Transcription
Chronic CareManagement (CCM) ToolkitYour implementation guide for patients with chronic conditions
Chronic Care Management ToolkitYour implementation guide for patients with chronic conditionsThank you for using the Chronic Care Management (CCM) Toolkit. This guide isintended to help you and your team implement or expand CCM for your targetedpatients with chronic conditions. You can either develop CCM processes with yourown team, or you can use this guide to help you form a collaborative partnershipbetween a physician practice and a local pharmacist.How to use this resource.1. Review the Overview Section on pages four through six.a. The Challengeb. Solutionc. Team Membersd. Requirements and Components of a CCM ProgramIndexOverviewThe ChallengeSolutionTeam MembersRequirements and Components of a CCM Program2. Identify your implementation team to develop your next steps.a. Your internal champion and team membersb. Community Pharmacist optionImplementation Strategies for a Successful CCM Program073. Assess Implementation Strategies for Successful CCM TrialMaximize Your CCM Program - Collaborate with a Pharmacist104. Choose individual Appendices for:a. Team toolsb. Easy-to-use templatesc. Supplemental CCM resourcesTeam Tools and Sample Templates125. Contact HQIN for technical assistance: CCM@hqi.solutions Appendix A: Sample CCM Care Plan TemplateAppendix B: Sample CCM WorkflowAppendix C: Sample CCM Care Team FlowAppendix D: General CCM BenefitsAppendix E: Pharmacy Partnership ChecklistAppendix F: CCM Management Trial AgreementAppendix G: Business Associate Agreement SampleAppendix H: CCM Coding and Billing DetailsAppendix I: Participating CCM Patient Log TemplateAppendix J: Considerations Prior to CCM ImplementationAppendix K: Supplemental CCM Resources204www.hqin.org 877.731.4746323
OverviewThe Challenge Chronic diseases are the leading causes of death and disability and accountfor 90% of the nation’s 3.8 trillion in health care expenditures. Currently, sixin 10 adults are living with at least one chronic disease, and four in 10 havetwo or more chronic conditions.1 Black and Hispanic Medicare patients havehigher prevalence rates of many chronic conditions (hypertension, diabetes,stroke, and depression) than their white counterparts2 and racial and ethnicminorities receive poorer care than whites on 40% of quality measures,including chronic care coordination and patient-centered care. People with chronic conditions often require care and support betweenphysician visits. Gaps in care may occur when that support is lacking dueto factors such as a person’s high-risk situation (i.e., uncontrolled bloodglucose levels), follow-up challenges, or even lack of services. That gapplaces people at risk for complications, worsening symptoms, and hospitalvisits. Clinicians are accountable for their patients’ chronic disease outcomes andclinical improvements. Programs and services need to be sustainable whileimpacting patient engagement, satisfaction, and outcomes.SolutionChronic Care Management (CCM) services offer routine non-face-to-face servicesto help Medicare beneficiaries who have multiple, significant chronic diseasesbetter manage their conditions. Refer to Appendix D for a summary of CCMbenefits.Implementing at least a four-month trial will enable your care team to experiencethe numerous benefits (summarized in Appendix D) along with enough datacollection to measure patients’ improved engagement and outcomes. When aphysician practice adds a community pharmacist to the team, the benefits can beeven greater.Team Members4 Qualified Healthcare Professionals (Physician, Physician Assistant, NursePractitioner) Clinical Staff (Pharmacist, Nurse, Social Worker) Non-Clinical Staff (Pharmacy Tech, Office Manager)Requirements and Components of a Chronic CareManagement ProgramPatient EligibilityChronic Care Management (CCM) services are available to Medicare beneficiarieswho have two or more chronic conditions expected to last at least 12 months,or until the death of the patient. To bill for the CCM services you provide to youreligible patients, various components must be in place to successfully implementyour CCM program in your practice. These components include:Patient ConsentBefore CCM services can be billed, either verbal or written patient consentmust be obtained. The patient must be informed about the services offered,applicable cost-sharing, and the right to end services. To prevent duplicatepractitioner billing, patients must be aware that only one practitioner canprovide and bill CCM services. Patient consent must be documented in themedical record, whether participation is acceptedor declined.Comprehensive Care PlanA “Comprehensive Care Plan” must be established, implemented, revisedand/or regularly monitored in an electronic format for the patient to trackhealth issues and share with their care team and/or caregiver as appropriate(See Appendix A for an example care plan template). For complex CCM,the care plan must be established or substantially revised. Some care planelements could include the following: Problem listExpected outcomes and prognosisMeasurable treatment goalsSymptom managementPlanned interventions and responsibilitiesMedication managementCommunity services ordersCoordination of services needed outside the practicePeriodic review of the care plan5
Continuity of CareContinuity of care for CCM recipients must be provided through adesignated care team member with whom the patient can scheduleappointments and who is in regular contact with the patient to help themmanage their chronic conditions.Electronic Health Records (EHRs)Certified Electronic Health Records (EHRs) must be used to record certainpatient data, including the patient’s demographics, medical problems,medications, and medication allergies. Your EHR can help to identify highrisk and at-risk patients for participation in your CCM program and help youto effectively manage chronic conditions and population health.24/7 Access to Care TeamCCM recipients must be provided with a way to contact their care teamregardless of the time of day or day of the week to address urgent caremanagement needs.CCM Care Team Roles and ResponsibilitiesLegend QHP requiredO Team members or QHPQualified HealthcareProfessionals (Physician,Physician Assistant, NursePractitioner)Clinical Staff(Pharmacist,Nurse, SocialWorker)Non-Clinical Staff(Pharmacy Tech,Office Manager)OOConsent Patient Collect Structured DataODevelop ComprehensiveCare Plan Maintain/Inform Updatesfor Care PlanOOManage CareOOProvide 24/7 Access to CareOODocument CCM ServicesOOBill for CCM Services Provide Support Services toFacilitate CCM6OImplementation Strategies for a SuccessfulCCM ProgramMost practices that implement CCM services do it within the confines oftheir own practices. An effective CCM program can increase your revenuepotential, maximize clinical outcomes, enhance practice efficiency, andimprove patient care. Below are seven key strategies to consider forimplementing a CCM in your practice.1. Establish a WorkflowIt is important to consider what your initial workflow may look like to meetthe requirements of the program, accommodate organizational capacities/resources and be able to generate revenue while also providing a high level ofcustomer satisfaction (See Appendix B for a sample workflow and AppendixC for care team workflow).2. Define your CCM ProcessBased on the initial workflow, practices and community partners should furtherdefine the who, what, when, and how. This will vary depending on individualorganizational variables. It is best to start small and improve over time. Forexample, start with one provider identifying higher risk patients with onedisease state that is typically associated with an additional chronic conditioncomorbidity and get comfortable with this before increasing scope. Identifyingthe initial CCM patient is important. Potential populations for considerationinclude: Patients with diabetes since they often have a secondary chronic condition New patients Dually eligible Medicare/Medicaid patients for co-pay coverage3. Prepare for ReimbursementCCM claims should be submitted timely each calendar month. It is importantto ensure your EHR/Practice Management system meets your billing needs andreimbursement staff are adequately trained to ensure proper reimbursement.O7
4. Establish Ongoing Monitoring and Quality ImprovementAs with all new endeavors, it is especially important to routinely measure andmonitor the new program to ensure that it is working as expected. Areas thatshould be monitored include: Staff/community partner comfort with process Patient satisfaction Billing and reimbursement Sustainability Consult the FQHC/RHC Care Management FAQOnce you have stabilized your processes and outcomes, consider spreadingthe scope of the services to other providers or additional populations.5. Identify Opportunities with Commercial PayersAlthough most of these tips are specific to the Centers of Medicare &Medicaid Services (CMS)-covered CCM services, it is important to exploreChronic Care opportunities with commercial payers. Some may have higherrates of reimbursement for more engagement with patients who have chronicconditions and sometimes with fewer requirements.6. Leverage Digital ToolsConsider using virtual or online platforms to reduce face-to-face visits forroutine chronic disease management. These digital tools can also be usedto arrange group visits for patients with similar chronic diseases focusing onbehavior change.7. Federally Qualified Health Centers (FQHC) andRural Health Clinics (RHC) CCM service can be billed using the general care management code G0511,either alone or with other payable services. If CCM services are billed on the same claim as an office visit, both will bepaid. 2021 payment rate remains at 66.77. Patient coinsurance and deductibles do apply. Special rules apply. Consult the FQHC/RHC Care Management FAQ for moreinformation. Principal Care Management (PCM) services can be done but only requireone chronic condition using same code (G0511).8Refer to Appendix J for an itemized checklist of specific items to considerwhen implementing a CCM program.8. CCM and Telehealth during a Public Health Emergency (PHE)Due to COVID-19, patients who have chronic conditions may have an increasedrisk for severe illness and even death if they are avoiding getting the carethey need including emergent care, routine screenings, and behavioral healthassistance.Because of the Public Health Emergency (PHE), an add-on G-code wasidentified by CMS as a “telehealth allowed service” and can meet the billingrequirements through an audio-only visit, (but only during the PHE). G0506should be billed separately from the monthly care management services codes.Please refer to the Federal Register for theMedicare Physician Fee Schedule Final RuleImpact of Public Health(pg. 80245) for specific guidance on the useEmergency on Chronic Care Needsof this code.40% decrease in treatmentDuring a PHE, actively screen for changesfor severe heart attackto behavioral health status includingdepression, anxiety, or substance abuse. It is600% increase in suicidecommon for patients to struggle with mentalhotline callshealth during periods of social isolationand anxiety, and these complications canEstimated 150,000 missedcreate negative clinical outcomes related tocancer diagnosesmanaging chronic care conditions.G0506: “Comprehensive assessment of and care planning by the physician or other qualified healthcare professional for patients requiring chronic care management services, including assessmentduring the provision of a face-to-face service” can be used when the beneficiary requires an “extensiveface-to-face assessment and care planning by the billing practitioner” and the “billing practitionerpersonally performs and meaningfully contributes to the establishment of the CCM care plan whenthe patient’s complexity warrants it.”9
Maximize Your CCM Program Collaborate with a PharmacistThe key to optimizing your CCM program is to partnerwith a pharmacist or local pharmacy. This collaborationengages partners to assist with a variety of CCM activities,many of which can be provided virtually such as medicationreview and reconciliation opportunities. This partnershipcan be easily implemented with a four-month trial to testprocesses, collect data and measure patient outcomes.Also, a trial demonstrates how your practice can provideCCM services to patients without additional burden andoverhead costs. Cost-sharing can be arranged whereCCM services can provide needed revenue to both thepractice and the pharmacist while improving chroniccare management for your most vulnerable patients. Itis important to establish the roles, responsibilities, andexpectations for each community partner you select foryour CCM program.To help facilitate this collaboration, refer to the PharmacyPartner Checklist in Appendix E for considerations whenselecting your partners.CCM Value Proposition for Pharmacist PartnershipIncreased Revenue 10 40- 100 per month per patientPotentially leads to incentive paymentEnhanced practice reputationNew patients, word-of-mouth recommendationsIncreases timely follow up when appointments are dueImproved Quality Measures & Patient Outcomes A1C 9.0%ImmunizationsTobacco screening and counselingBlood pressure screening and control Reduce patient phone calls for refillsEnhance referral follow-throughScreen/triage less serious patient issuesStreamline workflows resulting with a team-based modelCoordinate care through specialist notesand communicationImproved Practice EfficiencyImproved Patient Care Optimize team-based care model Increase access Strengthen coordination of care11
Team Tools and Sample Templates12
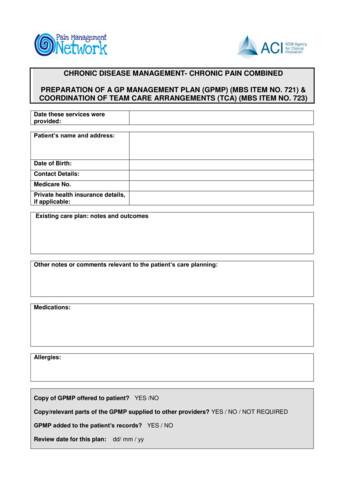
Sample CCM Care Plan TemplatePatient Name:Provider:Top Concern for Chronic Care Management: Diabetic condition management and patient self-monitoringExpected Outcomes: Improved patient self-monitoringImproved medication adherence and synchronizationImproved patient education related to diabetesActive patient medication list provided to physician using Blue Bag InitiativeSmoking cessation addressed and improvedMeasurement Improved: Improved BG levels and/or A1C Improved body size, weight, and/or compositionPlanned Interventions & Responsible Party: MD to provide initial labs, referrals and monitoring lipid levels Pharmacy to initiate and maintain regular monthly contact with patient Pharmacy to track monitoring vitals, BG levels, annual eye exam, and theimportance of foot exams Pharmacy to refer or provide diabetes self-management trainingopportunities for the patient Closing referral loops provided by pharmacy Preparation for medical appointments provided by pharmacy MD to review/edit care plan every six months based on outcomes andpatient needsProvider Signature:Appendix A
Sample CCM WorkflowID CCM EligiblePatientsConsider an InitialTrial: Dual EligibleDiabeticsSchedule visit(AWV, IPPE, TCM)Screen other needs &verify CCM eligibilityInitial AWV andSubsequent AWVsOther screening examples:DepressionAlcoholCognitiveDiabetesSmoking CessationF/U with provider reviewprior to billing codesObtain & Documentverbal or writtenconsent in patientchart and enrollProvider consents Pt.for CCM & briefly coversconcept and Care PlanCCMProviderPRACTICE:Billing provideror designatedclinical staffCCM visits/servicesdocumented in EHRProvider SignoffAppendix BCCM Services BilledMonthly for 99490PHARMACIST:Care Plane-prescribedas Rx by practice1st CCM Visit - BBComprehensiveMed ReviewBB BlueBag ProgramPredeterminedcost-sharingto Pharmacist
Sample CCM Care Team FlowCMS LicensedClinical StaffBilled CCM Code99490 MonthlyCare PlanCertifiedEHR DemographicsProblem ListMedications /Medication AllergiesBeneficiary writtenconsentDocumentation ofcommunications to/ from home andcommunity-basedprovidersPractitioner Care Team Conduct initialPreventative PhysicalExamConduct Annual WellnessVisit ORConduct Evaluation andManagement Visit (billedseparately) WrittenConsent Beneficiary Educate ElectronicUpdated at least annually 20 minutes CCM /month24/7 access for urgentneedsTelephone andasynchronousconsultationPost-discharge TCMER follow-up Coordinate referralsIdentify appropriateprovidersCapable of sharingelectronic care plan andelectronic summary carerecordMedication reconciliationCommunicate to / fromcommunity-basedprovidersOtherProvidersAccess to successive,routine appointmentsAppendix C
General CCM BenefitsImproved Patient-Centered Care Assist in the development and updating of the comprehensive care planProvide care management and coordination services to patientsEnsure an accurate comprehensive medication review and reconciliationProvide 24/7 access to chronic care management servicesIncreased Revenue Provider billing for initial comprehensive assessmentIncreased timely follow up when appointments are dueImproved practice reputation, new patient drawImproved quality metrics can lead to incentive payments (e.g., MACRA/MIPS)Improved Quality Measures Collect and record/relay structured data for documentation in the EHR Potential to improve key quality metrics and patient outcomesSaving Provider Time Home health collaboration - supplies, feedbackReferral follow-throughReduce phone calls/refill requests to practiceScreen/triage less serious patient issuesConsiderations prior to implementation – Refer to Appendix JAppendix D
Pharmacy Partnership ChecklistUse this checklist to facilitate pharmacy partner collaboration.Identify a potential partner (community pharmacy or primary care practice). If a local pharmacist is not available, schools of pharmacies may be able toassist. Pharmacists can also provide services remotely.Discuss a partnership opportunity to offer CCM.Agree to implement a four-month trial. Execute any necessary agreements. SeeAppendix F for a sample CCM Trial Agreement.Select the chronic condition of focus for the trial (i.e., diabetes for dual eligiblepatients).Identify eligible patients and create a referral process for the pharmacist orclinician. Providers can simply write a prescription for CCM services to the pharmacist.Decide what patient outcomes you will measure. Note: The outcomes may align with the practice quality and/orimprovement measures for the Medicare Quality Payment Program.Collaborate to develop a basic care plan that can be individualized, ifnecessary, and reevaluated at the end of the trial. See Appendix A for asample care plan.Clarify provider/practice responsibilities including: Identifying eligible patients, obtaining/documenting patient consent. Setting up the initial appointment with the pharmacist/pharmacy. Billing for the service and paying the pharmacist a pre-arranged consultantfee.The pharmacist responsibilities can include: Meeting with the patient monthly either in-person or by phone. Documenting a minimum of 20 minutes. Implementing the agreed-upon care plan. Providing monthly reports and invoices to the practice.Appendix E
Pharmacy Partnership Checklist (cont.)Use this checklist to facilitate pharmacy partner collaboration.Develop a communication process for the provider and the pharmacist. Forexample, use a secure fax line or grant the pharmacist access to the patientchart, portal or EHR.Decide how often you will communicate during the trial and evaluate areas forimprovement.Decide on a start/end date, and the number of patients that will be referredeach month.Establish Community Partner HIPAA agreement between practice andcommunity partner. See Appendix G for a sample agreement.Partner with the Health Quality Innovation Network (HQIN) for assistance withdata analysis and outcomes reporting or use a basic data collection template.Evaluate the outcomes and discuss how to expand, change, or end theprogram.Appendix E
Chronic Care Management Trial(Sample Agreement)Insert Pharmacy Name or Logo HereInsert Practice Name or Logo HereStart Date:End Date:Description of Trial: Patients from the practice who would benefit from ChronicCare Management and meet the trial inclusion criteria will be identified/consented byEnter Provider name herePatients would then be referred to Enter Pharmacist Name(s) Here who will act asclinical extenders for the practice implementing the patient care plan fromEnter Practice Name HerePharmacy will:1. Provide monthly data reports via the EMR (or other process as defined bythe practice) as well as invoices to Enter Practice Name(s) Here detailingthose trial patients who have received Chronic Care Management by thepharmacists.2. Provide services in person or by phone at Enter Pharmacy Name(s) Here orat Enter Practice Name(s) Here or at an agreed location that better suits thepatient.Practice will:1. Consent and refer patients.2. Bill Medicare for Chronic Care Management services.At the conclusion of the trial, analysis of the program will be discussed, and nextsteps decided.Financial Terms for Trial: Enter Pharmacy Name(s) Here would be compensatedfor Enter Agreed Upon % of the billable services for Chronic Care Management.Practice RepresentativePharmacist RepresentativeAppendix F
Business Associate AgreementSampleThis Agreement is made effective the day of , 20 byand between, hereinafter referred to as “Covered Entity, and, hereinafter referred to as “BusinessAssociate” or “Vendor”, (individually, a “Party” and collectively, the “Parties’’).WITNESSETH:WHEREAS, Sections 261 through 264 of the federal Health InsurancePortability and Accountability Act (HIPAA) of 1996, Public Law I 04191, known as “the Administrative Simplification provisions;” direct theDepartment of Health and Human Services to develop standards to protectthe security, confidentiality and integrity of health information; andWHEREAS, pursuant to the Administrative Simplification provisions, theSecretary of Health and Human Services has issued regulations modifying45 CFR Parts 160 and 164 (the “HIPAA Security and Privacy Rule’’); andWHEREAS, the Parties wish to enter into or have entered into anarrangement whereby Business Associate will provide certain servicesto Covered Entity, and, pursuant to such arrangement, BusinessAssociate may be considered a “business associate” of Covered Entityas defined in the HIPAA Security and Privacy Rule (the agreementevidencing such arrangement is entitled Legal Services Agreement, dated, and is hereby referred to as the “ ArrangementAgreement”); andWHEREAS, Business Associate may have access to Protected HealthInformation (as defined below) in fulfilling its responsibilities under sucharrangement;Appendix G
I. DEFINITIONSa. Except as otherwise defined herein, any and all capitalized terms in thisSection shall have the definitions set forth in the HIPAA Security andPrivacy Rule. In the event of an inconsistency between the provisionsof this Agreement and mandatory provisions of the HIPAA Security andPrivacy Rule, as amended, the HIPAA Security and Privacy Rule shallcontrol. Where provisions of this Agreement are different than thosemandated in the HIPAA Security and Privacy Rule but are nonethelesspermitted by the HIPAA Security and Privacy Rule, the provisions of thisAgreement shall control.b. The term “Protected Health Information”(PHI) means individuallyidentifiable health information including, without limitation, allinformation, data, documentation, and materials, including withoutlimitation. Demographic, medical, and financial information that relatesto the past, present, or future physical or mental health or conditionof an individual: the provision of health care to an individual; or thepast, present, or future payment for the provision of health care to anindividual: and that identifies the individual or with respect to whichthere is a reasonable basis to believe the information can be used toidentify the individual. “Protected Health Information “ includes withoutlimitation “’Electronic Protected Health Information” as defined below.c. The term “ Electronic Protected Health Information”’ means ProtectedHealth Information which is transmitted by Electronic Media (as definedin the HIPAA Security and Privacy Rule) or maintained in ElectronicMedia.d. Business Associate acknowledges and agrees that all ProtectedHealth Information that is created or received by Covered Entity anddisclosed or made available in any form, including paper record, oralcommunication, audio recording, and electronic dis p lay by CoveredEntity or its operating units to Business Associate or is created orreceived by Business Associate on Covered Entity’s behalf shall besubject to this Agreement.II. RESPONSIBILITIES OF THE PARTIES WITH RESPECT TO PROTECTIVEHEALTH INFORMATIONAppendix G
a. Business Associate agrees:i. to use or disclose any Protected Health Information solely: (I) formeeting its obligations as set forth in any agreements between theParties evidencing their business relationship, or (2) as required byapplicable law, rule or regulation, or by accrediting or credentialingorganization to whom Covered Entity is required to disclose suchinformation or as otherwise permitted under this Agreement, theArrangement Agreement (if consistent with this Agreement and theHIPAA Security and Privacy Rule), or the HIPAA Security and PrivacyRule, and (3) as would be permitted by the HIPAA Security andPrivacy Rule if such use or disclosure were made by Covered Entity:ii. at termination of this Agreement, the Arrangement Agreement(or any similar documentation of the business relationship of theParties), or upon request of Covered Entity, whichever occurs first,if feasible, Business Associate will return or destroy all ProtectedHealth Information received from or created or received by BusinessAssociate on behalf of Covered Entity that Business Associate stillmaintains in any form and retain no copies of such information, orif such return or destruction is not feasible, Business Associate willextend the protections of this Agreement to the information andlimit further uses and disclosures to those purposes that make thereturn or destruction of the information not feasible; andiii. to ensure that its agents, including a subcontractor, to whom itprovides Protected Health Information received from or created byBusiness Associate on behalf of Covered Entity, agrees to the samerestrictions and conditions that apply to Business Associate withrespect to such information, and agrees to implement reasonableand appropriate safeguards to protect any of such informationwhich is Electronic Protected Health Information. In addition,Business Associate agrees to take reasonable steps to ensure that itsemployees’ actions or omissions do not cause Business Associate tobreach the terms of this Agreement.b. Notwithstanding the prohibitions set forth in this Agreement, BusinessAssociate may use and disclose Protected Health Information asfollows:i. if necessary, for the proper management and administration ofAppendix G
Business Associate or to carry out the legal responsibilities of BusinessAssociate, provided that as to any such disclosure, the followingrequirements are met:A. the disclosure is required by law; orB. Business Associate obtains reasonable assurances from the person towhom the information is disclosed that it will be held confidentiallyand used or further disclosed only as required by law or for thepurpose for which it was disclosed to the person, and the personnotifies Business Associate of any instances of which it is aware inwhich the confidentiality of the information has been breached; fordata aggregation services, if to be provided by Business Associatefor the health care operations of Covered Entity pursuant toany agreements between the Parties evidencing their businessrelationship. For purposes of this Agreement, data aggregationservices mean the combining of Protected Health Information byBusiness Associate with the protected health information received byBusiness Associate in its capacity as a business associate of anothercovered entity, to permit data analyses that relate to the health careoperations of the respective covered entities.C. Business Associate will implement appropriate safeguards toprevent use or disclosure of Protected Health Information otherthan as permitted in this Agreement. Business Associate willimplement administrative, physical, and technical safeguards thatreasonably and appropriately protect the confidentiality, integrity,and availability of any Electronic Protected Health Information that itcreates, receives, maintains, or transmits on behalf of Covered Entityas required by the HIPAA Security and Privacy Rule.c. Business Associate shall report to Covered Entity any use or disclosureof Protected Health Information which is not in compliance with theterms of this Agreement of which it becomes aware. Business Associateshall report to Covered Entity any Security Incident of which it becomesaware. For purposes of this Agreement, “security Incident” meansthe attempted or successful unauthorized access, use, disclosure,modification, or destruction of information or interference with systemoperations in an information system. In addition, Business Associateagrees to mitigate, to the extent practicable, any harmful effect that isknown to Business Associate of a use or disclosure of Protected HealthAppendix G
Information by Business Associate in violation of the requirements ofthis Agreement.d. Business Associate agrees to make available all records, books,agreements, policies and procedures related to the use and /o rdisclosure of protected health information to the Secretary of HHS forpurposes of determining Covered Entity’s compliance with the PrivacyRule.e. Covered Entity agrees:i. to obtain any patient consent or authorization that may be requiredby the Privacy rule
including chronic care coordination and patient-centered care. People with chronic conditions often require care and support between physician visits. Gaps in care may occur when that support is lacking due to factors such as a person's high-risk situation (i.e., uncontrolled blood glucose levels), follow-up challenges, or even lack of .