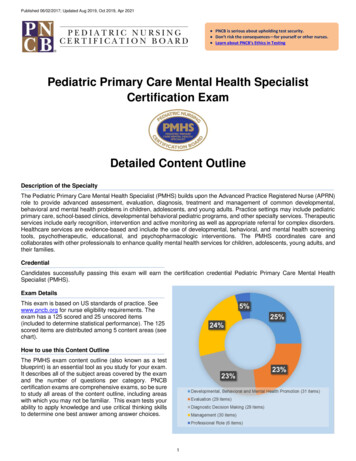
Transcription
A FAMILY GUIDEIntegrating Mental Health andPediatric Primary Care
Find Help. Find Hope.A Family Guide: Integrating Mental Health and Pediatric Primary Care 2011 by NAMI, the National Alliance on Mental IllnessNAMI, the National Alliance on Mental Illness, is the nation’s largestgrassroots mental health organization dedicated to building better lives forthe millions of Americans affected by mental illness. NAMI advocates foraccess to services, treatment, supports and research and is steadfast in itscommitment to raising awareness and building a community of hope forall of those in need.To access this publication, visit www.nami.org/primarycare.Stock photos used in this publication are not meant to indicate any particular attitude or opinion onthe part of those whose images are being used and are not intended to indicate an endorsement bythe subjects.
A FAMILY GUIDEIntegrating Mental Health andPediatric Primary CarePrepared by:Darcy Gruttadaro, J.D., director, NAMI Child and Adolescent Action CenterDana Markey, program manager, NAMI Child and Adolescent Action CenterNovember 20111st Edition
TABLE OF CONTENTSAcknowledgments.3Introduction.5Integrated Care: What Is It?.7At a Glance: Steps to Integrated Care. 9Why Integrated Care Makes Sense for Families. 13How Integrated Care Can Benefit Your Family. 15The Medical Home and Integrated Care . 16How Families Can Become More Involved in the .Integrated Care Movement. 18Learn More: Ask Questions About Integrated Care. 19Speak Up: Communicate Your Needs.22Share Resources: Help Your Primary Care Office. 23Raise Your Voice: Gather Families to Get Involved. 23Build Support: Reach Out to Stakeholders in Your .Community. 23Bring Change: Weigh In On the Integrated Care Movement. 24Overcome Challenges: Use Your Network to Find .Creative Solutions. 25Making the Case for Integrated Care. 26Integrated Care in the Real World: Model Programs. 27Massachusetts Child Psychiatry Access Project. 28North Carolina Center of Excellence for Integrated Care. 30Cherokee Health Systems. 31Conclusion. 33Resources for Families. 33Glossary of Terms.34References. 352A Family Guide
ACKNOWLEDGMENTSThis family guide was developed by the National Alliance on MentalIllness (NAMI) with partial support from the Child, Adolescent andFamily Branch, Center for Mental Health Services (CMHS), SubstanceAbuse and Mental Health Services Administration (SAMHSA). Theinformation, opinion and commentary in this guide are those of NAMIand do not necessarily reflect those of CMHS, SAMHSA or theDepartment of Health and Human Services. We greatly appreciate theirassistance and support for making this family guide possible.This guide would not have been possible without the dedication andhelp of the following individuals who participated in our expert workgroup on integrating mental health and primary care:Laura M. GalbreathSAMHSA-HRSA Center forIntegrated Health SolutionsNational Council for CommunityBehavioral HealthcareRuth Hughes, Ph.D.CEOChildren and Adults withAttention Deficit/HyperactivityDisorderStephanie Nelson, M.S.ManagerMental Health IntegrationActivitiesAmerican Academy of PediatricsSarah StevermanDirector of State PolicyMental Health AmericaLinda B. Paul, M.P.H.ManagerCommittees and Sections TaskForce on Mental HealthAmerican Academy of PediatricsKristin Kroeger PtakowskiSenior Deputy Executive DirectorAmerican Academy of Child andAdolescent PsychiatryIntegrating Mental Health and Pediatric Primary Care3
We would also like to express our gratitude to the followingindividuals for the information, expertise and resources they provided forthis manual:Susan Van Cleve, D.N.P.President ElectNational Association of PediatricNurse PractitionersFrank Verloin deGruy III, M.D.Woodward-Chisholm Professor andChairDepartment of Family MedicineUniversity of Colorado School ofMedicineRegina Schaaf Dickens, Ed.D.Program DirectorNorth Carolina Center forExcellence for Integrated CareParinda Khatri, Ph.D.Director of Integrated CareCherokee Health SystemsBenjamin F. Miller, Psy.D.Assistant ProfessorDepartment of Family MedicineUniversity of Colorado School ofMedicineBarry Sarvet, M.D.Associate Clinical ProfessorTufts School of MedicineCo-medical DirectorMassachusetts Child PsychiatryAccess ProjectDolores Jones, Ed.D.National Association of PediatricNurse PractitionersWe wish to thank our family reviewers for their insightful feedback ondraft versions of this guide, including Sue Abderholden, AliciaStevenson and Sherri Wittwer. We are especially grateful to MichaelCohen, another family reviewer, for sharing his wisdom and experiencegained from working with families in New Hampshire. This guide wasstrengthened by his involvement. We also wish to thank the AmericanAcademy of Pediatrics reviewers Marian Earls, M.D., Jane Meschan Foy,M.D., and Angela Tobin.Lastly, we greatly appreciate the input and guidance from KennethDuckworth, M.D., NAMI’s medical director, and NAMI staff for theirvaluable contributions, including Katrina Gay, Brendan McLean, CourtneyReyers and Marin Swesey. We especially appreciate the contribution ofBianca Ruffin for her design work.4A Family Guide
INTRODUCTION“Integration is in response to the fragmentation ofhealth care. As individuals we are not fragmented,we are whole people. The current health care systemdoes not recognize this. Integration is trying to fixa big problem, which is that we have two separatesystems that take care of our health. Integration is agame changer for health care.”– Benjamin Miller, Psy.D., assistant professor, Department ofFamily Medicine, University of Colorado School of MedicineWe know physical health impacts mental health and mental healthimpacts physical health. Yet, the health care system has historicallytreated mental and physical health separately. You may experience thiswhen you visit a primary care provider with your child and then are sentelsewhere for mental health care. This fragmentation is often costly,frustrating and does not lead to the best outcomes for families.When it comes to the health and well-being of your child, it is importantto understand that mental health is part of overall health. A healthy childis one with a healthy body and a healthy mind. You cannot have onewithout the other.Addressing the whole person by integrating care is one way to begin toaddress the fragmentation that often exists in our health care system.Integrated care is designed to treat mental health conditions like anyother health conditions that children experience.There is widespread support to improve our nation’s health care systemby effectively integrating mental health and pediatric primary care. “The need for primary care clinicians to manage children with mentalhealth concerns only will continue to increase in the future Primary care clinicians are, and will continue to be, an importantfirst resource for parents who are worried about their child’sbehavioral problems.” – American Academy of Pediatrics Task Forceon Mental Health1 “One of the best indicators of risk for emergence of mental illness inthe future is the presence of parental or caretaker concern about aparticular child’s behavior. Primary care offices can screen for risk byroutinely inquiring about parental concern. The prevention of mentalIntegrating Mental Health and Pediatric Primary Care5
illness and physical disorders and the promotion of mental healthand physical health are inseparable.” – National Research Counciland Institute of Medicine2 “Mass screening in primary care could help clinicians identify missedcases and increase the proportion of depressed children andadolescents who initiate appropriate treatment. It could also helpclinicians to identify cases earlier in the course of disease.” – U.S.Preventive Services Task Force3 “This report calls on the nation—its leaders, its mental healthresearch and service provision agencies, its schools, its primary caremedical systems, its community-based organizations, its child welfareand criminal justice systems—to make prevention of mental,emotional and behavioral disorders and the promotion of mentalhealth of young people a very high priority.” – National ResearchCouncil and Institute of Medicine4Interest in mental health and primary care integration is growing. Manycommunities have developed innovative approaches to improve thequality of care provided to youth and families. These communities haveseen the benefits of addressing mental and physical health conditions in acoordinated, collaborative manner to ensure that children receivecomprehensive and high quality care and reach their optimal health.Integrated care presents you and your child with opportunities to activelyparticipate with both primary care and mental health providers in caredelivery. It is important to understand what integrated care means, what itlooks like in practice and how it impacts you and your child.So, what exactly is integrated care and what does it mean for your child?How might this change your role in seeking mental health care for yourchild? What questions should you be asking in an integrated care settingand what should you expect?This guide is designed for families to provide you with a roadmap tonavigate the integrated care landscape. It offers families help and hope infinding the best comprehensive care for their child. This guide will helpyou better understand what integrated care is and what it can mean foryour child’s improved health. Reading this guide may help you thinkdifferently about the kind of help you may want to seek for your child6A Family Guide
and questions to ask your primary care provider. Asking the rightquestions can get you and your child more effective care. This guide alsoprovides you with information on how to become more involved in theintegrated care movement to improve the quality of care that your childreceives.While integration of mental and physical health care applies across thelife span, this guide highlights the impact of integration on children andyouth and what you need to know about mental health care in thepediatric primary care setting.INTEGRATED CARE: WHAT IS IT?There is no one definition or approach to integrated care. Rather thereare principles and concepts that help to define what it means. Here aretwo definitions that capture the principles and concepts of integratedcare: “Integrated health care is the systematic coordination of physical andbehavioral health care. The idea is that physical and behavioral healthproblems occur at the same time. Integrating services to treat both willyield the best results and be the most acceptable and effectiveapproach for those being served.” – The Hogg Foundation for MentalHealth5 “Integrated primary care combines medical and behavioral healthservices to more fully address the spectrum of problems that patientsbring to their primary medical care providers. It allows patients to feelthat, for almost any problem, they have come to the right place.”– Alexander Blount, Ed.D., director, Center for Integrated PrimaryCare6Integrating Mental Health and Pediatric Primary Care7
Simply put, integrated care refers to the practice of incorporating mentalhealth care into primary care settings and primary care into mental healthcare settings for the purpose of improving the quality of care.There is no single, right way to integrate services and supports. There area number of steps that primary care practices can take in moving towardintegrated care. These steps include everything from distributinginformation to families about mental health care in primary care practicesto co-locating mental health care in primary care practices to fullyintegrated collaborative care. These steps aim to improvecommunication, collaboration and coordination among health careproviders, families and youth and emphasize a care team approach toaddressing mental and physical health concerns. The table, At a Glance:Steps to Integrated Care, captures the different ways in which primary carepractices can move toward fully integrated care.For most youth, the pediatric primary care setting is the most practicallocation for integrated care because most families and youth access carein primary care offices. The primary care office is a place where familieshave often established a trusting relationship with a primary careprovider. It is also a place that youth are familiar with and arecomfortable visiting. However, youth with serious mental healthconditions who require ongoing, regular care from mental healthproviders may benefit from coordinated care in a mental health caresetting that also has the capacity to provide essential primary care.8A Family Guide
Integrating Mental Health and Pediatric Primary Care9Primary care and mental health careproviders are educated and trained toaddress both mental health and otherphysical health concerns.Primary care office displays posters,brochures and fact sheets that emphasizethe importance of mental health and shareinformation with youth and families.Share mental healthinformation,supports andresources withyouth and families.Provider educationand training.DescriptionStepsPromotes understanding acrosshealth care fields. Creates a welcoming environment for conversations aboutchildren’s mental health. Increases providers’ knowledge,expertise and capacity.Helps to normalize mentalhealth issues. Connects families to valuableinformation. Helps providers confidentlyaddress both mental and physical health issues.Makes a statement that mentalhealth matters. Raises public awareness aboutmental health.Benefits AT A GLANCE: STEPS TO INTEGRATED CARE Training and education can becostly.Training provides time-limitedimpact without other supports.Follow-up and ongoing coachingand mentoring are needed butrarely provided.Primary care practices may havelimited capacity to help ensurethat families understand theinformation being shared.It does not lead to care for achild in need.Resource distribution is a smallstep.Limitations
10A Family GuideMental healthscreening.Identifying billing codes to seekreimbursement for mental health care.Reviewing technology needs related toelectronic health records. Primary care providers use checklists orquestionnaires to ask children, youth andfamilies about their feelings, behaviors andfunctioning in order to identify mental healthconcerns early.Adjusting primary care provider schedules to allow for longer appointments.Primary care office develops a plan to beginto provide mental health care. This caninclude: Identifying staff who will provide youthand families with behavior rating scalesand collect information from schoolsand other child-serving agencies tobetter understand the child’s needs.Planning forchanges in theprimary careoffice to delivermental health care. DescriptionStepsIdentifies mental healthconcerns early and alerts thecare team about concerns.Links youth to services andsupports before mental healthconcerns become more serious. Organized office systems support primary care providers inproviding comprehensive andcoordinated care. BenefitsAT A GLANCE: STEPS TO INTEGRATED CARE (continued) Children and youth may notbe comfortable with screeningif they have concerns aboutconfidentiality.Screening without follow-up anda link to effective services doesnot improve outcomes.The dissemination, collectionand review of screening toolsand outside records is oftentime-consuming. Primary care offices are busyand longer visits with childrenand families may be challengingfor practices. Limitations
DescriptionSupportivecounseling andtreatment withconsultation.Primary care providers provide supportive counseling, family education andtreatment within the primary care setting formild to moderate issues rather than referringfamilies out. Mental health providers are available in-person, by phone or by videoconference to provide consultation on cases.Primary care referral Primary care office provides referrals to with collaboration. families for mental health providers that takeinto account the family’s treatment preferences and barriers to accessingmental health care. This enhanced referralsystem also encourages follow-up, feedbackand coordination between the primary careproviders and mental health care providers. Steps Allows the primary care providerto draw upon the expertise of atrained mental health providerand to become more comfortable in addressing the needsof children with mental healthconditions. Improves the primary careprovider’s ability to effectivelytreat a child with mental healthneeds.Allows primary care providers toremain involved and toeffectively coordinate care.Facilitates communication,collaboration and treatmentcoordination between primarycare and mental healthproviders.Encourages follow-through withreferrals.BenefitsAT A GLANCE: STEPS TO INTEGRATED CARE (continued)They may be uncomfortable orunwilling to provide any levelof mental health care in theirprimary care offices.Primary care providers may notbe able to provide long-termpsychotherapy or evidencebased treatments.A national shortage of child andadolescent mental healthproviders has led to limitedreferral options and long waitingtimes for families seekingmental health care for theirchild.LimitationsIntegrating Mental Health and Pediatric Primary Care11
12A Family GuidePrimary care providers and mental healthcare providers are housed in the samesetting.DescriptionCollaborative careA comprehensive, team-based approachor coordinated team to integrated care in which mental healthcare.providers are on staff and work with primarycare providers as a care team on an ongoingbasis to address the mental and physicalhealth needs of youth. This approach oftenentails regular care team meetings, training,close collaboration on treatment plans andshared electronic health records.Co-location ofservices.StepsAllows families and youth toaccess a full array of integratedmental and physical healthservices and supports in anintegrated setting.Improves family satisfactionwith services and treatmentoutcomes. Makes it easier for families tofollow-through with referrals. Increases the opportunity forprimary care providers andmental health providers tocommunicate, collaborate andcoordinate care. BenefitsAT A GLANCE: STEPS TO INTEGRATED CARE (continued)There may be sustainabilityissues because it can be difficultto secure funding to cover thecost of time spent oncollaboration and consultationwith the care team.May encourage a hand-offwithout coordinated care. Does not guaranteecollaborative, coordinated orintegrated care. Limitations
WHY INTEGRATED CARE MAKES SENSEFOR FAMILIES“When families are so caught up in trying to takecare of their child’s mental health needs, regularhealth care needs—such as vision, weight, bloodpressure, allergies—fall to the wayside. When care isintegrated, parents only have to go through onedoor, not multiple doors, to make sure their child ishealthy.”– Sue Abderholden, parent and executivedirector, NAMI MinnesotaThe integration of mental health and primary health care makes sense forseveral reasons. Most families value their relationship with their primarycare providers and are comfortable openly discussing concerns abouttheir child. Primary care providers are often the first point of contactwhen a child is born. Primary care providers, typically pediatricians, arealso the trusted professionals that families most often turn to withconcerns about the health and well-being of their child. This placesprimary care providers in a key position to improve the early identification of mental health concerns and to link families with effective servicesand supports.Most families initially seek help for mental health concerns in theprimary care setting. This is especially true for families from culturally,economically, racially and ethnically diverse communities.7 Up to 70percent of primary care medical appointments are for issues related topsychosocial concerns.8 More than half of all care for common mentalhealth conditions—including anxiety, depression, attention-deficit/hyperactivity disorder (ADHD) and related conditions—is provided in theprimary care setting.9Integrating Mental Health and Pediatric Primary Care13
There are several reasons to seek help from the primary care setting: Easier access to care because of a critical shortage of mental healthproviders, especially in rural communities. Care provided in a primary care setting may be covered by insurancepolicies that do not include mental health care coverage. Families may feel more comfortable in a primary care setting becauseof stigma associated with seeking care in a mental health care setting.Many families have long-standing, trusting relationships with primarycare providers and these providers understand how to work effectivelywith youth and families. You and your child may want to ask yourprimary care provider to use his or her experience in coordinating carewith specialists on a broad range of health issues to help ensure that yourchild gets the help that he or she needs from mental health providers.14A Family Guide
HOW INTEGRATED CARE CAN BENEFITYOUR FAMILY“When my family physician spoke with mydaughter’s therapist everyone finally was on thesame page. I felt like my daughter’s treatmentmoved forward and all of her health needs werebeing addressed Finally, everyone—my daughter,my family and I—had hope that treatment was onthe right track and things would be better.”– ParentIntegrated care is re-envisioning the way your child receives andparticipates in health care. There are many ways in which you can benefitfrom integrated care.Families, health care providers and program leaderswho have experience with integrated care havereported the following benefits for families:10, 11Improved access to care.Reduced stigma.Avoidance of treatment .errors and duplicative testsand lab work that are costly.Reduced treatment errors by.using an integrated medicalchart.Increased consultation,referral and collaborationbecause of regular contactbetween mental health andprimary care providers.Encouraged the development of individualized careplans and established clearlines of responsibility for .follow up.Improved adherence to .treatment.Greater convenience and .satisfaction for families.Increased likelihood that .families follow through withreferral for mental health .services and supports.Decreased wait times .between mental health .referrals and initial .appointments.Decreased use of unneededmedical and emergency .services.Increased attention to the .treatment preferences of .families.Integrating Mental Health and Pediatric Primary Care15
Ultimately, integrated care promises to improve the quality of careprovided to children, youth and families. It helps to establish ongoing,close relationships between youth, families and health care providers thathelp to produce better outcomes and greater satisfaction with care foreveryone.THE MEDICAL HOME AND INTEGRATED CARE“The medical home is built on a trusting,collaborative, working partnership betweenthe child, family and primary care provider incooperation with specialty care practitionersand the community network of medical andnon-medical resources.”- Marie Mann, M.D., medical officer, Maternal and Child HealthBureau, Health Resources and Services AdministrationA “medical home” is an approach to delivering comprehensive andcoordinated primary health care. The medical home approach provides a“go to” care team to help families and youth access needed resources andto coordinate care across all practice settings. There is no singledefinition for a “medical home,” but there are key elements that help todefine this approach to care. The American Academy of Pediatrics (AAP),which has helped to define the concept of “medical home,” has statedthat the medical home approach to care includes: Accessible care 24 hours a day and seven days a week for clinicalsupport, questions and concerns. Continuous care to allow youth and families to see a member of thecare team who is familiar with their unique needs. Child and family-centered care to ensure youth and familiesdevelop an effective partnership with the treating provider and careteam who respects them as experts, encourages their participation incare delivery and ensures that care is always provided based onfamily needs and preferences. Coordinated care between youth and families, primary care and anyspecialty care when needed by developing effective care plans, securingreferrals to specialty care, maintaining health records and providingyouth and families with connections to other community resources.16A Family Guide
Comprehensive care by ensuring that the child receives appropriatescreenings, necessary evaluations, preventive care, specialty care andeffective management of all health conditions to help the child reachhis or her full potential. Compassionate care by providing the youth and family with asupportive, safe and comfortable place to share concerns and askquestions. Culturally effective care by acknowledging and addressing thecultural and religious beliefs and values of the youth and family inservice delivery and outcome goals. Health care providers should beaware of the cultures in their communities and should respect thevalues and beliefs of those cultures in all aspects of care.The medical home should include the capacity to address mental andphysical health concerns together. Youth, families and primary careproviders should work as a team to determine the resources that areneeded for the child to be mentally and physically well and to reach hisor her full potential.The medical home emphasizes the importance of treating the wholechild from the top of the head to the tip of the toes. The medical homeprovides a framework for thinking about and implementing integratedcare because it focuses on team work, collaboration, developing effectivepartnerships with youth and families, coordinating care and improvingthe overall quality of care.The Patient Protection and Affordable Care Act, the federal health carereform law, includes a new Medicaid Health Home option. This optionexpands on the traditional medical home model and provides Medicaidfunding for comprehensive care management, care coordination andcollaboration, individual and family support and more for children,youth and adults with serious mental health conditions.12 This stateMedicaid option is designed to improve the quality of care that isdelivered to children and adults with a number of chronic healthconditions, including serious mental health conditions, and promises toincrease the state-level focus on integrated care.Integrating Mental Health and Pediatric Primary Care17
HOW FAMILIES CAN BECOME MORE INVOLVEDIN THE INTEGRATED CARE MOVEMENT“Primary care providers need families and youthto help them lead this effort in making integrationprograms available for all.”– Brenda Reiss-Brennan, M.S., mental health integrationdirector, Intermountain HealthcareThe integrated care movement is still in its infancy, so there are manyopportunities for youth, families and family organizations to becomemore involved in helping to shape the development of integrated careapproaches. Much of the work that has been done to date has beeninitiated by providers, with little involvement of the family voice. Iffamilies are involved, it is more likely that the integrated care models thatare developed will work better for you and your child.There are many ways to get involved. You can learn more about how careis delivered in your child’s primary care practice, talk about your needs inan integrated care setting with your primary care provider and determinehow you can help to bring more integrated care into the practice. Youcan also work with other youth, families and organizations to reach outto other stakeholders involved with integrated care to help design andpromote effective integrated care models in your state and community.These proactive steps are all summarized, starting on page 19.For starters, learn all that you can about integrated care. This guide is astart, but the more you understand about medical homes, co-locationmodels, collaborative care and related issues, the more you can weighin on the subject. Knowledge is power. A full array of family friendlyresources on integrated care is available at www.nami.org/primarycare.18A Family Guide
LEARN MOREASK QUESTIONS ABOUT INTEGRATED CARE Start a conversation with your child’s primary care
Steps to Integrated Care, captures the different ways in which primary care practices can move toward fully integrated care. For most youth, the pediatric primary care setting is the most practical location for integrated care because most families and youth access care in primary care offices. The primary care office is a place where families