Transcription
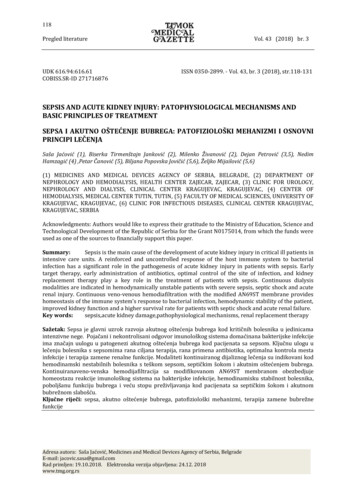
Critical Sepsis- Emergency DepartmentSigns & Symptoms ofCritical Sepsis Inclusion Criteria:Any patient 30 days old withclinical concern for critical sepsis/septicshock ORSepsis RED ANDED Attending/Fellow assessmentwith concern for critical sepsis/septic shockExclusion Criteria:Burn patientsHypotension (MAP 5thpercentile for age)TachycardiaPoor perfusionReduced urine outputTachypnea/new oxygenrequirementMental status changes!RN callsSEPSISTriage Alert forSEPSIS REDs Primary team huddle to evaluate for sepsis(RN/Team Leader, LIP, Surgeon when appropriate) Notify AttendingDeviation from pathway requires detailed documentation SHOCK TIMEGOALSDoespatientmeetCritical SEPSIScriteria?Time Zero Patient flags sepsis redOFF PATHWAYResume routine careNOYES5minActivate Critical Sepsis Pathway/Order Set Provide supplemental oxygen as needed (oral/nasal ETCO2 for perfusion deficits)Reassess vital signs every 5 minutesOrder appropriate antibioticsAccess 15minPlace 2 large borePIVs if no centrallineConsider PIV inpatients withcentral lineIf 2 unsuccessful IVattempts: considerIO 30min 60min LabsBlood/urine culturesiSTAT VBGPOCT GlucoseCBC diffCorrectUAglucoseBMPand calciumCRPProcalcitoninConsider Type & ScreenLactate-order STATMagnesiumPhosphorusConsider PT/PTT/d-dimerConsider lumbar puncture 1 year old!Administer AntimicrobialsAppropriate antibiotics for specific populations: HemOnc Suspected Infection Central Line Infections Previously healthy patients with/without intraabdominal source Medically complex patients with/without intraabdominal sourceConsider history of resistant organismsSurgical consult for suspected infection requiring sourcecontrol (e.g. skin/soft tissue, intra-abdominal)Initiate vasoactive/inotropic dripsfor Fluid Refractory Shock Epinephrine for cold shock Norepinephrine for warm shock Obtain additional access ifneeded Consider broadening antibioticcoverageInitial Fluid Resuscitation ! Ongoing ResuscitationAdminister 2nd and 3rd bolus of 20mL/kgnormal saline RAPIDLY via push-pull orpressure bag, until perfusion improvesor rales or hepatomegaly developOrder vasoactive/inotropic dripsConsider blood products Bedside Huddlewith ED, ICU, /Inpatient Admitting LIPLIP-Document outcome of huddleRN-SepsisreassessmentAdminister 1st bolus of 20mL/kgnormal saline RAPIDLY via push-pullor pressure bag within 5-15 minutesConsider 5-10mL/kg boluses ifconcern for fluid intolerance(cardiac/ renal dysfunction)Consider hydrocortisone stressdosing in pt. with adrenalinsufficiency or petechia/purpura Respiratory SupportConsider ET intubation forhypoxemic respiratory failure orpersistent shock despiteadequate resuscitation andinotropic support (obtain CXR forETT verification) using shock safemedications NO ETOMIDATEConsider BiPAP as an alternativeInpatient Admit CriteriaIMU Admit Criteria(ACNW – use clinical judgementfor transfer to ACLR) Normotensive after 40mL/kg NS bolusesWell appearing withreassuring labsFirst dose of antibioticsadministeredImproving tachycardia(ACNW – use clinical judgementfor transfer to ACLR)ICU Admit/Transfer to ACLittle Rock Criteria:Any of the followingand/or other concerning clinical findings: E. Rader 4-1659Approved by P&T committee 9/15/20Approved by PCOC 10/6/20Ventilatory supportVasoactive/inotropicsupportHypotension despitefluid resuscitationvolumeLactate 4mmol/LpH 7.3Base excess greaterthan -6mmol Ill appearingCold shockTachycardia not resolvedafter interventionCR 3 sec after 60mL/kg NS bolusesMAP according to thefollowing: 1.5(age inyears) 40; 14 years oldand greater MAP 60mmHgNeed for critical caremanagement Need for monitored bedNormotensive after40-60mL/kg NS bolusesIncreased assessment needsIncreased vital sign needsIncreasing HFNC support
Signs & Symptoms ofCritical SepsisNew Onset Critical Sepsis –General Care Inpatient PhaseHypotension (MAP 5thpercentile for age)TachycardiaPoor perfusionReduced urine outputTachypnea/new oxygenrequirementMental status changesInclusion Criteria:Any patient 30 days old withclinical deterioration AND concern fornew or evolving critical sepsis/septicshock AND/OR that flags Sepsis RedExclusion Criteria:Burn and ICU patients SHOCK TIMEGOALSCall code blue forimminent cardiacor pulmonary failure orneurologic emergencyPrimary team huddle to evaluate for sepsis (RN/Team Leader, LIP, Surgeon when appropriate) Notify Attending Call MET Consider transfer to IMU/ICUDoespatientmeetCRITICAL SEPSIScriteria?!Time Zero Patient flags sepsis red!RapidResponse/METOFF PATHWAYResume routine careNOYES15minActivate Critical Sepsis Pathway Provide supplemental oxygen as needed (oral/nasal ETCO2 for perfusion deficits)Reassess vital signs every 5 minutesOrder appropriate antibiotics POCT: Electrolytes, VBG, lactate, iCa, GlucoseProcalcitoninBlood/urine/CSF cultures!CBC diffCMPCorrectCRPglucoseMagnesiumand calciumPhosphorusConsider Type & ScreenConsider lumbar puncture Appropriate antibiotics for specific populations: HemOnc Suspected Infection Central Line Infections Previously healthy patients with/without intraabdominal source Medically complex patients with/without intraabdominal sourceConsider history of resistant organismsConsider broadening antibiotic coverageSurgery consult for suspected infection requiring sourcecontrol (e.g. skin/soft tissue, intra-abdominal)30min LabsAccess/Initial Fluid Resuscitation Consider PIV in patients with central line ifadditional access is neededAdminister 1st bolus of 20ml/kg normalsaline rapidly over 20 minutes OR LESSConsider 5-10ml/kg boluses if concern forfluid intolerance (cardiac/renaldysfunction)Ongoing ResuscitationAdminister Antimicrobials Consider administration of 2nd and 3rdboluses of 20ml/kg normal saline rapidlyover 20 minutes OR LESS as clinicallyindicatedOrder vasoactive/inotropic drips asindicatedConsider blood products as indicatedBMT patients: consider vasoactive/inotropic drips after 2nd NS bolusConsider PICU consult or calling a codeTransfer to ICURe-Evaluation 60minWell-appearing patients whodo not meet IMU/ICUtransfer criteria, may stay onInpatient unit and are placedon WATCHER list forreassessmentNOMET DebriefDoes patient meetIMU/ICU transfercriteria?YES (ACNW – Use clinical judgement fortransfer to ACLR)Initiate vasoactive/inotropic dripsfor Fluid Refractory ShockEpinephrine for cold shockNorepinephrine for warm shockTitrate drips to resuscitation goalsICU Transfer CriteriaIntermediate Care (IMU) Transfer Criteria (ACNW – use clinical judgement for transfer to ACLR) Resolved hypotension requiring intervention ( 5thpercentile for age)-How to calculate MAP- 1.5 (age in years) 40or if age 13 years MAP 60Need for continuous cardiorespiratory monitoringNeed for 3rd normal saline fluid bolusIMU Admission, Transfer, and Discharge CriteriaE. Rader 4-1659Approved by P&T committee 9/15/20Approved by PCOC 10/6/20 (ACNW – use clinical judgement for transfer to ACLR)Recurrent hypotension despite 40ml/kg fluid resuscitationin the last 12 hours-Fluid resuscitation includes either crystalloid or colloid-Hypotension ( 5th percentile for age)-How to calculate MAP- 1.5 (age in years) 40or if age 13 years MAP 60Clinical situation not appropriate for ongoing fluidresuscitation-Defined as underlying cardiac disease, lung disease,existing fluid overload, impaired renal functionLactate 4 or base excess -4 mmolSustained change in mentation from baseline or perfusion(CR 2 seconds) for at least 15 minutesPatient requires continuous ICU monitoring orICU level respiratory support
MAPs by AgeAge (year)0123456789101112131415161718MAP 5th %tile40424345464849515254555758606163646667MAP 50th %tile55575860616364666769707273757678798182
Medication Dosing for Critical SepsisDosing is for normal renal functionAntipyretics – Choose one Acetaminophen Acetaminophen Acetaminophen IbuprofenAntibiotics: Previously healthy patients Ceftriaxone (bacteremia) Ceftriaxone (meningitis) Ceftriaxone (pneumonia) / Vancomycin – only if suspect MRSA (what dose has patient beenon that gave therapeutic levels?) / Metronidazole – only if suspect intra-abdominal infectionAntibiotics: Medically Complex Patients Cefepime / Vancomycin - only if suspect MRSA (what dose has patient beenon that gave therapeutic levels?) / Metronidazole – only if suspect intra-abdominal infectionOR Meropenem - alternative if cefepime allergy or previous cefepimeresistant infection (ID/ASP approval required) Must re-evaluatetreatment plan at 72 hrs / Vancomycin - only if suspect MRSA (what dose has patient beenon that gave therapeutic levels?)Hypocalcemia Calcium gluconate in dextrose 5%-PIVAdrenal Insufficiency HydrocortisoneHypoglycemia D10 Bolus D25 Bolus D50 BolusIntubation Atropine Ketamine Rocuronium Sugammadex (for NMB reversal)VasoactiveEpinephrine- titrate in small increments based on perfusion (drug ofchoice for inotropy in pediatric shock)Norepinephrine- titrate in small increments to achieve normal MAPMilrinone- no bolus; no titration15 mg/kg, PO, q6 PRN fever20 mg/kg, Rectal, q6 PRN fever15 mg/kg, IV, q6 PRN fever10mg/kg, PO, q6 PRN fever50 mg/kg, IV, q24h50 mg/kg, IV q12h75 mg/kg, IV, q24h15 mg/kg, IV, q6h10 mg/kg, IV, q8h50 mg/kg, IV, q8h15 mg/kg, IV, q6h10 mg/kg, IV, q8h40 mg/kg, IV, q8h15 mg/kg, IV, q6h50 mg/kg, IV, once2 mg/kg, IV, once5 mL/kg, IV, once2 mL/kg, IV, once1 mL/kg, IV, once0.02 mg/kg (max 0.5 mg)2 mg/kg (max 100 mg)1.2 mg/kg (max 100 mg)16 mg/kg0.05-2 mcg/kg/min0.05-2 mcg/kg/min0.3-0.5 mcg/kg/min
Metrics1. Time to first normal saline bolus from positive sepsis red screen2. Time to first antibiotics from positive sepsis red screen3. Blood culture collection time and result4. Huddle completed for patients that screen sepsis red5. Critical sepsis order set usage in ED and Inpatient areas6. Number of critical sepsis/septic shock diagnoses added to problem list
Contributing MembersLawrence Quang, MD – Emergency MedicineJennifer Perry, MD -Emergency MedicineElizabeth Storm, MD – Emergency MedicineSteve Shirm, MD – Emergency MedicineBrittany Slagle, MD – Hospital MedicineChristopher Edwards, MD – Hospital MedicineSanjiv Pasala, MD - Critical Care MedicineMichael Stroud, MD – Critical Care MedicineAmir Mian, MD – Hematology/OncologySuzanne Saccente, MD – Hematology/OncologyAmy Allen, RN – Hematology/Oncology Nursing DirectorLindsey Ward, RN – Hematology/Oncology Clinical EducatorRobyn Abernathy, RN – Hematology/OncologyJulie Pettitt – Hematology/Oncology Pharmacy CoordinatorThad Carter, RN – Emergency Department Nursing DirectorHeather Kreulen, RN – Inpatient Nursing DirectorEimear Melton, RN – Emergency DepartmentJill Jacobs, RN – Emergency Department Patient Care ManagerJessica Crump, RN – Intermediate Care UnitAngela Roberson – Inpatient Clinical Nurse SpecialistValerie Hamric, RN – Intermediate Care Unit Patient Care ManagerHolly Maples, PharmD - Antimicrobial Stewardship DirectorEmily Rader, RN – Clinical Pathways Specialist
References1. Ikram U. Haque, MD, FAAP; Arno L. Zaritsky, MD, FAAP, FCCM (2007). Analysis of theevidence for the lower limit pf systolic and mean arterial pressure in children. Pediatr CritCare Med 2007 Vol. 8, No. 2. 2. B. Ku, MD; F. Balamuth, MD; M.K. Funari, RN; J. Lavelle, MD; C. Jacobstein, MD; D. Davis,MD; J. Fitzgerald, MD J. Gerber, MD; T. Metjian, Pharm D; S. Fesnak, MD; L. Hutchins, CRNP;D. Potts, RN 2018 July. ED Pathway for Evaluation/Treatment of Infants 28 Days of Age andChildren with Suspected Severe Sepsis. Available from: from nt-care-clinical-pathway3. Seattle Children s Hospital, Rutman, L., Robert, J., Beardsley, E., Farris, R., Fenstermacher,S., Leu, M., Marshall, H., Migita, D., O hare, P., Ringer, C., 2016 December. Septic ShockPathway. Available from: athway.pdf
Critical sepsis order set usage in ED and Inpatient areas 6. Number of critical sepsis/septic shock diagnoses added to problem list . Amy Allen, RN - Hematology/Oncology Nursing Director Lindsey Ward, RN - Hematology/Oncology Clinical Educator Robyn Abernathy, RN - Hematology/Oncology . Clinical Pathways Specialist. References 1 .





![EMR Sepsis Information 2016 [Read-Only] - Baxter Regional Health System](/img/42/emr-sepsis-information-2016-78079.jpg)