Transcription
SUMMER 2019 VOLUME 15 NO. 2DukeNursingAdvancing Nursing Education, Research and Clinical PracticeCreating Pathways forInnovation4 Creating New Pathwaysfor Innovation14Powering Innovative Connections322019 Alumni Awards
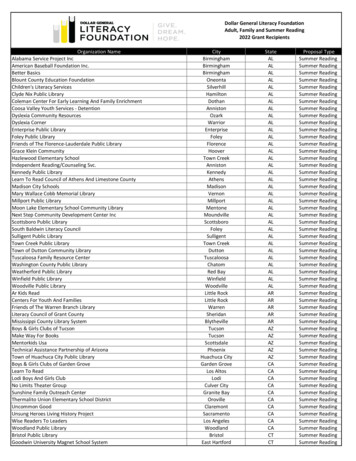
DukeNursingmagazineSUMMER 2019 VOLUME 15 NO. 2DUKE NURSING DEVELOPMENT AND ALUMNI AFFAIRS STAFFAnita StallingsAssociate Dean, Developmentand Alumni AffairsDiana StaplesSenior Director, DevelopmentMarla GreggDirector, Alumni and DevelopmentProgramsSarah BlumigDirector, Annual Giving andthe Bessie Baker Society4Creating New Pathwaysfor InnovationCreating Pathways forInnovation4 Creating New Pathways for Innovation14 Powering Innovative ConnectionsCREATIVE DESIGNHopkins Design GroupPHOTOGRAPHYKara CockerellDevelopment AssociateKen Huth and Andrew BuchananCheryl BelcherStaff AssistantPRODUCED BY DUKE UNIVERSITYSCHOOL OF NURSINGEDITORIAL STAFFMarketing and CommunicationsDepartmentAmy BaskinAssistant Director, Marketingand CommunicationsCopyright Duke UniversitySchool of NursingLaWanda McCrearyCommunication StrategistStephanie SchellerPublic Relations SpecialistNURSING BOARD OF ADVISORS JANUARY 2019 – DECEMBER 2019Bimal R. Shah, MD‘01, MBA’01ChairEMERITUS MEMBERSGale AdcockCharles C. McIlvaine, T’87Guy Cole Arnall, Jr., T’8532 2019 Alumni AwardsWRITING TEAMCristina SmithLaWanda McCrearyStephanie SchellerMarla GreggBernadette GillisAliza InbariDaniel T. Blue III, T’95, L’01, B’01Christy W. BellSheppard ZinovoyMichele Chulick, BSN’77Lynn K. ErdmanSchool News20New Faculty, Recent Grant Awardsand Promotions23Accomplishments & Honors40Class Notes44ObituariesOn the cover: Innovation@ DUSON graphic 2019 Ryan Shaw, PhD, RN and Duke University School of NursingDuke Nursing Magazine is published bythe Duke University School of Nursing. Issuesare available online at nursing.duke.edu.Your comments, ideas and letters to theeditor are welcome. Please contact us at:Duke Nursing Magazine, c/o Marketing andCommunications Department, DUMC 3322,307 Trent Drive, Durham, NC 27710,919-684-9356, michael.evans2@duke.edu.L. Sue Frederick, N’77, MD’83Ruby G. Holder, E’88, B’93Norma MartiJoanne L. Mazurki, T’74Bettye M. Musham, N’54Orit SzulikJames E. Vanek Jr., T’01Brett. T. Williams, T’81NURSING ALUMNI COUNCIL JULY 1, 2018 – JUNE 30, 2019OFFICERSKathleen V. Gallagher, BSN’75Marianne Tango Williams, BSN’81PresidentLaura T. Gantt, BSN’79Elizabeth A. Lee, BSN’82Vice PresidentAliki H. Martin, DNP’13M. Christine Fulgencio, MSN’99SecretaryLouisa Soler-Greene, DNP’14, MSN’13MEMBERSJudith A. Thorpe, BSN’77Karen Jacobus Baxter, BSN’84S. Celeste Toombs, MSN’00, GNC’02Susan Beck Davis, BSN’77Constance E. Vaught, BSN’73Andrew R. Benson, MSN’09Mary Ellen Wright, BSN’81Ellen G. Donaldson, BSN’81K. Becky Zagor, BSN’80V. Laurie Griggs, BSN’80Christine S. Pearson, BSN’84Joan M. Stanley, BSN’71
Dean’s WelcomeInnervating InnovationNursing and health care innovation doesnot necessarily require a lot of resources(although they certainly help), but itdoes require focus, a willingness to openourselves up to new ways of thinkingabout our profession, exploring newcollaborations with colleagues with whowe may not have traditionally worked,and to accept the risk of failure.I invite you to learn how we at Duke areattempting to innervate innovation withineducation, research, clinical practice andhealth care policy. I sincerely hope someof our experiences will spark a newidea or two for your nursing community,or stimulate a conversation about howtogether we can build upon the best ofour profession and prepare for a veryexciting future.Sincerely,Marion E. Broome, PhD, RN, FAANDean and Ruby Wilson Professor of Nursing,Duke University School of NursingVice Chancellor for Nursing Affairs, Duke UniversityAssociate Vice President for Academic Affairs for Nursing,Duke University Health SystemD U K E N U R S I N G S U M M E R 2 019Innervating means “to stimulate to action”and “to supply with energy.” It requiresa new way of thinking and new, excitingcollaborations with others. At DUSON,we are creating a culture in which facultyand staff are encouraged, stimulated andeven expected to develop new, creativeways to address challenges in education,research and clinical practice.Each of us gets out of bed every morningwith a passion for at least one aspect ofnursing. It might be a passion for clinicalpractice, or for research or for education.If we as nursing leaders can focus thepassion that each of our organizationspossess, and encourage it towards creativeproblem solving today, while buildingcapacity for solving tomorrow’s problems,then we have created a true culture ofinnovation.1Throughout my career, I have firmlybelieved that if you bring a team ofnurses with diverse backgroundstogether in a room, that they can solveany problem you give them. Any problemat all. That is what real innovation isabout. As nurses, we don’t innovatejust to innovate, we innovate to createsolutions that address the problems andchallenges we face.
Behindthe ScrubsFollowing a presentation of a devicefor repositioning immobile patients inacute and long-term care at the 2017Duke Innovation Jam, an annual eventcreated and managed by the DukeInstitute for Health Innovation, apartnership evolved between DUSON,Duke Health and Seneca Devices.The product is designed to improvecaregiver productivity, reduce caregiverback strain and reduce life-threateningpatient complications. The deviceautomates the patient turning andboosting process, allowing onecaregiver to reposition the patient atthe push of a button.2D U K E N U R S I N G S U M M E R 2 019DUSON’s Health Innovation Labassisted with simulated field tests toassess the device’s safety, effectivenessand ease-of-use.Shown here testing the device in theDUSON Simulation lab are current PrattEngineering Student Venice Leone,inventor Samuel Fox E’18, MicheleKuszajewski, DNP, RN, CHSE,assistant director, Center for NursingDiscovery, Nashonda Thomas, staffassistant, Center for Nursing Discoveryand DUSON associate professor andDirector of DUSON’s Health InnovationLab, Ryan Shaw PhD’12, RN.
3D U K E N U R S I N G S U M M E R 2 019
4D U K E N U R S I N G S U M M E R 2 019Creating NewPathways forInnovation
5D U K E N U R S I N G S U M M E R 2 019
Fundamentally, nursing is about solvingproblems, whether it’s in a clinic, aclassroom or a lab. At Duke UniversitySchool of Nursing (DUSON) we understandthis and strive to educate our students inways that support creativity and innovation,core skills for problem-solving. In a digitalworld, where access to information isvirtually limitless, teaching and curricula must assumethe added challenge of capitalizing on new ideas andapproaches to health care while continuing to honorproven nursing practices and traditions.To Dean Marion E. Broome, PhD, RN, FAAN, andRuby Wilson Professor of Nursing, nurses are naturalinnovators. Especially when they come from a varietyof perspectives and experiences, she says, the sky isthe limit. “My observation has been you can give meany challenge, and if I can put a group of nurses in aroom together, who are very different and come fromdifferent backgrounds, we can make huge stridestoward solving the problem. I don’t care what it is.”Because today’s practitioners and researchers relyso much on readily available digital health information,faculty must continually adapt their approach toteaching, mentoring and guiding their students, sheadds. An important task they have is helping studentsfilter through the mass of information and resources,“Nurses are6D U K E N U R S I N G S U M M E R 2 019natural innovators.”since many students may not yet have the knowledgeto effectively interpret them. “The best teacherscan translate knowledge in a way that users can findaccessible,” Broome says.Being innovative in instruction is critical to keepingup with the dynamic and increasingly digital age ofhealth care because that is what practitioners and nursescientists are dealing with every day, and their learningprocesses must reflect that reality. It’s natural to teachhow one has learned, but because the world of scienceand information has changed so much, faculty have toacknowledge and adjust to those changes in not justwhat we know, but how we access and translate thatknowledge, Broome says. “Younger generations havedifferent ways of looking at information that sometimesincludes data, but also includes their impressions of otherpeople’s assessments of that data. It’s more a ‘groupthink’,” she says. “They trust their intuition more than Idid when I was a nurse scientist. I always wanted dataand more data to make decisions.”Even though a quick Google search can render almostevery bit of information on a topic, that informationbecomes much more powerful and complex in the handsof someone who has years of deep study and learning,heightening the importance of savvy instructors. “Ittakes a certain kind of thinking to really be innovative.I think almost everybody is innovative in some parts
“Beinginnovativein instruction iscritical to keeping upwith the dynamicand increasingly digitalage of health care.”“When those students go out into practice and aproblem arises on their unit, they’re going to think aboutsolutions in an entirely different way,” Broome says,noting that this type of teaching gives students the roomand support to collaborate and expand their thinking.One question faculty should be asking, Broome says, is“How do we really pull out the very best of our studentsand let them take their ideas and talents way beyondwhat we thought they could?”DUSON will be offering a new course on health careinnovation, created by Associate Professor RyanShaw, PhD‘12, RN, and director of the Duke HealthInnovation Lab (HIL). The class will be situated withinan inter-professional education framework, Shawsays, with the goal to teach not only nurses, but alsophysicians, physical therapists and engineers to work asa group to create change.“We’re trying to empower nurses to be able to actupon their ideas and unmet needs to improve health andhealth outcomes,” Shaw says, noting that collaborationwith other disciplines enhances problem-solving skills.“We will educate our students to think in different waysso that when they do graduate and they go into theirown practice, they have the skills and knowledge to beempowered to innovate.”The HIL provides the support and resources forstudents, faculty and practitioners at Duke who wantD U K E N U R S I N G S U M M E R 2 019Health Care Innovation7of their life. But innovation truly takes somebody who’sokay about failing at certain times and also is able tothen re-conceptualize their approach and see newpossibilities in order to move forward,” Broome says,noting that technology is one tool of innovation, but notthe ultimate one. “It’s one mechanism to use, but it’s notthe be all end all. Innovators rely on data, intuition andcues from disparate sources, combined with their visionof what could be.”Teaching students how to think creatively bystructuring classes in new ways is another way of beinginnovative. A class can be broken up into smaller groupsand given a case or problem to solve, Broome says. Forinstance, an observation about a consistent increase inno-shows at pediatric and prenatal appointments amongcertain groups of women should signal a need forchange. Students may be tasked with researching andgathering data about what has been happening, hearingfrom providers and the women about their perspectivesof the problem. They might also observe a typical clinicvisit from beginning to end or even take transportationwomen typically take to clinic. Then they collaboratein small groups to puzzle out what social, political oreconomic issues might be driving the increase and alsoto look at the downstream effects of more no-shows.Each group could come up with different viablesolutions for how to reverse the trend or deal with itsramifications, thus giving the class as a whole a broaderand more complex view of problem-solving.
“Innovators rely on data,intuition and cuesfrom disparate sources,combined withtheir vision of8D U K E N U R S I N G S U M M E R 2 019what could be.”to improve processes and patient care throughinnovative thinking and ideas. Whether it’s testingthe viability of a new product or brainstorming aboutchanging how data are collected, stored and used,the goal is to support creative potential, Shaw says.“I think it’s important for us to create a strategy sothat the School has direction for how to create newopportunities for both our students and faculty. Andwe also want to collaborate with practicing clinicianswho identify real-world problems within healthcare and to be able to make a difference.”Duke not only has the resources to innovate—through its faculty, funding sources, and state-of-theart labs and tools—it also has a tradition of altruism.“The beauty of being at Duke is that’s what we are allabout: knowledge in the service of society,” Broomesaid. Creating new ways to teach so that the newgeneration of nurses learn in a way that will servethem in a digital age can be a daunting task, but it’snecessary to the pursuit of excellence, she says. Butinnovation doesn’t mean change for change’s sake,Broome warns. It must be methodical and thoughtful.Her advice is to start with one course. “You don’tneed to reinvent the entire curriculum, start with justone course. Present students with a set of challengesin health care and let them try to solve them,” Broomesaid. “The outcomes could be exciting. Alternativelearning that acknowledges different approachesand perspectives on health care produces studentswho are better prepared to be critical and innovativethinkers, and ultimately better nurses when theygraduate,” she added.“The Accelerated Bachelor of Science in Nursing(ABSN) programs are perfect for this type ofapproach because these students all come withprevious degrees. So they already come with differentperspectives and approaches to problem solving—maybe one’s an engineer, one’s a sociologist,” Broomesays. “They’re going to learn much more from eachother and it will be a deeper learning experience.”And that’s what innovation is all about, Broomesays. “I look at DUSON and the intellectual and socialcapital here, it’s pretty amazing. We have peoplewho are incredibly strong researchers, incrediblystrong practitioners, incredibly strong educators. Andwhen they bring it to bear on a challenge or an issue,there’s very little stopping them.”Broome encourages other schools to find waysto foster innovation and creative problem solving.“Innovation doesn’t have to be expensive,” Broomesaid “Regardless of where you are, there is neverenough time and never enough resources. It’s reallyabout identifying new ways of thinking and doingwhat nurses already do so well.” n
INNOVATION @ DUSON Current need/problem? Brainstorm Prototype Test devices Cost Business plan Health Implications? List potentialsolutions Mockups Test processes ROI Product development Iterate Get feedback Clinical evidence Investment Data collectionINPUTS Prioritize ideas Improve design STUDENT SCHOLARS FACULTYOUTPUTS Clinical trial STUDENTS- MARKETABLE SKILLS- CAPSTONE / DISSERTATIONS CLINICIANS- CAREER OPPORTUNITIES INTERDISCIPLINARY PARTNERS PRODUCTS CARE DELIVERY MODELS ENTREPRENEURSHIPBy breaking down the process into iterative steps,this approach strengthens the potential for innovation.Adapted from the Design Thinking model at theHass-Plattner Institute of Design at Stanford University. INVESTORS SCHOLARSHIP REPUTATION LEADERSHIP HEALTH/HEALTH CARE POLICY 2019 Ryan Shaw, PhD, RN and Duke University School of NursingD U K E N U R S I N G S U M M E R 2 019to identify and solve complex unmet needs in nursing. GRANT FUNDING9This model provides a human-centered framework
NEW PATHWAYS FORClinical InnovationDUSON and Duke Heath System Partner to LaunchDNP Quality Improvement Scholars Program10D U K E N U R S I N G S U M M E R 2 019Across the country, there issignificant demand within healthcare organizations to improvethe quality of individual patient careand the health of populations, whilereducing costs. Clinically, DNP-preparednurses are well qualified to lead entityor system-wide quality and safetyimprovement initiatives, but may lacksome of the specific knowledge in theareas of data analytics and implementation science.The DUSON-DUHS QualityImplementation Scholars Program,a unique three-year pilot programbetween DUSON and Duke Nursing,was created through a collaborationled by Marion E. Broome, PhD, RN,FAAN, dean of Duke University Schoolof Nursing and Mary Ann Fuchs,DNP’10, MSN’90, RN, NEA-BC, FAAN,vice president of patient care andsystem chief nurse executive for DukeUniversity Health System.The first cohort of four DUSONDUHS Quality Implementation Scholarsbegan a 12-month certificate programthis summer. The students selectedare already leaders in their field and willcontinue to grow as quality improvement experts.“This partnership is the first ofits kind, and will allow senior-levelDNP-educated nurses to develop theskills necessary to provide solutions andimplementation plans for improvingBroomeFuchsquality of care for our patients and theirfamilies who we serve, said Broome.“At DUSON, we are creating innovativepartnerships that can change thetrajectory of the role of nursing in majorhealth systems.”“The initial cohort is rich withexperience and expertise. These nurseleaders will be on the cutting edge ofimplementing new quality processesthat will have a significant impact on thepatients that our health system serves,”said Fuchs.“DNP-prepared nurses within theDuke Health System are an untappedresource as we explore ways toimprove the quality of care and patientoutcomes,” said Staci Reynolds, PhD,RN, ACNS-BC, CCRN, CNRN, SCRN,lead faculty for this Program. “In ourhealth system, DNP-prepared nursesReynoldshold a variety of roles in administrationand advanced practice. They serveas formal and informal leaders whocan, with the additional knowledgegained through the program, providethe practical expertise and leadershipto affect organizational change on alarger scale.”Scholars will participate in coursesfocused on analytic, methodologic andleadership competences associated withimplementation science. In additionto their full-time responsibilities in thehealth system, scholars will implementa quality improvement project utilizingdata from existing databases and/or the electronic medical record toevaluate the effectiveness of a changeon quality, safety, cost and patientoutcomes. n
NEW PATHWAYS FORPolicy InnovationA Nursing Perspective Enhances Health Policy DiscussionsMargolis Scholars Lauren Arrington (l)and Michelle Franklin (r) joinDean Marion E. Broome in Washington D.C.Margolis Program, by bringing diversedisciplines together, provides a richopportunity for real world application.The coupling of health policy educationin an interdisciplinary setting is crucialfor translating knowledge into action.”continued on page 12D U K E N U R S I N G S U M M E R 2 019reforms, as well as improving modelsfor drug access and development.Initially, the cohorts included Dukestudents representing public policy andlaw. However, in 2018 two nursingstudents—one DNP and one PhD—were added to the program, and in2019 the cohort is being expanded toinclude medical and business students.“I am thrilled to have nurses represented among our Margolis Scholars,”said Mark McClellan, MD, MPH,director of the Duke-Margolis Centerfor Health Policy and Robert J. Margolis,MD, professor of business, medicineand health policy. “As someone whohas studied and worked on methods toexpand the role of nurses in alternativepayment models and care deliverymodels, I am deeply committed toenhancing the role of nurses in improving health outcomes,” McClellan said.PhD in Nursing student MichelleFranklin and Lauren Arrington fromthe Doctor of Nursing Practice Programwere selected as DUSON’s first studentsto be admitted to the Margolis ScholarsProgram.For Franklin, a pediatric nurse practitioner, the Margolis Scholars Programis helping to change how nursingis viewed in broader health policydiscussions. “We gain health policyexposure in our individual programs anddisciplines,” said Franklin. “However, the11Advocacy has always played acentral role in nursing. Whetheradvocating for a single patientor on a larger public health issue,nurses can provide a unique voice andperspective to health care discussionsat the local, state and national level.“Our roots in advocacy go as farback as the early 1900s when nursesworked with underserved populationsto push for public health and healthcare policy changes, said Dean MarionE. Broome PhD, RN, FAAN. “Todayit is more than just advocacy, nursesmust be able to incorporate evidenceinto their advocacy. Given that manypeople who work in health policy aren’tclinicians, nurses can help bring thatperspective to conversation.”Through an innovative partnershipand program at the Margolis Centerfor Health Policy at Duke, nurses’experiences as both researchers andclinicians are being brought into healthcare discussions in a very unique way.The Margolis Scholars Program inHealth Policy and Management is aninterdisciplinary cohort approach forgraduate and professional studentsto engage in real-world public healthpolicy advocacy. The two-year programcombines academic and experientialtraining in health policy and management working on practical challengesincluding Medicare and other payer
NEW PATHWAYS FORPatient Care InnovationHealth Policy Discussions12D U K E N U R S I N G S U M M E R 2 019continued from page 11The Margolis Scholars Program ismeeting both personal and professional aspirations for Arrington. “Ibecame a nurse-midwife so thatI could develop clinical skills toserve my community and understand their needs and experiences,”she said. “Most graduate studentsare siloed in their particulardiscipline. Through the MargolisScholars Program, we establisha precedent for interdisciplinarycollaboration that will follow usthroughout our careers. We have aseat at the table.”“Working with Mark McClellanand the Margolis Center has provideda wonderful opportunity for ourDNP and PhD students to workon high-powered interdisciplinaryresearch teams,” said Broome. “Theycan hone their articulation skills tolend a voice as well-educated nurseresearchers and clinicians that willhelp ground health policy in the realworld.”The Robert J. Margolis, MD, Centerfor Health Policy was established inJanuary 2016 with a 16.5 million giftfrom Duke medical school alumnusRobert J. Margolis and his wife Lisa,through the Robert and Lisa MargolisFamily Foundation. The Center'smission is to improve health and thevalue of health care through practical,innovative and evidence-based policysolutions. nTransition to Home Care Innovations ReducesReadmissions—Improves Patient OutcomesDEFT Center Creator, Cristina Hendrix conducts a training class for family caregiversprior to their patient’s discharge.When an older patient isdischarged from the hospital,everyone is hopeful the patientcontinues to recover and rehabilitate.Avoiding hospital readmission is atop priority—not just from the patientand their family’s perspective, butalso from a financial one. It’s costly onmany fronts when a patient returns forhospitalization. For the past two years,the Duke Elder Family/Caregiver Training(DEFT) Center has been uniquelyaddressing this issue, improving 30-dayreadmission rates through an innovativeapproach to post-hospitalizationsupport of elderly patients.Research by DEFT founder CristinaHendrix, DNS, CNP-BC, FNP, FAAN,associate professor at DUSON, showsthat training and direct follow-upwith a patient’s support group posthospitalization are keys to avoidingreadmission. “The involvement of familyand friends is critical to preventing thoseadverse events from occurring in elderlypatients as a result of not knowing whatto do when they’re recovering at home,or not fully following post-hospitalizationinstructions,” Hendrix said. “We wantto increase the level of confidenceand preparedness in home caregivingand minimize preventable 30-day
to understand the situation.” Providinginformation that can be absorbed andacted upon is an important aspect of theDEFT approach.Looking beyond DEFT, Hendrixenvisions caregiver support and trainingbeing employed for other situations,such as for chronic disease managementwith an aim of preventing the firsthospitalization, or during the transitionto end-of-life palliative care. “We startedwith post-hospital or the hospital-tohome transition. Our intent is not to stopthere, “Hendrix said.At DUSON, Hendrix has created anelective course on caregiver training.Pre-licensure ABSN students also havethe opportunity to observe the graduatestudents as they train caregivers, to enrichtheir education outside the classroom,Hendrix said.Hendrix believes DEFT has provenitself clinically, and she is now focusedon creating a business plan that iscost-effective and sustainable so thatthis innovative approach may reach itsfull potential, not only at Duke, butelsewhere.“If we can demonstrate to the otherhospitals and schools of nursing howwe were able to put an idea into actionand with good outcomes,” Hendrix said,“then it might interest them to replicateus.” nD U K E N U R S I N G S U M M E R 2 019that I gained from my exposure to theDuke Elder Family/Caregiver program wasthe caring and genuine concern for thepatient, as well as the care and concernfor me the caregiver,” he said. “No oneelse seemed to know what struggles thatI was a going through as a caregiver andit was so good to talk to someone whowould listen and offer help as needed.”Hendrix said after closely assessingthe program since its launch in spring2017, she has additional ideas forimproving the training and expandingit beyond post-hospitalization. Forinstance, making it easier for caregiversto access training is one area for possibleimprovement. Hendrix said somecaregivers face obstacles with schedulingor transportation to their assignedtraining sessions. She believes it’spossible to overcome these barriers byproviding some of the training digitally,using a closed system where informationis downloaded for the caregiver to accessat home on a mobile tablet.“Caregivers are thirsty for knowledgeof certain points in time along thechronic illness trajectory. If everything isgoing well, the caregivers may not be asinterested. But if there’s a crisis—duringhospitalization, during an initial diagnosisor after discharge—that’s when theyneed the knowledge and will absorb asmuch as they can because they want13readmissions among the patients.”The DEFT program, funded for threeyears by The Duke Endowment, bringstogether case managers, physiciansand nurses to broaden care protocolsto include what happens after a patientis released from the hospital. Providersidentify family or friends who will helpthe patient at home and refer them toDEFT. Before the patient is discharged,their caregivers receive training, includinglearning how to do simple procedures.The training also educates caregivers onmanaging follow-up appointments andprescriptions, and identifying red flagsthat would signal the need for immediatemedical intervention. In addition to thetraining, caregivers also receive follow-upphone calls during the first 14 days aftera patient’s discharge to answer questionsand ensure better compliance withdischarge instructions.According to one caregiver, “the DEFTprogram was introduced to me when mywife was in Duke suffering from kidneyfailure. I participated in the trainingsession while my wife was just startingdialysis. The support from the DEFT staffwas superb. Once discharged from Duke,the DEFT staff kept in contact with me,asking what resources that I needed.”Looking beyond simply trainingcaregivers, the impact the DEFT programmakes is tremendous. “The greatest thing
Innovation in nursing happensat multiple levels, but it all startswith an idea. Some ideas aresimple and grow from a practicalneed a nurse might face inclinical care. Other ideas may bemore complex, and involvePowering InnovativeConnectionsthe use of technology or computeralgorithms and databases toassist the research of a nursescientist. In all cases at DukeSchool of Nursing (DUSON) ,ideas have fertile ground in whichto flourish in large part becauseof a supportive environment14D U K E N U R S I N G S U M M E R 2 019and multi-disciplinary collaboration.
Health Innovation LabThree years ago Ryan Shaw, PhD‘12, RN,associate professor and Elizabeth C. ClippTerm Chair of Nursing and director of theDuke Health Innovation Lab (HIL) at DUSON,needed a place to test new technology in aclinical environment. He created the HIL toprovide structure and a physical home forclinicians, nurses, doctors and even engineersand computer scientists to explore their ideasin a practical setting.“It’s a place to be able to ideate, prototypeand test concepts,” Shaw said, noting thatbefore the lab, there was a limited supportprocess to follow through on ideas beinggenerated by nurse faculty and clinicians.“There was no pathway if you did inventsomething, or you found a new way todeliver care to know what to do next. Ifyour concept was successful, then whatdid you do? Who could you talk with foradvice about whether or not you couldmove forward with a patent prototyping orfeasibility testing in the hospital?”The HIL, in conjunction with the School’sBusiness Development Office and resourceslike the Duke Innovation & Entrepreneurship“It’s a place tobe able to ideate,prototypeand test concepts.”Ryan Shaw, PhD‘12, RN15D U K E N U R S I N G S U M M E R 2 019Ryan Shaw, PhD’12, RN, works with ABSN students on TRINA, a collaborative robotics projectbetween the DUSON’s Health Innovation Lab and the Pratt School of Engineering
16D U K E N U R S I N G S U M M E R 2 019Marybeth Tetlow, MSN’17 explain
4 Creating New Pathways for Innovation NURSING BOARD OF ADVISORS JANUARY 2019 - DECEMBER 2019 Bimal R. Shah, MD'01, MBA'01 Chair Gale Adcock . critical to keeping up with the dynamic and increasingly digital . DUKE SUMMER 2019. DUKE NURSING SUMMER 2019. SUMMER 2019, , SUMMER 2019, and . DUKE