-Health Savings Blue & Embedded Blue-Comprehensive Care Blue & Flex Blue-my Direct Blue EPO & HMO(Bronze/Silver/Gold Plans)New Appointed PhysiciansEmily E Abbott, D.O.Emily E Gleason, M.D.Orthopaedic Specialists - UPMCOrthopaedic SurgerySt. Clair Family Practice AssociatesFamily MedicineTala Achkar, M.D.Calin Gorun Gorunescu, M.D.Richard J Oh, M.D.vRadRadiologyAlanna Carol Peterson, M.D.UPMC Emergency MedicineEmergency MedicineIntegrated Cancer ServicesHematology & OncologyKeystone Anesthesia Consultants, LTDAnesthesiologyDeborah Brooks, M.D.Crystal-Dawn L Gunsch, DPMKeystone Anesthesia Consultants, LTDAnesthesiologyAvery C Capone, M.D.Christina L Johnson, DPMThe Health Center for Integrative MedicineFamily MedicineSarahgene G DeFoe, M.D.Clarence D Lin, M.D.Orthopaedic SpecialistsOrthopaedic SurgerySt Clair Emergency MedicineEmergency MedicineR.A. Capone Jr MD OCPlastic Surgery, Hand Surgery, SurgeryThe Orthopedic GroupPodiatric SurgeryGreentree Foot and AnklePodiatric SurgeryIntegrated Cancer ServicesRadiation OncologyRipepi Surgical AssociatesSurgeryAndrew Joseph Gentilin, M.D.Reed Z Louderback, M.D.Keystone Anesthesia Consultants, LTDAnesthesiologyMichael Todd Rice, M.D.Janine K Rihmland, M.D.Thomas R Zink, D.O.UPMC Emergency MedicineEmergency Medicine5
Documentation TipSufficient Documentation of AcuteRespiratory FailureRecent Denial Statistics for St. Clair HospitalJanuary 1, 2019 -June 30, 2019 24% of the total clinical validation denials were forAcute Respiratory Failure.July 1, 2019 – Dec. 5, 2019 30% of the total clinical validation denials were forAcute Respiratory Failure.*Denied for "Insufficient Clinical Evidence and Supportive Documentationto substantiate the coding of this condition"Does your documentation representthe severity of your patient’s AcuteRespiratory Failure? Auditors look forspecific documentation in a chart tosupport this diagnosis. Below are someclinical indicators to consider adding todocumentation if present in your patient.Clinical Indicators: dyspnea, tachypnea,decreased respirations, wheezing,labored breathing, nasal flaring, grunting,accessory muscle use, retractions,cyanosis, speaking in shortened sentences,ABG values, SpO2 %, changes frombaseline for chronic pulmonarydisease patients.6Physician’s Focus Spring 2020
St Clair HospitaleConsult Guide1. The Mayo eConsult Process-Who is it for?DiagnosismanagementAny St. Clair physicianTreatmentoptionsAny patient who requests a Mayo eConsult or asksfor a second opinion. (eConsult service is free for patients ofSecondopinionSt. Clair)2. The Mayo eConsult Process-How to Submit-2 options(·c;i ·:.ClairnetOn the Clairnet home page,select "Mayo Clinic CareNetwork" on the top left.On the following screen,select "eConsult request."'Home,DepartmCl.tlrnetrirfil MAYO CLI IC'\}" CARE ETWORKDIeConsult Request(PHYSICIAN ONLY)Consult with Mayo Clinic specialistsand subspecialists Oil pabent cases.MemberAskMayoExpert IDirect CommunicationContact the Quality Department:Phone: 412.942.2260Email: mayo.inquiries@stclair.orgSpecific QuestionClinical Summary of PatientDocumentation needed7
Expected Date of Discharge (EDOD) OverviewLive in SCM December 17th, 2019What is Expected Date of Discharge (EDOD)?How is the EDOD predicted?The EDOD is a predicted date of discharge based on average nationalperformance for similar patients. The goal is to discharge on orbefore the EDOD.EDOD will only display for patients currently in an Inpatient Statuswith a Total LOS equal to or greater than 24 hours AND sufficientdocumentation to make a prediction.Day of Admission Day 0Will it be perfect?NO! It is a tool in our toolbox to proactively identify a date that theclinical team can work toward. It is only as good as the documentationthat goes into it.Will it be communicated to patients & families?Eventually. First we will ensure our clinical team is comfortable withthe tool and prepared for the dialogue with patients. There will bephase 2 education prior to patient/family involvement.Questions? Please contact any memberof the Care Progression Delivery Teamor kaitlin.shotsberger@stclair.orgHow will it be displayed?Quality Performance DashboardIDEAS for theNEXT ISSUE?Contact The QualityDepartmentVictoria g412.942.2264Linda Lattner, Corporate Compliance Officer,Compliance Line 1.800.218.8538. For any questionsor concerns about unethical, illegal or improperconduct. Calls can be made confidentially, anonymouslyand can not be traced or recorded. All calls are takenseriously and investigated by the Compliance Officer.
Gateway HealthMedicare Assured . -Medicare Complete -United Healthcare Dual UPMC Health Plan: -UPMC for Life -UPMC for Life Dual -UPMC for Life HMO -Premier Rx Western PA Medicare Advantage UPMC Community Cares Continued to pg. 5 Traditional Medicaid Medicaid HealthChoices Plan (Adult Benefit Package) Gateway Health .