Transcription
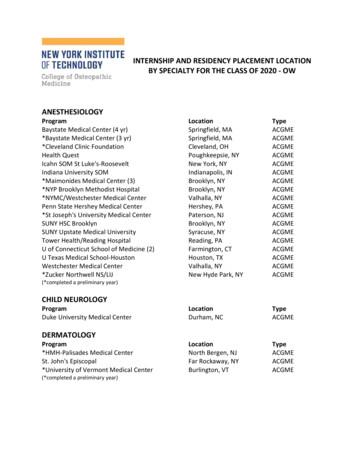
10/20/2014Graduate Medical Education : Focusing on Qualityand Safety in a Clinical Learning EnvironmentDeveloping a Standardized and SustainableResident Sign – Out ProcessBetter Hand Off Safer CareRon Amedee, MDJanice Piazza, MSN, MBAOctober 24, 2014ACGME Institutional Requirements III.B.3. Transitions of care: The Sponsoring Institutionmust:– III.B.3.a) facilitate professional development for corefaculty members and residents/fellows regardingeffective transitions of care; and, (Core)– III.B.3.b) ensure that participating sites engageresidents/fellows in standardized transitions of careconsistent with the setting and type of patient care.(Core)ACGME approved: June 9, 2013; Effective: July 1, 2013 for new sponsoring institutions makingnew applications and July 1, 2014 for existing sponsoring institutions (including both multiple- andsingle- program sponsors)21
10/20/2014CLER Focus AreasDuty HoursFatigueManagementPatient SafetySupervisionTransitionsOf CareHealth CareQualityHealth CareDisparitiesProfessionalismAdapted from ACGMEOMC - CLER Readiness AssessmentCLER site visit (July 23 & 24, 2013)CLER Focus AreasSelf AssessmentGap AnalysisPost CLER site visitcommentsPATIENT SAFETYTrainee reporting of errors, etc.Participation in interprofessional teamsQUALITY IMPROVEMENTSI engages trainees use of data to qualitySI engages trainees use of data to disparitiesSI engages trainees use of data to ID & disparitiesTRANSITIONS IN CARESI standardization/oversight of transitions of careSUPERVISIONSI oversight in line with ACGMEProgram oversight in line with ACGMEDUTY HOURS/FATIGUESI oversight of Duty HoursSI mitigating fatigueSI educates Faculty/TraineesPROFESSIONALISMEducate/Monitor TraineesEducate/Monitor Faculty42
10/20/2014Why a National Initiative Collaboration with some of the best Independent Academic Centers in the CountrySharing of best practices and lessons learnedAccess to National Leaders and Experts inperformance improvement and patient safetyScholarly ActivityNational Initiative IV Needs Statement:Team Charter Lack of standard processbetween : Inpatient settings Hospital Based andPrimary Care Provider to Provider Inpatient to extended /home care Evidenced by:– Patient safety metrics– Readmissions– Patient lost to follow up withunknown outcomesWhat we have committed to doTo evaluate currentpractices, define bestpractices and implementa standardized approachto transitions of care,specifically resident toresident hand-overs.3
10/20/2014DWork Plan Timeline3/15APost InterventionSData CollectionS9/14ImplementationD7/14Project DesignS&Development PublishA Begin next cycle : focus12/14 mentoring and faculty development Minor modifications to forms Repeat Survey and collect feedback Roll out to all programs Implementation in Internal Medicine withResident Champions Pre implementation education / training4/14 Build Tool, Identify metrics and available data sourcesP Assess EMR ( EPIC) functionality hat could supportPre- InterventionData Collection 1/14defined best practices Faculty & House Staff survey to determine currentunderstanding / opinions10/13 Literature Review to identify best practices Gap Analysis: Review tools, practices, policies currently in place toFacilitate transitions of careA Review of What We Have LearnedDuty Hour restrictions increase hand offsEach hand off creates a point of vulnerability in exchange of data, understanding and responsibility betweenphysiciansResearch : breakdown in information transfer creates discontinuity of care and has a negative impact onpatient safetyDelay in test orderingExcessive test orderingMedication errorsIncreased length of stayDecreased efficiency of the individual and the systemFindings to date: Strong adoption and utilization in areas where we have significant focus and buy in fromResident and Faculty Champions. Need continued work with faculty to establish as aprt of routine curriculum,assessment and feedback processesLogic would suggest :More effective hand off systems Decrease in error and adverse eventsStandardized and formalized processes of information transfer are more effective4
10/20/2014The Underlying Model : iPassIIllness Severity -- Stable , “Watcher” , UnstableP Patient Summary - events leading up to admission,hospital/operative course, assessment and planA Action list – to do list , timeline and ownershipS Situation Awareness & Contingency Plan - Know what’s going on;plan for what may happen --- If / ThenS Synthesis by Receiver - receiver summarizes what was heard, asksquestions; restates key actions / to do itemsIpass.study@childrens.harvard.eduGlobal Elements of Effective Handoffs:Unambiguous transfer of Information & Responsibility , Protected Timeand Space , Standardized FormatVerbalComplements Tool Structured Format – High leveloverview Appropriate Pace Closed loop communication Solicit check backs Non-verbalTool/ Written– Electronic Tool thefoundation– Content /Length– Level of training– Knowledge of pts– Length of time onrotation– Opportunity for Discussioncreates shared mentalmodel and facilitates activeparticipation by both parties5
10/20/2014 The Structured Tool - EPICSupplements the verbal handoff– Allows receiver to follow– Provides more comprehensive information Creates efficient information transfer Requires routine updates– High- quality information Don’t copy and paste– Mentor ( Sr resident / supervising faculty ) should edit whennecessary to assure quality– Incorporate time for review and update into daily workflow– Note updates are time stamped and identified6
10/20/2014Resident HandoffPrimary Team Team XRoom Number: 500Date of Birth 1/01/1964Allergies: penicillinAge:60Admit Date: 07/01/2014Sex:MBMI: 52Code Status: FullIllness level ( current clinical status ) : WATCHER (Unstable)Reason for admission: Severe sepsisBrief HPI ( pertinent PMH and diagnosis or differential diagnosis ) :60yo M with past medical history of DM2, CAD, CHF (EF 40%), AF, and COPD who presents with gradually worsening SOB, coughproductive of yellow sputum, increased swelling of lower extremities. Increased use of home O2 (baseline of 2L)Hospital Course( Updated brief assessment by system or problem, significant events)1. Severe Sepsis: Admitted with ¾ SIRS (febrile to 102, HR 110, RR 22) with AMS and AKI. Patient is alert and communicative(sometimes inappropriate) currently.2. COPD exacerbation: Global wheezing on presentation, Obtaining solumedrol 125 Q8H, Duonebs Q4H, Moxifloxacin (day 2). On 50%Venti Mask currently.3. AKI: BUN/creat of 40/2.5 with a baseline of 1.3.Tasks (specific, using if , then statements ):If patient is febrile overnight, please recollect blood cultures, urine cultures, urinalysis.If patient becomes hypotensive (SBP 100), please bolus patient 500cc fluid at a time. Be cautious of respiratory status as patient doeshave a history of CHF.If patient becomes agitated, may give zyprexa 10mg IM.Contingency Plan ( special circumstances anticipated and plan )Plan: Continue steroids/duonebs/antibiotics while weaning down O2 requirements. Notify ICU if acute change in respiratory status orworsening BP unresponsive to IVF.Tips on Observing the Hand off Set the stage and establish objectives– Establish the importance of direct observation– Review the elements that are being observed– Remind participants that this is formative feedbackListen and observeAttempt not to interrupt unless a patient safety issuearisesDebrief– Optimally done immediately or within 24 hours of observation– Best if done in person so that dialogue is possible7
10/20/20148
10/20/20149
10/20/2014Progress to Date : Transitions of care Collaborative project with Alliance of Academic Medical Centers: National Initiative IVFocus on Clinical Learning Environment ( CLE ) component : transitions of careBegan October, 2013 – to date :– Literature review to identify best practices - iPass – Boston Children’s Hospital built onTEAM STEPPS model– Internally identified lack of standardization, lack of mentorship of the process, leadingto redundancy, dropped hand offs, lack of continuity in care - difficult to ascertainspecific data, however moving to an electronic note understanding of the process willimprove over time as we capture relevant information– HIM approved the note type– Frame work and template for form developed in with EPIC builders– Implementation, June 23, 2014– Observation process established August, 2014– Program by Program introduction to process– Form amended based on House Staff feedback: added procedure / delivery date andanticipated discharge date, Advanced Practice Clinicians access established– Ongoing faculty development and plan for increased mentoring of the processChallenges and Barriers Beware of the “Brick Walls” Access and performance within the context of IT securityBuy- in to the standardized approachReaching everyone involved with the same levelof informationParallel, redundant processes that tap sameresourcesIndividualized program roll-out10
10/20/2014Next Steps Ongoing education and facultydevelopmentOngoing faculty engagementCustomizing smart phrasesIncorporate into initial EPICtrainingInterprofessional engagementContinued cycles ofimprovementProcess Application Exercise11
10/20/2014In ConclusionWe welcome you thoughts andfeedbackAny Questions or rences1.2.3.4.5.6.7.8.9.10.Accreditation Council for Graduate Medical Education. Outcome Project. Available at:http://www.acgme.org/outcome/comp/ compCPRL.asp. Accessed November 30, 2009.The Joint Commission. 2009 National Patient Safety Goals Hospital Program. Available at:http://www.jointcommission.org/patientsafety/ nationalpatientsafetygoals/ Accessed on March10, 2010.Gakhar B, Spencer AL (2010) Using Direct Observation, Formal Evaluation, and anInteractive Curriculum to Improve the Sign-Out Practices of Internal Medicine Interns.Academic Medicine 85: 1182–1188Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM (2006) Managing discontinuity inacademic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med1: 257–266.Horwitz LI, Moin T, Green M (2007) Development and Implementation of an Oral Sign-outskills curriculum. J Gen Intern Med. 2007 October; 22(10): 1470–1474.Chu ES, Reid M, Schulz T, Burden M, Mancini D, et al. (2009) A Structured Handoff Programfor Interns. Academic Medicine 84: 347–352Arora V, Johnson J (2006) A Model for Building a Standardized Hand-off Protocol. JointCommission Journal on Quality and Patient Safety 2006 Nov; 32(11): 646-55.Feldman L, Aboumatar H (2007) The “Sign-out Success” workshop: A handoff workshop forphysicians in training. Johns Hopkins Wksp%201.5%20and%202.5 Feldman.pdfI-PASS Program. Children’s Hospital Boston. Ipass.study@childrens.harvard.eduBreaux J, McLendon R, Stedman RB, Amedee RG, Piazza J, Wolterman R. Developing astandardized and sustainable resident sign-out process: an AIAMC National Initiative IV project.Ochsner J. 2014. In press.12
ACGME Institutional Requirements III.B.3. Transitions of care: The Sponsoring Institution must: -III.B.3.a) facilitate professional development for core faculty members and residents/fellows regarding effective transitions of care; and, (Core) -III.B.3.b) ensure that participating sites engage