Transcription
Improvingcare for peoplewith MS: the potentialof data and technologySophie Castle-Clarke, Natasha Curry,Holly Dorning and Laura WetherlyJuly 2018
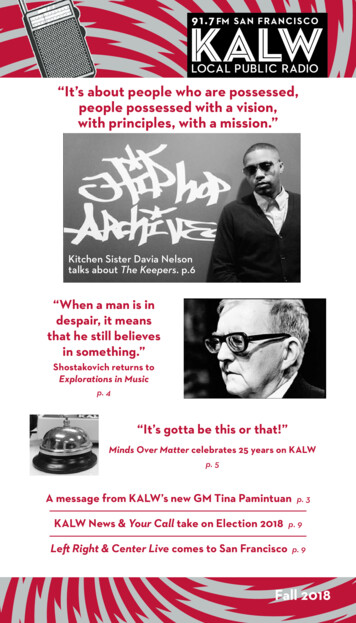
for people affected by MSThe potential of data and technologyfor people affected by MSData shared betweenservices means peopledon’t have to rememberand repeat themselvesIt’s easier for peopleto compare optionsand learn from eachother onlineDigital care planningand coordination helpsprofessionals andpatients to act asone teamInteractive digitalinformation makes iteasy to find what peopleneed and make decisionsNew digital toolsproduced with peopleaffected by MS so theywork for themAutomated collection andanalysis of outcomes meansricher data for cliniciansand researchersIncreased data collectionstrengthens knowledgeof what treatmentworks best fordifferent peopleMore controlover careAccessible andcoordinatedcarePeoplePeople with MS areconfident their data willbe used appropriatelywhen they share itwith MSThe righttreatment atthe right timeServicesthat bettermeet needHealth services use existingdata to understand whatpeople with MS need andprovide the right supportAudits help withcomparing servicesand drive improvementthrough shared learningTreatment outcomesreflect what mattersto people with MSand help them makethe right decisionsfor themPlanning isimproved throughnew data focussedon what mattersto people with MS
ContentsAcknowledgements4Stakeholders consulted throughout research4Glossary6Foreword – Michelle Mitchell, Chief Executive, MS Society8Executive summary11Chapter One: Helping people with MS take control of their care22The internet24The impact of apps on helping people manage their MS26Online patient networks30Chapter Two: Accessible and coordinated care34Coordinating care between professionals34Online access to records39Digital Care Plans40Making care more accessible through digital tools41Email and messaging41Remote consultations and telerehabilitation42Chapter Three: Improving access to the right treatments at the right time44Evaluating treatment outcomes44Improving data collection and professional trust45Chapter Four: Using data to better meet patient needs48Keeping people with MS out of hospital49Reducing treatment waiting times52Monitoring the progression of MS52MS Society view: the difference our recommendations could make54A common experience now54A possible experience in the future55How do we get there?56Annex 1: Summary of evidence for professionally-led services that use digital tools58Annex 2: Factors influencing attitudes towards data sharing61Appendix 1: Routinely collected data for improving MS service planning and commissioning63
AcknowledgementsWe are very grateful to everyone who participated in this research eitherthrough interviews, focus groups or roundtables (see stakeholder list below,published with consent). We are also very grateful to David Rog, ConsultantNeurologist and Divisional Chief Clinical Information Officer at Salford RoyalFoundation Trust as well as Nuffield Trust Colleagues Candace Imison andHelen Buckingham who reviewed the report and offered insightful feedback.Finally we are very grateful to the people with MS who shared their views aboutsharing their health data and using technology to manage their condition.Stakeholders consulted throughout researchAdnan AzfarSenior Implementation and BusinessManager, NHS DigitalTechnology roundtableparticipantAlison BradfordMS Specialist Nurse, Salford RoyalFoundation TrustData roundtableparticipantAnthony LawtonManaging Director, Front Foot MI Ltd. AndNHS RightCare AssociateData roundtableparticipantAshley AkbariSenior Research Officer, Farr Institute,Swansea UniversityData intervieweeChrissie WattersNational Clinical Audit Co-ordinator,National Services Scotland NHSData intervieweeDr David PalingConsultant in Neurology, RoyalHallamshire Hospital, Sheffield; HonorarySenior Lecturer, University of Sheffield;Clinical lead for Multiple Sclerosis, SouthYorkshireTechnology roundtableparticipantImproving care for people with MS4
Dr Martin DuddyConsultant Neurologist, Newcastle uponTyne Hospitals TrustData intervieweeMichael JacksonHead of Health Intelligence (Dementia& Neurology), Public Health England Mental Health, Dementia & NeurologyIntelligence NetworksData intervieweeMultiple intervieweesNI Health and Social Care BoardData intervieweesNeil WhiteChief Strategy Officer, MedopadPeter NuckleyService Delivery Manager for NHSWidening Digital ParticipationProgramme, Good Things FoundationTechnology roundtableparticipantRaman BehlHealth Informatics Lead, Practice andDevelopment, Chartered Society ofPhysiotherapyTechnology roundtableparticipantRod MiddletonProject Manager/System Architect, MSRegister operated by Swansea UniversityMedical SchoolData intervieweeand data roundtableparticipantSam BillingtonHead of Digital, Shift MSTechnology roundtableparticipantSamantha ColhounClinical Nurse Specialist – MultipleSclerosis, University Hospital Birminghamand Co-Chair, UKMSSNATechnology roundtableparticipantSelena BealingNational Lead for Prior ApprovalImplementation, NHS EnglandData roundtableparticipantSue ThomasChief Executive, Commissioning ExcellenceWilmington HealthcareData intervieweeand data roundtableparticipantTechnology roundtableparticipantImproving care for people with MS5
GlossaryAPIApplication Programming Interface: a method ofinteraction between softwareAnonymised dataAny way of identifying individuals is completelydestroyed.BlueteqThe company responsible for monitoring the use ofdisease modifying therapies in England, contracted byNHS England.Burden of treatmentHow equipped people feel to carry out tasks that helpthem stay well.Clinical CommissioningGroups (CCGs)Local organisations that are run by groups of GPs tobuy healthcare services for the local population.CommissioningThe process of deciding what services should beprovided in the NHS.Commissioning SupportUnits (CSUs)NHS organisations that provide a range of supportservices to CCGs.ConsentThe process of explicitly asking you whether you wouldlike your data to be shared for a certain purpose. Thissometimes happens with health data, but not always.Data securityEnsuring data is protected from corruption and accessby unauthorized individuals/software.Disease modifyingtherapies (DMTs)Treatments to slow the progression of MS.Expanded DisabilityScale Status (EDSS)A measure of disability and how it changes over time inpeople with MS.Improving care for people with MS6
Health care dataE.g. information on the number of people with MS,the types of services they’re accessing, the treatmentthey’re receiving and their outcomes.Health literacyA person’s capacity to find, process and understandhealth information and make appropriate decisionsregarding their health care.Information Governance(IG)The legal framework governing the use of personalconfidential data.Interoperabilitydifferent systems (for example IT systems) being ableto operate togetherMultiple sclerosis (MS)A progressive, neurological condition with manysymptoms including fatigue, mobility issues,depression and anxiety, cognitive problems and visualdisturbances.Patient activationA person’s level of knowledge, skill and confidence tomeaningfully participate in their health and care.Pharmacovigilancemonitoring the effects of medical drugs, especially toidentify adverse side-effectsPseudonymised dataIdentifying information (e.g. name, address) is replacedwith pseudonyms, e.g. a unique number. It is fairlystandard practice when using health data for reasonsother than providing care.Secondary uses of dataAny use of health data beyond delivering direct careto a patient (primarily service improvement, serviceplanning/commissioning and research).Improving care for people with MS7
Foreword – Michelle Mitchell,Chief Executive, MS SocietyIntroductionand technologycontextJust like all of us, the100,000 people withMS in the UK have hadaspects of their livesdramatically changedby technology. Fromhow we shop and run our homes to how we interactwith each other and access information, technologyand data have increasingly empowered us andpersonalised the services we use.1However, it’s fair to say there is one aspect of thelives of people with MS where the pace of changehas been much slower: their health and care.Websites like Amazon can offer personalisedrecommendations based on previous purchases,yet people with MS often find themselves havingto describe their case to new professionals fromscratch because their case history has not beenshared. Supermarket chains can track people’sjourneys through stores and use this metadata torearrange their products to match what people arelooking for, yet many parts of the NHS cannot sayhow many people with MS receive services in theirarea. The gap between policy ambition and real lifeexperience can be huge.With that said, we are starting to see long overduemoves to accelerate change. International examplesof innovative practice like the Cleveland Clinic2 haveshown promise – empowering patients with easy,online access to their health and appointmentsinformation – while in the UK NHS England’sTest Bed Programme3 has begun to act on theDepartment of Health’s ambition to use data andtechnology to deliver safer, more effective care by2020.4We welcome these initiatives precisely becausethe UK is so well placed to become a global leaderin delivering better health outcomes and qualityservices through the use of technology. TheUK Government’s Industrial5 and Life SciencesStrategies6 provide the building blocks to achievethis both across the wider economy and in healthcare specifically – setting out commitments toinvest in innovation and technological possibilitiesand to use the power of the NHS to support moreresearch and real-world data.About MS and the current state ofMS services and dataJust as in other areas of their lives, people with MSrightfully want health care to increasingly respondto how they live their lives, empowering them tomanage their condition and providing timely accessto the right services as they are needed.Sadly, so far for people with MS the reality is fallingfar short of this aspiration. Despite clear, acuteneed too often people with MS are still facingunwarranted variations in care and increasinglyrestricted access to over-burdened services. In2016 we found that 10% of people with MS hadneeded to see a neurologist but had not been ableto7 and 82% had not been offered a care plan inthe last 12 months.8 The UK has some of the lowestprescribing rates in Europe: we found 44% of thosewho could benefit from a disease modifying therapy(DMT) were not taking any.9Improving care for people with MS8
Our reportIn this context, it is perhaps tempting to dismissinnovation as a “nice to have” that MS servicescannot afford to focus on in the current climate. Infact the opposite is true: what services truly cannotafford is to stand still. That’s why we commissionedthe Nuffield Trust to take an in-depth look at thebenefits to be gained from harnessing the potentialof data and technology within MS health and careand moving towards the more technology-savvy,precision medicine and personalised model of carethat people with MS expect.For the first time, this report articulates a vision ofpersonalised, coordinated and empowering care forpeople with MS, enabled by effective technology,underpinned by robust data. We identify thepotential “win-wins” for people with MS and for thehealth and care system across four key areas.1.Helping people with MS to take morecontrol of their careWe want people with MS to able to selfmanage (defined by NHS England as actionsto recognise, treat or manage one’s health)10their condition but so far few MS specific toolsexist to support this, limiting engagement andeffectiveness. Improved understanding of theneeds of people with MS among technologydevelopers and support from the NHS todevelop targeted interventions could put selfmanagement within the reach of many peoplewith MS. Similarly, improved support for peoplewith MS to navigate their options and comparenotes with each other could make it easier forthem to find the solution that’s right for them.2. Accessible and coordinated careTechnology-enabled services would allowcoordination between the many professionalspeople with MS see, drastically improving thecurrently complicated and confusing systemof care and appointments which often meanpeople with MS have to repeat their storiestime and again. Better still, it would giveprofessionals an easy way to refer to each other,maximising the chances that people with MS willreceive all of the treatments and services thatcould help them. Too often where people withMS should receive things like home adaptationsthe message never gets through to the teamresponsible for providing these11. Harnessingdata and technology to analyse medical dataand history – and share it more easily – wouldallow professionals to truly act as a team,always involving each other where needed andresponsively reacting to issues as they occur.3. Improving access to the right treatmentsat the right timeBoth data and technological innovationcould play a part in deepening our often poorunderstanding of prescribing practice, targetingunwarranted variation and helping to improveaccess to the right treatments at the right timewhich can slow the progression of MS. Linkingcurrently collected prescribing data (such asthe Bluteq form in England) to the MS Registerwould be a stepping stone to robust andevidenced prescribing practice.Improving care for people with MS9
4. Using data to better meet patient needsCurrent MS data collection is patchy and rarelyused to best effect. With action, comprehensiveand robust MS data could be collected andshared, allowing services to be planned andcommissioned on a complete picture of theneeds of the MS population. Services wouldbe responsive and tailored to local need –drastically improving the experiences of peoplewith MS.Achievi
Clinical lead for Multiple Sclerosis, South Yorkshire. Impr or 5 Consultant Neurologist, Newcastle upon Tyne Hospitals Trust Head of Health Intelligence (Dementia & Neurology), Public Health England - Mental Health, Dementia & Neurology Intelligence Networks NI Health and Social Care Board Chief Strategy Officer, Medopad Service Delivery Manager for NHS Widening Digital Participation