Transcription
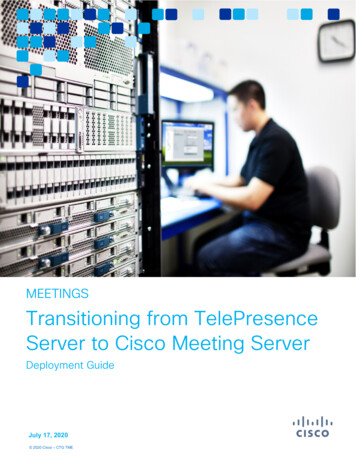
PROVIDER ENROLLMENT 101MARCH 2019Alisha Sanders, CMSDirector, Division of Enrollment OperationsMarian Love, First Coast Service OptionsProvider Enrollment DirectorLucas Dockter, NoridianProvider Enrollment Operations Supervisor
OverviewMorning Session Introduction to Medicare Provider Enrollment Overview Submission Intake Processing, Screening and Verification Finalization and ClaimsAfternoon Session Provider Enrollment PolicyCMS National Provider Enrollment Conference March 2019 2
PollQuestion 1CMS National Provider Enrollment Conference March 2019 3
PollQuestion 2CMS National Provider Enrollment Conference March 2019 4
Introduction toMedicareCMS National Provider Enrollment Conference March 2019 5
What is Medicare?Medicare is a federal health insurance program for: People 65 and older, Certain younger people with disabilities, and People of any age with End-Stage Renal DiseaseDifferent parts of Medicare help cover specificservices (A, B, C and D)CMS National Provider Enrollment Conference March 2019 6
Medicare Part A (Hospital Insurance)Part A covers inpatient hospital stays, care in a skillednursing facility, hospice care, and some home health care Hospital Federally Qualified Health Center Community Mental Health Center Skilled Nursing Facility Home Health AgencyCMS National Provider Enrollment Conference March 2019 7
Medicare Part B (Medical Insurance)Part B covers certain doctors' services, outpatientcare, medical supplies, and preventive services Physician/Non-Physician Practitioner Services Clinic/Group Practices Independent Diagnostics Testing Facilities (IDTF) Durable Medical Equipment, Prosthetics, Orthotics,and Supplies (DMEPOS) suppliers Medicare Diabetes Prevention Program (MDPP)suppliersCMS National Provider Enrollment Conference March 2019 8
Medicare Part C (Medicare Advantage Plans)Part C provides Part A and Part B benefits offered bya private company that contracts with Medicare Health Maintenance Organizations Preferred Provider Organizations Private Fee-for-Service Plans Special Needs Plans Medicare Medical Savings Account PlansCMS National Provider Enrollment Conference March 2019 9
Medicare Part D (Prescription Drug Coverage)Part D offers coverage for prescription drugs Original MedicareSome Medicare Cost PlansSome Medicare Private Fee-for-Service PlansMedicare Medical Savings Account PlansCMS National Provider Enrollment Conference March 2019 10
PollQuestion 3CMS National Provider Enrollment Conference March 2019 11
What is a Medicare Administrative Contractor (MAC)?A private health care insurer that has been awardeda geographic jurisdiction to: Enroll providers in the Medicare program Process Medicare claims (Part A/B and DME) Respond to provider inquiries Educate providers about Medicare billing requirementsCMS National Provider Enrollment Conference March 2019 12
A / B MACsCMS National Provider Enrollment Conference March 2019 13
Home Health & Hospice MACsCMS National Provider Enrollment Conference March 2019 14
What is the National Supplier Clearinghouse (NSC)? National contractor responsible for enrolling all DMEsuppliers Ensures that DME suppliers meet and maintain all Federaland State requirements to bill the Medicare program Claims are processed by 4 DME MACsCMS National Provider Enrollment Conference March 2019 15
DME MACsCMS National Provider Enrollment Conference March 2019 16
Question& Answer SessionCMS National Provider Enrollment Conference March 2019 17
Provider EnrollmentOverviewCMS National Provider Enrollment Conference March 2019 18
Provider Enrollment Regulations / StatutesEstablishes enrollment requirements, conditionsfor participation and payments The Social Security Act (1861) Federal regulations (42 CFR 424) Program Integrity Manual 100-08, Chapter 15CMS National Provider Enrollment Conference March 2019 19
How Enrolling WorksMedicareProviders& Suppliersw/NPIUpdate Claim System855Form60 days*Online45 daysDevelopmentLetter MAC UpdatesClaim System (1-2 days) Provider not approveduntil claims updated MAC Mail Room Manual Data EntryMAC Recommendationto State/RO Certifiedproviders/suppliers MAC recommends to RO RO performsin 3-9 monthsDirect Input Signed and DatedApp Fee (or Waiver)Supporting DocsAll Data Elements Name / LBNSSN / DOBNPPESAddress License AdverseActions Fingerprints Site Visits* If the app is complete, and no site visitCMS National Provider Enrollment Conference March 2019 20
SubmissionMedicare Providers & Suppliers w/NPI855Form60 days*Online45 days* If the app is complete, and no site visitCMS National Provider Enrollment Conference March 2019 21
National Provider Identifier Type 1Individual healthcareproviders(i.e., physicians,dentists,chiropractors,physical therapists) Type 2Organizationalhealthcare providers(i.e., hospitals, homehealth agencies,clinics, labs, grouppractices, suppliersof durable medicalequipment)Providers must obtain an NPI prior to enrollingin the Medicare Program.Healthcare providers can apply for NPIsin one of three ways: Online via National Plan & Provider EnumerationSystem (NPPES) Paper NPI Application/Update Form (CMS-10114) Electronic File Interchange (EFI) whereby an approvedEFI Organization can submit the healthcare provider’sapplication on their behalf (i.e., through a bulkenumeration process).NPPES Registry (for online stry/NPIRegistryHome.doCMS National Provider Enrollment Conference March 2019 22
Taxonomy Codes vs. Specialty TypesTaxonomy Codes Providers select a taxonomy code when applying for an NPI Uniquely identifies providers in order to assign them NPIs, notto ensure that they are credentialed or qualified to render health care May or may not be the same category used by Medicarefor enrollment purposesSpecialty Types Self-designated on the CMS-855 application Describes the specific type of medical practice or services provided Used by CMS for enrollment and claims processingCMS National Provider Enrollment Conference March 2019 23
Taxonomy / Specialty Crosswalk CMS crosswalks the types of providers/supplierswho are eligible to enroll in Medicare with theappropriate taxonomy codes Can be accessed at E-PROVIDER-SUPPLIER-toHEALTHCARE/j75i-rw8y Updated on a quarterly basisCMS National Provider Enrollment Conference March 2019 24
CMS-855 Enrollment Applications CMS-855AInstitutional Providers (Part A) CMS-855BClinics/Group Practices and Certain Other Suppliers(Part B, non-DME Suppliers) CMS-855IPhysicians and Non-Physician Practitioners(Part B, non-DME Individuals) CMS-855RReassignment of Medicare Benefits(Supplemental to CMS-855I form) CMS-855SSuppliers of Durable Medical Equipment, Prosthetics,Orthotics, and Supplies (DMEPOS) (Part B, DME Suppliers)) CMS-855OEligible Ordering, Referring and Prescribing Physiciansand Non-Physician Practitioners(Part B , Part-D and non-DME Individuals) CMS-20134Medicare Diabetes Prevention Program (MDPP) Suppliers(Part B, non-DME Suppliers)CMS National Provider Enrollment Conference March 2019 25
Authorized and Delegated OfficialsEnroll, make changes and ensure compliancewith enrollment requirementsAppointed by the AO with authority to reportchanges to enrollment information CEO, CFO, partner, chairman, owner,or equivalent appointed by the org May sign all applications(must sign initial application) Approves DOs Ownership, control,or W-2 managing employee Multiple DOs permitted May sign changes, updates & revalidations(cannot sign initial application)CMS National Provider Enrollment Conference March 2019 26
Who Can Sign the Enrollment Application?Initial:All:Adding:Changes& Revals:Changing / Terminating:CMS National Provider Enrollment Conference March 2019 27
Application FeesApplication fee for 2019 is 586Refund Request Supports provider enrollment and screening activities Required for institutional providers when initiallyenrolling, revalidating or adding a practice locationHome Health Agencies, DME supplier, Hospital, IDTF Application fee varies from year-to-year Must be paid electronically via PECOS Credit or debit card (no checks permitted) MACs will develop for missing applicationfees and reject the application if not submittedwithin 30 daysA refund may be issued if 1.A hardship exception request is approved2.The application was rejected prior to the MAC’sinitiation of the screening process3.The application denied due to temporary moratorium4.Fee not required for the transaction in question or notpart of an application submissionCMS National Provider Enrollment Conference March 2019For information on which actions trigger the applicationfee requirement by provider/supplier type refer to theApplication Fee Matrix on CMS.gov.Pay the application fee e.do 28
PollQuestion 4CMS National Provider Enrollment Conference March 2019 29
CMS-588Electronic Funds Transfer (EFT) Agreement All providers must receive Medicare payments via EFT Must include a copy of a voided check or bank letterverifying account information Providers who reassign all of their benefits to a groupare not required to submit an EFT agreementCMS National Provider Enrollment Conference March 2019 30
CMS-460Participation AgreementParticipationNonparticipation Medicare reimbursementis 5 percent higher thannonparticipating physiciansand other suppliers Medicare reimbursementis 5 percent lower thanparticipating physiciansand other suppliers Medicare issues paymentsdirectly to you because theclaims are always assigned You cannot charge thebeneficiary more than thelimiting charge, 115 percentof the Medicare PhysicianFee Schedule amount You may accept assignmenton a case-by-case basisCMS National Provider Enrollment Conference March 2019 31
CMS-855Submission Reasons New Enrollee (Initial) Change of Information Revalidation Reactivation Voluntary WithdrawalCMS National Provider Enrollment Conference March 2019 32
New Enrollee (Initial) Welcome to Medicare! You are submitting an application to initiallyenroll in the Medicare program or to initiallyenroll in a new MAC jurisdiction Must submit a complete applicationCMS National Provider Enrollment Conference March 2019 33
PollQuestion 5CMS National Provider Enrollment Conference March 2019 34
Question& Answer SessionCMS National Provider Enrollment Conference March 2019 35
Intake MAC Mail Room Manual Data EntryDirect InputCMS National Provider Enrollment Conference March 2019 36
Receipt Date DeterminationReceipt date is important in determining youreffective datePaper Applications Based on the date the MAC receivedthe package in the mail MACs will no longer accept handwrittenapplications (late 2019)Web Applications (October 2018) Based on the date the MAC received the websubmission in PECOS Must be e-signed or signature uploadedCMS National Provider Enrollment Conference March 2019 37
Impacts to Receipt DateFingerprints The date fingerprint results are receivedHardship Waiver Approval The date CMS notifies the MAC thatthe hardship waiver is approvedCMS National Provider Enrollment Conference March 2019 38
PollQuestion 6CMS National Provider Enrollment Conference March 2019 39
Medicare Effective Dates Part BEffective date is the later of: Application Receipt Date Date of first services at a new location (up to 30 days prior to application receipt)Option A: Early SubmissionPhysicians / Groupscan apply 60 days prior ** MACreceivesappAPR 1MARProvider seeking effective dateJUNE 1MACapprovesMAY 15(w/ effectiveJune 1)MAC PROCESSINGAPRMAYJUNProvider performsserviceJUNE 1JULAUGSEPOCTMAC PROCESSINGOption B: Late SubmissionPhysicians / Groupseffective date up to 30 days prior to submission date ***ProviderperformsserviceJUNE 1MACreceivesappJULY 1MACapprovesSEPT 1(w/ effective June 1)** Must be in compliance at requested effective date (operational, licensed)CMS National Provider Enrollment Conference March 2019 40
Medicare Effective Dates Part BScenarioEffective Date Application receipt date of 6/10/19with app requested date of 7/01/19 7/01/19 (no retro, based on requestedeffective date on application) Application receipt date of 6/10/19with app requested date of 6/01/19and all requirements met 6/01/19(based on requirements met date) Application receipt date of 6/10/19with app requested date of 3/01/19 5/11/19(30-day retro) Application receipt date of 6/10/19with app requested date of 6/01/19,license effective date 6/28/19 6/28/19(based on license effective date)CMS National Provider Enrollment Conference March 2019 41
Medicare Effective Dates Part BIndependent Diagnostic Testing Facility (IDTF) The later of: (1) the receipt date of theapplication or (2) the date all Medicarerequirements were metOrdering and Referring Only Providers (CMS-855O) Receipt date of the applicationCMS National Provider Enrollment Conference March 2019 42
Medicare Effective Dates Part AProvider seeking effective dateSEPT 1Hospitals / HHAs / SNFscan apply up to180 days prior **MACreceives appAPR 1MAC recommendsapproval toState/ROJUNE 1PROCESSINGAPRState surveycompletedDEC 1RO approves,w/ effective date DEC 1when RO determined allrequirements were metSTATE/RO PROCESSINGJUNSEPTDECJANAPR ’19** Must be in compliance at requested effective date (operational, licensed)CMS National Provider Enrollment Conference March 2019 43
Question& Answer SessionCMS National Provider Enrollment Conference March 2019 44
Processing, Screening and VerificationMedicareProviders& Suppliersw/NPIDevelopmentLetter CMS National Provider Enrollment Conference March 2019Signed and DatedApp Fee (or Waiver)Supporting DocsAll Data Elements Name / LBNSSN / DOBNPPESAddress License AdverseActions Fingerprints Site Visits 45
What Causes Delays? Missing Documents30-35%delayedIRS documents, CMS 588 EFT, voided check,bank letter, education documentation,par agreement, cert term page, org charts Missing Fields (missing signature/date) Wrong Signature (paper)need at least1 round of corrections Incorrect Information Missing Application FeeHow the MAC develops for missing informationContacts the By 1. Contact person (sec 13) 2. Individual provider (sec 2)3. Authorized or Delegated Official (sec 15/16)CMS National Provider Enrollment Conference March 2019emailfaxphoneletter30days torespondNo response? delays rejections later effective date 46
PollQuestion 7CMS National Provider Enrollment Conference March 2019 47
MAC Notification LettersWho is listed on MAC notification letters?MAC analyst isthe point of contactlisted on the letterCMS National Provider Enrollment Conference March 2019MAC call center isthe point of contactlisted on the letter 48
How Addresses are UsedCorrespondenceMedical RecordCorrespondencePractice LocationUsed to contact theprovider directlyUsed to requestdocumentationWhere you renderservices to beneficiaries Approval letters Medical records Revalidation notices Site visit Revalidation notices Revocation lettersCMS National Provider Enrollment Conference March 2019 49
How Addresses are UsedPrimary PracticeLocation (855R)Special PaymentContact PersonWhere you renderservices most ofthe timeWhere all otherpayment informationis sentPerson to contactregarding yourapplication PhysicianCompare Revalidationnotices Remittancenotices Paper checks Developmentrequests Approval lettersCMS National Provider Enrollment Conference March 2019 50
Contact Person Any contact listed on an enrollment record mayrequest a copy of approval and revalidation letters MAC will send by email fax mail (excludes certification letters or Tie In noticesissued by Regional Office)How to end date a contact person?Requests may be submitted by By 1.Current Contact person (sec 13)1.email2.Individual provider (sec 2)2.fax3.Authorized or Delegated Official (sec 15/16)3.letterCMS National Provider Enrollment Conference March 2019Addition of contact persons must stillbe reported on appropriate CMS-855 51
Certification Statement RequirementsCMS National Provider Enrollment Conference March 2019 52
Screening LevelsScreening level may beelevated to “high” if: Excluded fromMedicare/other FederalHealth Care program Terminated from Medicaid Applied for Medicare within6 months after temporarymoratorium Within the last 10 years,you had: Medicare paymentsuspension Medicare billingprivileges revoked Final adverse action(s)WHO?e.g. Newly enrollingDMEPOS and HHAs,MDPPHIGHWHO?e.g. Ambulance,IDTF, CMHC, CORFMODERATEWHO?e.g. Phys, Non Phys,FQHC, Group PracticeCMS National Provider Enrollment Conference March 2019LIMITEDSUBJECT TO LIMITED &MODERATE REQUIREMENTSAND FINGERPRINTSSUBJECT TO LIMITEDREQUIREMENTSAND SITE VISITVERIFICATION OFLICENSURE ANDDATABASE CHECKSRISK CATEGORY 53
Site Visits National Site Visit Contractor (NSVC) All enrollment site visits conducted by the NSVC(except Durable Medical Equipment (DME) suppliers) Required for moderate/high risk providers- initial enrollment, revalidation, adding a new location CMS has the authority to perform site visits on all providers Verifies practice location information to determinecompliance with enrollment requirements Separate from state site visits for certified providersWhat to expect during a site visit?1. An external or internal review, by an inspector, with limited disruption to your business2. Photographs of the business3. Inspector will possess a photo ID and a letter of authorization issued and signed by CMS To verify that an inspector is credentialed to perform a site visit contact MSM SecurityService, at 1-855-220-1071.Refer to SE1520 on CMS.gov for more informationCMS National Provider Enrollment Conference March 2019 54
Site Visits National Supplier Clearinghouse (NSC) All DME supplier enrollment site visits conducted by the NSC Required for initial enrollments and revalidation Verifies compliance with supplier standards: Hours of operation Licenses/certifications Patient records Proof of business records (rental agreements) InventoryWhat to expect during a site visit?1. An internal review by an inspectorInspector will possess:2. Photographs of the business Photo identification3. Staff interviews Letter stating reason for the visit signedby the NSC manager Site visit acknowledgment form(signed by the supplier attesting the visit was completed)CMS National Provider Enrollment Conference March 2019 55
Fingerprinting5%( ) Ownership/Partnersin a high risk provider/supplierCMSfingerprinting.com Letter will be sent giving 30 daysto get fingerprintedApplies to: Medicare phased rollout New HHAsIf the provider/supplier: New DME suppliers New MDPP suppliers High risk providers/suppliersExcludes: Managing Employees Has a felony conviction Refuses fingerprintingThen CMS may deny the application,or revoke their billing privileges Officers DirectorsIf the initial fingerprints are unreadable a 2ndset of fingerprints will be requestedCMS National Provider Enrollment Conference March 2019 56
PollQuestion 8CMS National Provider Enrollment Conference March 2019 57
Question& Answer SessionCMS National Provider Enrollment Conference March 2019 58
PROVIDER ENROLLMENT 101Joseph Schultz, CMSTeam Lead, Division of Enrollment OperationsWilliam Price, National Government ServicesProvider Enrollment Process Expert
Finalization and ClaimsUpdate Claim System MAC UpdatesClaim System (1-2 days) Provider not approveduntil claims updatedMAC Recommendationto State/RO Certifiedproviders/suppliers MAC recommends to RO RO performsin 3-9 monthsCMS National Provider Enrollment Conference March 2019 60
Approved The enrolling provider / supplier has been determinedto be eligible under Medicare rules and regulationsto be granted Medicare billing privileges Provider is not approved until claims system is updated(within 1 – 2 days) Approval letter is sent to the contact person. If nocontact person is listed the letter is sent to the providerat their correspondence addressCMS National Provider Enrollment Conference March 2019 61
PollQuestion 9CMS National Provider Enrollment Conference March 2019 62
What is a PTAN? A Medicare-only number issued to providersupon enrollment to Medicare Used to authenticate the provider when using theInteractive Voice Response (IVR) phone system,internet portal or on-line application status The PTAN's use should generally be limitedto the provider’s contact with their MAC The NPI must be used to bill the Medicare programCMS National Provider Enrollment Conference March 2019 63
Physician / Non-Physician PTANs Individuals are assigned PTANs based on their privatepractice and group affiliations (i.e. sole proprietor,reassignment of benefits) Individuals who reassign their benefits receive a memberPTAN for each group PTAN they reassign to A sole owner would have a Group PTAN assigned for thebusiness and a member PTAN for themselvesCMS National Provider Enrollment Conference March 2019 64
Group / Supplier PTANs PTANs are assigned per EIN, per State An existing provider would require a new PTAN if: Adding a new location in a different payment localityin the same State Enrolling a different provider type Exception: Hospitals that receive a PTAN perdepartmentCMS National Provider Enrollment Conference March 2019 65
What is a CCN? A CCN is a CMS Certification Number issuedto Part A/B certified providers Used for verifying Medicare certification, assessment-relatedactivities and communications The CMS RO assigns the CCN 6 or 10 digits The first 2 digits identify the state in which the provider is located The last 4 digits identify the type of facilityCMS National Provider Enrollment Conference March 2019 66
PollQuestion 10CMS National Provider Enrollment Conference March 2019 67
Understanding the TIN / NPI / PTAN RelationshipTIN to NPI to PTAN – Part A & B (non-DME)PTAN 1MDMDPI 2TIN(Organization)PTANTIN(Individual)PTAN 2MD - 2FLEnrollment Record(855I)FLEnrollment Record(855A & B)PTAN 3PTAN 4CMS National Provider Enrollment Conference March 2019 Organizations can have multipleenrollments per state Organizations can have multiple NPIs Individuals can only have one NPI 68
Understanding the TIN / NPI / PTAN RelationshipTIN to NPI to PTAN – Part B (DME)PTAN 1MDPI 2TIN(Organization)PTAN 2MD - 2PTAN 3MD - 3Enrollment Record(855S)CMS National Provider Enrollment Conference March 2019 Organizations can have multipleenrollments per state DME suppliers can only have one locationper enrollment A separate NPI is required per enrollment 69
Returns Unsolicited revalidation application Sent to incorrect contractor Submitted more than 60 days prior to the effective date Part A certified providers, Ambulatory Surgical Centers (ASCs)and Portable X-ray Suppliers (PXRS) applications submittedmore than 180 days prior to the effective date Submitted an application prior to the expirationof a re-enrollment bar Submitted an application prior to the expiration of the appealwindow for a previously denied application Entire fields or sections hand-written on the application (late 2019)CMS National Provider Enrollment Conference March 2019 70
How to Avoid a Return If submitting via paper be sure to sendto the correct MAC Don’t submit applications more than 60or 180 days in advance of the effective date Don’t submit a revalidation more than 7 monthsin advance of your revalidation due date Don’t submit the application multiple times Use the fillable CMS-855 form optionCMS National Provider Enrollment Conference March 2019 71
Rejections Failure to provide complete information within30 days of the MAC’s request Missing information/documentation Unsigned, undated certification statement Old version of the CMS-855 application Incorrect application submitted Failure to submit application fee Failure to submit all required forms(e.g. CMS-855Rs for group enrollments)CMS National Provider Enrollment Conference March 2019 72
How to Avoid Rejections Don’t delay in responding to the request forinformation from your MAC Contact your MAC if you aren’t sure what youneed to do to return accurate correctionsCMS National Provider Enrollment Conference March 2019 73
Denied The enrolling provider is ineligible to receive Medicarebilling privileges Denial letter will include appeal rights A new enrollment application cannot be submitted until: Appeal rights have lapsed, or Notification received that the determination wasupheldCMS National Provider Enrollment Conference March 2019 74
Question& Answer SessionCMS National Provider Enrollment Conference March 2019 75
Other Submission TypesCMS National Provider Enrollment Conference March 2019 76
Changes of Information You are submitting an enrollment application to notifyMedicare of a change(s) to your enrollment informationCMS National Provider Enrollment Conference March 2019 77
Changes of Information Within 30 days Change of ownership or control, including changes inauthorized or delegated official(s) Adverse Legal Action (e.g., suspension or revocationof any state or Federal license) Change in practice location(includes any new reassignments) Within 90 days All other changes to enrollmentNote: Timeframes may vary by provider type.Refer to SE1617 on CMS.gov for more informationCMS National Provider Enrollment Conference March 2019 78
When to Select Change / Add / Delete 1.Applicable CMS-855 sections (change/add/delete options)2.Location information (855A/855B/855I/855S)3.Ownership/Managing Control (855A/855B/855I/855S)4.Billing Agency (855A/855B/855I/855S)5.AO/DO (855A/855B/855S)6.Attachments 1&2 (855B)CMS National Provider Enrollment Conference March 2019Replace existing information with new information(ex. practice location, ownership )Update existing information(ex. change in suite #, telephone #)App fee is not requiredAdd additional enrollment informationto existing information (practice locations)App fee is requiredRemove existing enrollment informationApp fee is not requiredDeleting a practice location in PECOS removesthe special payment address and requires re-entryFor information on which actions trigger theapplication fee requirement by provider/suppliertype refer to the Application Fee Matrix on CMS.gov.Refer to SE1617 for reporting requirements 79
Revalidation Verify the accuracyof your enrollmentinformation thatexists on filewith Medicare DME suppliersrevalidate every3 years and all otherproviders/suppliersevery 5 yearsCMS National Provider Enrollment Conference March 2019 80
Reactivation You are returning to Medicare after a deactivation Must submit a complete CMS-855 to reactivate Effective date is based on the receipt date of the application 30 day retrospective billing permitted You will be issued a newProvider Transaction Access Number (PTAN) Except for deactivations due to non-responseto revalidationCMS National Provider Enrollment Conference March 2019 81
Voluntary Withdrawal You will no longer be rendering servicesto Medicare patients You are planning to cease (or have ceased)operations You are relocating to another state and no longerintend to practice in the current stateCMS National Provider Enrollment Conference March 2019 82
Opt-Out of MedicarePhysicians/practitioners who do not wish toenroll in the Medicare program may “opt-out”What this means: The physician/practitioner nor the beneficiarysubmits a bill and is reimbursed by Medicare forservices rendered (beneficiary pays out-of-pocket) A private contract is signed between thephysician/practitioner and the beneficiary The physician/practitioner submits an affidavitto Medicare to opt-out of the programCMS National Provider Enrollment Conference March 2019 83
Filing an Opt-Out Affidavit A standard CMS form is not available Some MACs have a form available on their website Must be filed withall MACs whohave jurisdictionover the claimsthe physician/practitionerwould haveotherwise filedwith MedicareCMS National Provider Enrollment Conference March 2019 84
Impacts of Opting-Out May not receive direct or indirect Medicare paymentfor services furnished to Medicare beneficiaries Cannot terminate early unless opting out for the first time andwithin 90 days after the effective date of the opt-out period Traditional Medicare fee-for- serviceUnder a Medicare Advantage planLocked in for 2 years if you miss the 90 day windowMay order or certify items and services or prescribePart D drugs for Medicare beneficiaries NPIDate of BirthSocial Security NumberConfirmation if an Office of Inspector General (OIG) exclusion existsCMS National Provider Enrollment Conference March 2019 85
Provider EnrollmentPolicyCMS National Provider Enrollment Conference March 2019 86
PollQuestion 11CMS National Provider Enrollment Conference March 2019 87
Physician Assistant Employer can bean Individual orOrganization Enroll in Medicare for services provided Establish an employer relationship using 855I (section 2E) Terminate an employer relationship using Section 2Fof 855I (PA) or Section 2G of 855B (Org) Individually enroll and receive direct payment(Payments made only to PA’s employer) Organize/in
Marian Love, First Coast Service Options. Provider Enrollment Director. Lucas Dockter, Noridian. . CMS-20134 Medicare Diabetes Prevention Program (MDPP) Suppliers (Part B, non-DME Suppliers) . Date of first services at a new location (up to 30 days prior to application receipt) .