Transcription
Network of Arizona2017 Provider guide
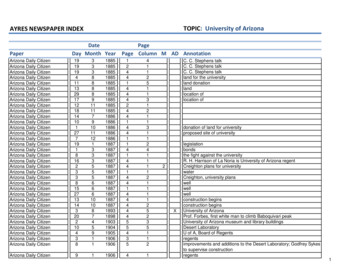
Contents1 Purpose24 Credentialing & recredentialing1 Business overview26 Health improvement4O ptumCare contact information27 Quality improvement7 Patient enrollment & assignment29 CMS quality measure overview7 Health plan contact information30 Medical records standards8 Health plan ID cards34 Appointment access criteria9O ptumCare website36 Preventive care recommendations10 OptumCare provider portal39 Utilization management &prior authorization12 OptumCare customer service13 Language & hearing impaired assistance13 Eligibility41 Prior authorization form43 Hospital admission notification14 Claims45 Coordination of benefits (COB)& third party liability (TPL)15 Electronic data interchange (EDI)46 Provider dispute resolution process16 Claim submission address47 Provider dispute resolution request17 Billing48 Care management overview18 Reading the provider remittance advice (PRA)52 Referral form for member programs18 Electronic fund transfer (EFT)54 Medicare risk adjustment19 Claims & encounter submissions54 CMS hierarchical conditioncategories (HCC) model20 Submission time frames21 Glossary of claims terminology23 Helpful billing & claims hints56 Annual wellness visits
PurposeThe purpose of this manual is to provide key information to our contracted networkproviders and support you in delivering effective care for mutual patients in accordancewith OptumCare Network of Arizona and industry standards.The vision of OptumCare is to meet individual patient’s needs through a connected set ofpractices and services. We look forward to working with you to achieve this visionand to providing you with the support you need to improve the health and well-beingof your patients.Business overviewWho is OptumCare?OptumCare Network of Arizona is an Independent Physician’s Association. We offer a fullrange of services to assist physicians and other providers in their managed care and businessoperations. The network is a health care innovator, with a track record for quality, financialstability and extraordinary services. We are well positioned to continually invest in newinfrastructure and systems for the benefit of our contracted physicians and to accommodatethe impending changes of health care reform.OptumCare contracted providers represent a network of over 1,000 primary care physicians(PCPs), 4,000 specialists and 17 hospitals serving all of Maricopa County.OptumCare is a fully delegated entity, assuming both institutional and professional financialrisk which allows us to enhance the coordinated care model. The network currently acceptsglobal capitation agreements with health plans for the provision of medical services for mostof its Medicare Advantage patients.1Provider guide
Service areaOptumCare serves the entire Maricopa County area.Provider guide2
MissionWe connect and support providers to deliverthe most effective and compassionate careto each and every patient.VisionTo improve lives by transforming health carein Phoenix: one patient, one family, onecommunity at a time.ValuesIntegrity. Compassion.Relationships. Innovation. Performance.3Provider guide
OptumCare contact informationNetwork contact informationOptumCare service center:1-877-370-2845 or visit us online: optumcare.com/arizona/provider-resourcesService Advocates are available to answer questions Monday through Saturday.Provider relations teamOptumCare assigns a provider relations representative to each practice, in order to give youpersonal service. They will get to know your business needs, make sure your practice understandsthe network’s best practices and assist with your questions and requests. Below is a full listing ofprovider network managers:Teresa Casillas1-623-707-2967Janice Chavarria1-623-707-0842Sharon L. Hawn1-623-707-2962Karen Jones1-623-707-0826Mark McLean1-623-707-0861Kathy MorenoGinny SandisonJamie TaylorCharmie UherMary WardElise 623-707-08531-623-707-08091-623-707-0859Prior authorization (urgent & routine): 1-877-370-2845Prior authorization fax: 1-888-992-2809Rx prior authorization for UnitedHealthcare patients:Phone: 1-800-711-4555Fax: 1-800-527-0531Online: optumrx.com health care professional prior authorizationsA prior authorization process is in place to provide for coverage of select formulary andnon-formulary medications. Depending on the patient’s plan, you can access the MedicareAdvantage Prescription Drug Formulary online and the drugs requiring prior authorizationat the plan’s website.Transplant prior authorization: 1-888-936-7246OptumCare community center: 1-623-707-0800For more information on classes and events at the OptumCare Community Center,visit our patient website: er guide4
Specialty, facility and ancillary contact informationLaboratory:Laboratory Corporation of America (LabCorp)Phone: 1-800-788-9743Online: labcorp.comLabCorp is the exclusive participating laboratory for OptumCare patients.In-home (mobile) laboratory:1st Choice Phlebotomy: 1-480-593-9192Mental health:Please refer to the back of the patient ID card for information on the mentalhealth provider network.Optum Behavioral Solutions: 1-800-579-5222or Crisis Preparation & Recovery, Inc.: 1-480-804-0326Durable medical equipment and infusion services:Preferred HomecarePhone: 1-480-446-9010Home health care (includes nursing, PT/ OT/ ST, social work, aide):Professional Health Care Network (PHCN)Phone: 1-602-395-5100Note: Referral forms for Home Health Services can befound on the OptumCare ysical, occupational, speech language therapy, and covered chiropractic services:Optum Physical HealthPhone: 1-800-873-4575Ophthalmology services:For locations and contact information, please refer to the online Referral Lookup tool atlookup.optumcare.com/arizona/find-doctors, or contact the Service Center.5Provider guide
Preferred specialty groups:In an ongoing effort to provide our patients with the highest level of service, OptumCare hasestablished preferred or exclusive arrangements with certain specialty groups. Preferred andexclusive specialists were chosen based on quality, performance metrics, geographic locationand availability of clinical services. Please direct all patient referrals within these specialties to thegroups listed below.Nephrology referrals:Arizona Kidney Disease andHypertension Centers (AKDHC)Phone: 1-602-997-0484Online: akdhc.comDesert KidneyPhone: 1-602-997-0484Fax: 1-480-964-7802Online: desertkidney.comRadiology & imaging services:Southwest Diagnostic Imaging (SDI)Phone: 1-602-955-4734Fax: 1-602-956-9729Online: sdil.netSimon MedPhone: 1-623-972-9669Fax: Varies on locationOnline: simonmed.comAztech ImagingPhone and fax vary by location. See website.Online: aztechradiology.comDesert Valley ImagingPhone and fax vary by location. See website.Online: dvrphx.com/locations.phpMarquis Diagnostic ImagingPhone: 1-480-553-8999Fax: Varies on locationOnline: marquisdiagnosticimaging.comAdditional specialists & facilities:For information on additional OptumCare specialists and facilities, please contact ourService Center:OptumCare service centerPhone: 1-877-370-2845 Online: Use the provider lookup r guide6
Patient enrollment & assignmentTo utilize services from OptumCare contracted physician and ancillary network, individualpatients or employer groups can purchase health care coverage from any of our contractedhealth plans and select a network contracted primary care physician (PCP). In the network,patients choose their PCP; the network does not assign patients to providers.Our Service Center is available to assist patients in selecting providers if they need help.Health plan contact informationOptumCare proudly accepts the following health plans:AARP MedicareComplete insured throughUnitedHealthcare Plan Name:AARP MedicareComplete Plan 1CMS Contract: H0609-026AARP MedicareComplete insured throughUnitedHealthcare Plan Name:Plan Name: AARP MedicareComplete Plan 2CMS Contract: H0609-027UnitedHealthcare GroupMedicare AdvantagePlan Name:UnitedHealthcare Group Medicare Advantage(HMO) CMS Contract: H0609-807, H0609-808,H0609-8097Provider guide
Y0066 150609 163758 AcceptedY0066 150609 163758 AcceptedPlan 1 exampleAttached is your Health Insurance MemberIdentification Card (ID Card). Verify theinformationon yourID Cardis correct.If youAttachedis yourHealthInsuranceMemberneed to makeCardchangesor havequestions,pleaseIdentification(ID Card).Verifythecall the Customernumberon theinformationon yourServiceID Cardphoneis correct.If youback ofCard. Alwaysyour IDpleaseCardneedto yourmakeIDchangesor havecarryquestions,withtheyou.Customer Service phone number on thecallback of your ID Card. Always carry your ID CardwithVisit you.the website listed on the back of yourID Card to access plan information.Visit the website listed on the back of yourIDCardareto insuredaccess nce Company or one of its affiliatedPlansare insuredthroughAdvantageUnitedHealthcarecompanies,a MedicareorganizationInsuranceCompanyor oneEnrollmentof its affiliatedwith a Medicarecontract.in the plancompanies,MedicareAdvantageorganizationdepends on atheplan's tintheplanMedicare.depends on the plan's contract renewal withMedicare.CUSTMAPDGPS DIV INDRUN DATEDATA SEQ NOCLIENT NUMBERUHG TYPEDOC SEQ IDDOC IDNAMEMAILSET NUMBERCUSTMAPDGPS KEY18563577 KEY0CUSTMAPDGPS KEY2CUSTMAPDGPS KEY3CUSTMAPDGPS KEY4CUSTMAPDGPS KEY5CUSTMAPDGPS KEY6CUSTMAPDGPS KEY7CUSTMAPDGPS KEY8CUSTMAPDGPS 563577 00CARD114:53:3025ExampleIDDcardRUN DATEDATA SEQ NOCLIENT NUMBERUHG TYPEDOC SEQ IDDOC IDNAMEMAILSET NUMBERCUSTMAPDGPS KEY18563577 KEY0CUSTMAPDGPS KEY2CUSTMAPDGPS KEY3CUSTMAPDGPS KEY4CUSTMAPDGPS KEY5CUSTMAPDGPS KEY6CUSTMAPDGPS KEY7CUSTMAPDGPS KEY8CUSTMAPDGPS KEY9CUSTMAPDGPS DIV 563577 00CARD114:53:3025-Visiton theback of althcareIDCardtoaccessplaninformation.Insurance Company or one of its affiliatedcompanies, a Medicare Advantage nitedHealthcarewith a areMedicarein the plaInsuranceCompanyoroneof itsrenewalaffiliateddepends on the plan's contractwithcompanies,Medicare. a Medicare Advantage organizatiowith a Medicare contract. Enrollment in the pladepends on the plan's contract renewal withMedicare.Attached is your Health Insurance MemberIdentification Card (ID Card). Verify theinformation on your ID Card is correct. If youAttachedis yourHealth orInsuranceMemberpleneed to makechangeshave questions,IdentificationCard(IDCard).Verifythe on thcall the Customer Service phone numberinformationonyourIDCardiscorrect.youCaback of your ID Card. Always carry yourIf IDneedto make changes or have questions, plewith you.call the Customer Service phone number on thbackof yourID Card.yourID CaVisit thewebsitelistedAlwayson the carryback ofyourwithyou.ID Card to access plan information.PO Box 29830Hot Springs, AR 71903-9830PO Box 29830Hot Springs, AR 71903-9830Benefits Start Date:01-01-2017Benefits Start Date:01-01-2017UnitedHealthcare PlanID cardCustomer ServiceHours:Service8 am - 8Hours:pm 7 days/weekCustomer8 am - 8 pm 7 days/weekPlan 2 example11HealthPlan (80840):911-87726-04Health Plan(80840):911-87726-04MemberID: 9999999-99 Group Number:Group Number:HCFAH4Member ID:9999999-99HCFAH4PLAN RL3CODE: RL3Member: Member:PLAN CODE:SUBSCRIBERSUBSCRIBERBROWNBROWNPayer2 ID:Payer ID:LIFE1 LIFE1PCP Name:PCP Name:SUBSCRIBERSUBSCRIBERBROWN BROWNPCP(999)Phone:(999) 999-9999PCP Phone:999-9999RxBin: RxBin:610097 6100973MEDNETWORKRxPCN:RxPCN:9999 9999MED NETWORK NAME NAMERxGrp:Copay:SHCO SHCOCopay: PCP 0 PCP 0 ER 75 ER 75RxGrp:Spec 25Spec 25AARP MedicareCompletePlan 2 (HMO)AARP4MedicareCompletePlan 2 (HMO)H0609PBP# 027H0609 PBP#027For MembersFor MembersWebsite: omCustomerCustomerService: Service:1-877-370-2843TTY 711 TTY 7111-877-370-2843NurseLine:1-877-365-7949TTY 711 TTY 711NurseLine:1-877-365-7949BehavioralHealth: Health:1-800-579-5222TTY 711 TTY 711Behavioral1-800-579-5222For Providerswww.optumcare.comFor 8297Y0066 150609 163758 AcceptedMember ID:9999999-99MemberID: 9999999-99Group Number:HCFAD7Group Number:HCFAD7Member: Member:PLAN CODE:PLANRM9CODE: RM9SUBSCRIBERBROWN BROWNSUBSCRIBERPayer ID:Payer ID:2LIFE1LIFE1PCP Name:PCP Name:PROVIDERBROWN BROWNPROVIDERPCP Phone:999-9999PCP(999)Phone:(999) 999-9999RxBin: RxBin:610097 610097OPTUMCARERxPCN: RxPCN:999999993 OPTUMCARERxGrp:SHCO SHCORxGrp:Copay: PCP 10PCP 10 ER 75 ER 75Copay:Spec 45Spec 45AARP4MedicareCompletePlan 1 (HMO)AARP MedicareCompletePlan 1 (HMO)H0609 PBP#026H0609PBP# 026Y0066 150609 163758 AcceptedPO Box 29830Hot Springs, AR 71903-9830Health Plan(80840):HealthPlan 911-87726-04(80840): 911-87726-04PO Box 29830Hot Springs, AR 71903-983016 Medical ClaimAddress:P.O. Box 46770MedicalClaim OptumCare,Address: s, NV 89114-67705For Pharmacists1-877-889-6510For Pharmacists1-877-889-6510Pharmacy PharmacyClaims OptumRxBox 29045,Hot29045,Springs,ARSprings,71903 AR 71903ClaimsPOOptumRxPO BoxHotCustomerService- 8 pm 7 days/weekCustomer ServiceHours:8 amHours:- 8 pm8 7amdays/weekFor MembersFor com1-800-950-9355TTY 7111-800-950-9355TTY 7111-877-365-7949TTY 7111-877-365-7949TTY 7111-888-777-2735TTY 7111-888-777-2735TTY 711www.optumcare.comFor Providerswww.optumcare.com6 For Providers1-888-866-82971-888-866-82975Claim Address:OptumCare,Box46770LasNVVegas,NV 89114-6770Medical MedicalClaim Address:OptumCare,P.O. Box P.O.46770LasVegas,89114-6770For Pharmacists1-877-889-6510For Pharmacists1-877-889-6510PharmacyClaims OptumRxBox Hot29045,Hot Springs,AR 71903PharmacyClaims OptumRxPO Box PO29045,Springs,AR 719031. Participating Health Plan Logo2. Payer ID3. Network name4. Plan name5. Provider services toll free number6. Medical claims addressProvider guide8
OptumCare websiteOur website, optumcare.com, provides contracted network providersand patients with access to timely information, updates, and resources.Patient websiteProvider websiteOn the patient portion of the website,existing and potential patients can explorethe various services OptumCare offers.Features include:On the provider portion of the website,non-contracted physicians and otherhealth care professionals can learn moreabout what it means to be part ofOptumCare, and the philosophies that guideour approach to care. There are also valuablework resources for the network contractedproviders including: A community center page with informationabout fitness classes, health relatedpresentations, and social events.An up-to-date community centercalendar is also available FAQs to address the most commonquestions from existing andpotential patients A provider lookup tool that allows patientsto find primary care physicians, specialistsand facilities in OptumCare A page where potential patients canrequest more information by mail or email Information about prior authorizations,urgent care locations, skilled nursingfacilities and more Health-related news and articles on topicssuch as diabetes, cancer screeningsand cardiovascular diseaseMembers can also access a securedpatient portal to access their secure emailauthorization and claims information online.9Provider guide Prior authorization forms andelectronic processing Home health and care coordinationorder forms Referral reference guides for variousspecialties, including locations forcardiac services, nephrology, andskilled nursing facilities User guide for creating an accountfor the OptumCare Provider Portal Coding tips and tools
OptumCare provider portalAbout the provider portalThe OptumCare provider portal is designed specifically for our contracted providers. It offersprovider offices access to key patient authorization and claims information online, along withother value-added services.Using the provider portal, provider staff can: Verify patient eligibility Search prior authorizations and claims Send secure emails to our service center,utilization management, eigibilityand claims staff Search for contracted physicians to referpatients for servicesThe provider portal can be a greattool to help eliminate lengthyphone calls and faxes. It can alsobe of assistance if you are doingpaperwork before or after normalbusiness hours. Submit requests for prior authorization Submit notification of patient hospitalization Select data by TIN for multi-TIN providers Obtain reports and helpful forms Update your account profile and resetyour passwordsProvider guide10
How to get accessTo gain access to the Provider Portal, visitsecure.optumcare.com/provider/account/logonIf your office does not currently have portal access, you will need to designate an accountadministrator and have them create a new account. The account administrator will beresponsible for creating and editing user profiles for your providers, as well as resettingpasswords and editing accounts. Once the designated account administrator fills outand submits the registration form found under the “Create Account” link, your accountinformation will be delivered via email in about two business days.11Provider guide
OptumCare customer serviceBy phoneSecure emailThe phone number for providers to contactCustomer Service is 1-877-370-2845. Serviceadvocates are available to answer questionsMonday through Friday.Service advocates can also be reached bysecure email through the Provider Portal neOur secure email allows contracted providersto submit questions on important topics suchas correcting claims payments, submitting orinquiring about prior authorizations and more.Any provider who has access to the securedportal can use this feature. When you submita question via the web portal, you will receivea response within 24 hours. Emails received onweekends will be responded to the followingbusiness day. All questions and replies sentthrough this system are encrypted to ensuresafe transfer of personal health information.For faster service regarding claimsor authorization inquiries, access thesecure Provider Portal rience the benefitsof online access: No wasted time on the phone, holdingfor information Accessible 24 hours a day, 7 days a week Quick and easy access to view claim,authorization and eligibility information No additional cost/fee for this featureProvider guide12
Language &hearing impaired assistanceOptumCare wants to make sure that all patients get their questions answered on topics likebenefits, claims and prior authorization. For those that may need translation assistance, thereis help available upon request and at no cost to your patients.Language assistanceHearing impaired assistanceFor patients that are more comfortablespeaking to a bilingual service advocate,one can be assigned when the patientcalls OptumCare, or we can bring aninterpreter on the call to assist.There is also access to assistance forpatients that are hearing impaired. Let yourpatients know that assistance is availableby using their text telephone (TTY) or bydialing 711 from any telephone.For more information, call OptumCareat 1-877-370-2845. The TTY/711 andlanguage lines are open 24 hours a day, 7days a week. The Service Center is availableMonday through Saturday 8 a.m. – 8 p.m.EligibilityThe eligibility department receives patient information from the health plans on a daily basis.Once this information has been received, it is loaded electronically into the system.This information is reviewed by the eligibility department staff to ensure that the eligibilitydata matches the information submitted by the health plans. Information is being constantlyupdated and revised as it is provided to OptumCare by the health plans.13Provider guide
ClaimsATTENTION: Office managers and billing managersProvided in the following sections is key information for claim submission andre-submission to initiate claims payment.Topics addressed: Claim submission and field requirements EDI (Electronic Data Interchange) Claim PaymentPolicy & Processing Standard Billing Reading a Provider Remittance Advice (PRA) Time frames Definitions Helpful HintsCorrected claims can be submitted electronically byfollowing the guidelines below:Professional claims1. On the CMS-1500 form, enter frequencycode “7” in the Medicaid Resubmission field(box 22). The provider can enter the claimnumber in the Original Ref No. field, which isalso in box 22.OptumCare preferred methodof claim submission is electronic,known as Electronic DataInterchange (EDI). EDI is thecomputer-to-computer transfer ofdata transactions and informationbetween trading partners (payersand providers). EDI is a fast,inexpensive and safe methodfor automating the businesspractices that take place on a dailybasis. There is no charge fromOptumCare for submitting claimselectronically to OptumCare.2. In the Additional Claim Information field(box 19), add a note indicating the reason forthe resubmission (i.e. changed CPT code, addeda modifier, corrected EOB was received, etc.).Facility claims1. On the CMS-1450 form, in the Type of Bill field(box 4), enter frequency code “7.”This will indicate the claim is a corrected claim.Provider guide14
Electronic data interchange (EDI)OptumCare encourages and supports Electronic Data Interchange (EDI), particularly claimsand encounters. Electronic claims submission allows the provider to eliminate the hassle andexpense of printing, stuffing and mailing your claims to the network. It substantially reducesthe delivery, processing and payment time of claims. There is no charge for submittingclaims electronically to the network. Providers are able to use any major clearinghouse.Payer ID: LIFE1Benefits of EDI:EDI format: Reduces costsEDI has a standardized format, whichensures that data can be sent quicklyand is interpreted on both sides. EDItransactions adhere to HIPAA regulationsand American National StandardsInstitution (ANSI) standards. The EDIspecifications are like blueprints for thedata that guide the data to make thetransitions between different data tradingpartners as smooth as possible. No more handling, sorting, distributingor searching paper documents Keeps health care affordable tothe end customer Reduces errors Improves accuracy of informationexchanged betweenhealth care participants Improves quality of health care deliveryand its processes Reduces cycle time Enhanced information isavailable quicker Ensures fast, reliable, accurate,secure and detailed information15Provider guide
As of March 31, 2012, health care providers must be compliant with version 5010 of theHIPAA EDI standards. The current format that is used is 837, ANSI x12. 837i – Institutional claims 837p – Professional claimsAdditional transactions performed by OptumCare: 997 – Functional acknowledgement (claim receipt acknowledgementvia clearinghouse)For paper submissions, please review the following to ensure that your claimis received and processed accordingly.Paper submission: Professional vendors must submit on a CMS 1500 Ambulatory surgery centers with appropriate modifier SG or TC Hospital and facility vendors must submit on a CMS 1450Claim submission addressOptumCare claimsPO Box 46770Las Vegas, NV 89114Provider guide16
BillingComplete (clean) claims are those claims and attachments or other documentationthat include all reasonably relevant information necessary to determine payer liability.To be considered a complete claim, the claim should be prepared in accordance withthe National Uniform Billing Committee standards and should include, but not be limitedto, the following information:A claim form that contains: A description of the service rendered usingvalid CPT, ICD-10, HCPCS, and/or revenuecodes, the number of days or units for eachservice line, the place of service code/billtype and the type of service code; Patient demographic information; Provider of service name, address, NationalProvider Identifier (NPI) number and taxidentification number; Date(s) of service; Amount billed; Signature of person submitting the claim;and Other documentation necessary in orderto adjudicate the claim, such as medicalreports, claims itemization or detailedinvoice, medical necessity documentation,other insurance payment information,referring provider information, attendingprovider information and associated NPIas applicableIncomplete claims or claims requiring medical records in order to make a determinationof payer liability will be contested back to the provider via EOB with a descriptive reasoncode informing the provider what additional information is needed. Medicare claims will bedeveloped in accordance with CMS regulations. Any claims submitted with invalid codes orclaims missing required billing elements will be mailed back to the provider with reason codesattached requesting a corrected claim.All payments and co-payments are subject to the benefit information as defined by thepatient’s specific health plan benefit plan. Claims payment is always dependent on patienteligibility status on the date of service as determined by the health plan.17Provider guide
Reading the provider remittanceadvice (PRA)Information is listed on the PRA in addition to the amount paid. See the end of this sectionfor a detailed explanation of each field.Denied claims are listed on the PRA with a detailed denial reason or reasons; these are helpfulto refer to when submitting a provider dispute, correcting a claim or contacting the ServiceCenter with questions regarding a claim.Electronic funds transfer (EFT)OptumCare offers EFT/ERA solution through our preferred vendor, InstaMed.Benefits include: Free integrated ERA/EFT including trace number linking the ERA and EFT. Quick registration, with only 8 to 10 business days before you receive yourfirst payment. No disruption to your current workflow – there is an option to have ERAs routed toyour existing clearing house. View payments at summary and detail level with intuitive reporting. Receive live InstaMed customer service support from 7:00 a.m. ET to 9:00 a.m.ET via phone, email and web.Please note: If you are already enrolled with InstaMed for ALL PAYERS, you willautomatically begin receiving InstaMed EFT transactions in April 2017 from OptumCare.If you are enrolled with another ERA/EFT vendor through OptumCare, you can quicklyre-enroll through InstaMed.To register visit instamed.com/eraeft or call 1-866- 945-7990 with any questions.Provider guide18
Claims & encounter submissionsFor proper payment and application of co-payment, deductible and co-insurance, it isimportant to accurately code all diagnoses and services in accordance with national codingguidelines. It is particularly important to accurately code because a patient’s level of coverageunder his or her benefit plan may vary for different services. You must submit a claimand/or encounter for your services, regardless of whether you have collected the co-payment,deductible or co-insurance from the patient at the time of service. All claims are validatedusing clinical editing software to check for coding accuracy.AnesthesiaDRG/APC reimbursementsAnesthesia is processed followingthe American Society of Anesthesiologists(ASA) guidelines.DRG/APC reimbursement is validated usingan outside vendor to verify DRG groupingand provide appropriate CMS pricing. One (1) unit fifteen (15) minutesof anesthesia timeDRG claims may be reviewed, post-payment,to determine necessity for DRG validation,which include complete review ofmedical records. All anesthesia time is prorated androunded to the nearest tenth 5010 EDI transactions must be reported inminutes. Should the procedure code haveminutes in the description, then units arestill acceptableImmunizations andinjectable medications Must include the appropriate National DrugCode (NDC) number and the correspondingquantity for each NDC unit dispensed Must include the appropriate HCPC/CPTcode and corresponding quantity for eachHCPC/CPT unit dispensed Reimbursement is based upon CMSpayment methodology for Part B drugs19Provider guideFee schedulesReimbursement is based on the currentMedicare Fee Schedule for the appropriategeographical area unless otherwise statedin the provider’s contract.
ModifiersMultiple proceduresThe AMA industry standard modifiers areacceptable for billing. The Correct CodingInitiative (CCI) guidelines for claims paymentand use of modifiers are used whenadjudicating claims.Multiple surgeries performed by the samephysician on the same patient during thesame operative session are reimbursed inaccordance to Medicare guidelines, unlessotherwise stated in the provider’s contract.CPT defines the standard, acceptable modifiersto be used for professional claims. HCPCS alsoincludes acceptable modifiers for services notdefined by CPT. OptumCare accepts modifierspublished by CPT and HCPCS.Submission time framesKeep in mind when submitting claims, whether it is electronic or paper, there are requiredtime frames that must be kept by all parties involved.Submitter: Timely filing limit is 90 days or per the provider contract. A claim submitted afterthis time frame may be denied.Please see provider dispute section of this manual for
Mental health: Please refer to the back of the patient ID card for information on the mental health provider network. Optum Behavioral Solutions: 1-800-579-5222 or Crisis Preparation & Recovery, Inc.: 1-480-804-0326 Durable medical equipment and infusion services: Preferred Homecare Phone: 1-480-446-9010