Transcription
ICU Competencies- PREVIEWDepartment of Physical Medicine and Rehabilitation Johns HopkinsHospital
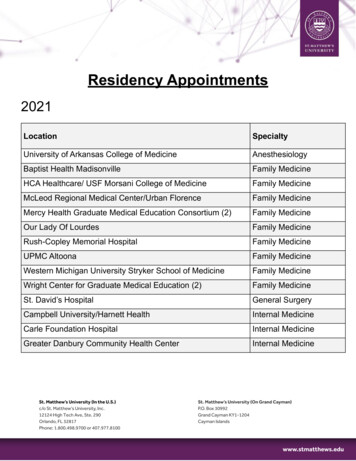
Table of Contents ELModule 1: Intro into Early ICU RehabilitationModule 2: Understanding ICU EquipmentModule 3: Oxygen Delivery SystemsModule 4: Understanding Mechanical VentilationModule 5: ICU Lab ValuesModule 6: ICU DeliriumModule 7: Optimal Assessment and Treatment PlanningASPM
PMELModule 2:Understanding ICU EquipmentASJennifer Zanni, PT, M.S,PTClinical SpecialistJohns Hopkins Hospital
ObjectivesELUpon completion of this module, the learner will beable to:PM Identify common ICU equipment and be able to state theindications and precautions of each Discuss the ability to mobilize patients with various pieces ofICU equipment and any considerations that need to beundertaken Make clinical decisions regarding hemodynamic parametersAS
The Bedside Monitor Monitoring Screen ELPMHeart rateArterial blood pressureCentral Venous PressurePulse oximetryASCheung AM et al. Am J Respir Crit Care Med. Sep 1 2006;174(5):538-544.Fletcher SN et al. Crit Care Med. Apr 2003;31(4):1012-1016.Herridge MS et al. N Engl J Med. Feb 20 2003;348(8):683-693.
EKGLet’s Start with the Basics 2 Types of EKG monitoring Hardwire TelemetryASPMEL
EKG: HardwireEL Patient is attached to monitor by a “hardwire” Allows for 12 lead monitoring (shows all areas of theheart muscle) Primarily used to diagnose ischemia and MI Pros: More thorough monitoring by various leads Cons ASPMLess portable. Not generally connected to central alarmsystem if arrhythmia arises
12 Lead EKGELV1 – right sternal border in the 4thV2 –V3 –V4 –V5 –V6 –intercostal spaceleft sternal border in the 4thintercostal spacemidpoint on a straight line betweenV2 & V45th intercostal space, midclavicularlineanterior axillary line, immediatelyhorizontal to V4midaxillary line, immediately horizontalto V4 & V5ASPM
EKG:Telemetry ELPortableDoes not monitor all 12 leadsSimple detection of rate and rhythm disturbancesUnable to use to diagnose ischemia or MIPros:ASPM More portable and “user-friendly” Attached to central alarm system Cons: Less ability to recognize ischemia/ MI
Blood Pressure MonitoringEL Non-Invasive (NBP)PM Invasive Arterial Blood Pressure (ABP) ASRadial, Femoral, Pedal, Brachial Central Venous Pressure (CVP) Pulmonary Artery (PA) Catheter
Arterial LinesELPMAShttps://www.google.com/search?q google images&hl en&tbm isch&source lnms&sa X&ved 0ahUKEwifq57BuPnTAhWFZiYKHbS8C44Q AUICigB&biw 1920&bih 995&dpr 1#hl en&tbm isch&q arterial line placement&imgrc jEy2sOQ9T5WQVM:
Arterial Blood PressureEL RadialASPMTaken by Jason Seltzer 5/2/17 CCU JHH
Arterial Blood Pressure PedalASPMTaken by Jason Seltzer 3/21/17 SICU JHHEL
Arterial Blood Pressure ELUsed for direct and continuous BP measurementsCan be also used for easy arterial blood drawsTransducer provides electrical read-outHeparinized-saline pressure bag attached toprevent clot formation/occlusion of the lineASPM
ABP:Waveform Left ventricular ejectiongenerates a pressure wavethrough the peripheral arterysystem; this waveform isdisplayed on the bedsidemonitor Each part of the waveformcorresponds to a phase of thecardiac cycleASPMEL
Arterial Blood PressureEL Transducer should be horizontal and close tothe level of the right atrium For every 6 inches the arm is raised above orbelow the heart, BP measurement can changeby 10 mmHg ABP systolic will be slightly higher and ABPdiastolic slightly lower (5-10 mm/Hg) than NBPASPM
Mean Arterial Pressure (MAP)EL Average pressure that pushes blood through the circulatorysystem, although not a true mathematic mean of systolic anddiastolicASPM MAP 1/3 (SBP – DBP) DBP Indication of tissue and organ perfusion Generally considered more important than actual bloodpressures in the ICU setting
Mean Arterial Pressure (MAP)PMEL Normal value: 80-100 mmHg MAP 60 mmHg indicates that perfusion to vitalorgans may be compromised Important to understand MAP goals for eachpatient, especially when on vasopressor orvasodilator medicationsAS
Arterial Blood Pressure Tricks of the trade PMEL MAP may be a better indication of perfusion and medical stability forPT rather than BP. Look at overall trends for clinical decision-making Art line readings will be “positional” with movement. Repositiontransducer if needed. Ensure good waveform throughout treatment.If you are unsure whether reading is accurate, check a NBP When switching to and from portable monitoring, the arterial line willneed to be “zeroed” to ensure accuracyAS
Orthostatic HypotensionTricks of the trade ELPM Drop in systolic BP by 20 mmHg and/or drop in diastolic by 10 mmHg Most accurate diagnosis of orthostatic BP is made when BP ismeasured 3 min after quiet standing (NOT immediately upon standing)AS Not all patients will have associated increased HR (especially if theyare on beta blocker meds)Kaufmann H. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure andmultiple system atrophy. Clin Auton Res 1996. 6125–126
Central Venous Pressure (CVP)EL Direct measurement of the pressure in the right atrium Direct relationship exists between cardiac venousreturn and CVP (i.e. as venous return decreases, CVPalso decreases) Used to assess right heart function and volume status Catheter also provides central IV access for medadministration or blood drawsASPM
Central Venous Pressure(CVP) Line Equipment: transducer, pressurebag and CVP catheterPMEL Single or multiple lumens Common insertion sites: subclavianand jugularAS Catheter tip sits just outside theright atrium in the SVC
Central Venous Pressure MonitoringELPMASkups:/ /Www.&oo .eom/ eard\l'li &1lun.:::isdtBcsour.:t kp.! biw l?ZO&'IIilt. ? &q etbUU Yt)II)US prmW't Jn.oxli.o oq eebUU YOI.ous premue moxli.o ,;- .LU72.6?!1.0.7l!I?. U4.0.0.0.0.1?4.U7 U & . M .O.l.l.64i .l.U.l4S.l .Oj)i10Jdj)i!Oi24klioLjJGH·!INoMJnuG i't)ZeV.JI.,yi]y).t:
MonitoringASPMEL
CVPEL Patient positioning will affect CVP readingsPM CVP will drop when patient is sitting upright due to gravity’saffects on changes in intrathoracic blood volumeAS Normative Values: 0-8 mmHg Low CVP hypovolemia High CVP volume overload or R sided heart failure
CVPTricks of the trade PMEL There is probably little need to monitor CVP continuouslyduring activity. Many times the transducer can bedisconnected for ambulation and mobility. Discuss with thepatient’s nurse If CVP is high, may want to consider modifying treatmentintervention if patient is in heart failure If CVP is low, monitor MAP to ensure adequate perfusionAS
Pulmonary Artery (PA) PressureEL Similar insertion sites as CVP, but catheter isadvanced through the right side of the heart andinto the proximal portion of the pulmonary artery Other name- Swan Ganz CatheterASPM
Pulmonary Artery (PA) PressureMeasures:PMEL Right atrial, ventricular, and pulmonary arterial pressures(including wedge pressure) Cardiac output Calculation of systemic and pulmonary vascular resistance(PVR) Indirect measurement of L-sided heart functionAS
Central Lines- PA CatheterPMELPulmonary Artery (Swan-Ganz) Catheter Used when precise measurements are needed aboutpressures and volume Measures left-sided heart pressure, cardiac output, andfluid statusAS
ASPMELle f t
ELPA Catheter: Normative ValuesPM Right atrium pressure: 0-8 mmHg Right ventricle pressure:15-25 mmHg systolic, 0-8 mmHgdiastolic Pulmonary artery pressure:15-25 mmHg systolic, 6-12 mmHgdiastolic In general, increased values demonstrates volume overloadand/or right sided heart failure. Low values demonstratehypovolemiaAS
PA Catheter: Normative ValuesPulmonary artery wedge pressurePMEL Assesses L-sided heart function Balloon tip inflated in the pulmonary artery to assess left sidedheart function (wedge position) Normal value: 4-12 mmHg Increased wedge pressure: L-sided heart dysfunction andvolume overload Decreased wedge pressure: hypovolemiaAS
PA CathetersTricks of the Trade:PMEL Mobility is contraindicated when the balloon is in the wedgedposition within the pulmonary artery (risk of tearing arterialwall) Ensure that the catheter is positioned in the “pulled back”position in the pulmonary artery and not in the “advanced”position in the pulmonary capillary bedAS
PA CathetersELPMTricks of the Trade: Avoid excessive movement of the lineAS Dislodgement of the PA catheter is a very serious event and maycause patient death Patients can be mobilized with a PA catheter, but opencommunication is needed of all health care providers to ensuresafety
Continuous DialysisPMELCVVHD (Continuous Veno Venous Hemodialysis) Provided over a prolonged period of time as compared to traditionalHD Can be used for HD and/or ultrafiltration Used in ICUs for patients with critical illness whose hemodynamicstatus would not tolerate traditional HD Access is usually subclavian, IJ, or femoralAS
ASPMEL
Continuous DialysisTricks of the trade:ELPM May be difficult to mobilize a patientwith femoral access with CVVHDrunning. Check your hospital policy Otherwise, the patient can bemobilized with care taken to avoidtension on the CVVHD lines. Keep inmind that many CVVHD units cannotbe unplugged to allow for ambulationAS
Intracranial Pressure Monitoring Monitors CSF & brain pressures Normal is 0-15 mmHgAS Can be placed:ELPM Intracranial Pressure (ICP) In lateral ventricles (Intraventricular catheter)- most common Between arachnoid membrane and cortex (Subarachnoid screw or bolt) Epidural space (Epidural sensor)
ICP MonitoringELPM Intracranial Pressure (ICP) Ideal is to keep ICP pressure below 20-25 mmHg Tricks of the TradeAS Ventricular drains should be clamped before changing the patientposition (even the head of the bed), during excessive coughing, andsuctioning Take extreme care with ICP monitoring lines. Have someone managethe head with transfers
Intra Aortic Balloon Pump Used in severe heart failure Left ventricular failureAS Cardiogenic shock ELPM Unstable anginaLine placed through the femoral artery to the aortaInflates during diastole (perfuses coronary arteries)Deflates during systoleIncreased myocardial perfusion and cardiac output
Intra Aortic Balloon PumpASPMEL
Intra Aortic Balloon PumpTricks of the trade:PMEL Patients are usually on bed rest, but still may benefit fromexercises to the uninvolved limbs and focus on pulmonarystatus Limitations on the ability to flex the hip where the line is andhow far the head of the bed can be elevated (usually 30degrees or less for both). Check your hospital policyAS
Extra Corporeal MembraneOxygenation (ECMO)PMEL A type of cardiopulmonary bypass that can be used for days toweeks to allow time for recovery or as a bridge to transplant Patients blood is pumped out through a cannula to aoxygenator that serves the function of the lungsAS Used as a “last chance” effort to save a life
Extra Corporeal MembraneOxygenation (ECMO)ELPMTwo types of systems:Veno-arterial (less common, used mostly in post op cardiac surgerypatients with persistent heart failure) Veno-venous systems (more common, used more for severe respfailure) Complications:ASBleeding due to high amounts of anticoagulation needed Tubing can become kinked Infection Darrah J. Adevnce for Resp Care and Sleep Medicine. Accessed on‐line Feb 27, 2011 at ce‐At‐Life.aspx
ECMOASPMEL
Extra Corporeal MembraneOxygenation (ECMO)Tricks of the trade:PMEL Certain patients on ECMO can be mobilized out of bed andASambulate (if not cannulated through femoral access). Thisrequires a team approach from physicians, nurses, rehab staff,and perfusionist team to ensure safety of the patient andequipment
References ELClini, E & Ambrosino, N. Early physiotherapy in the respiratory intensive care unit.Respiratory Medicine. 2005; Sep;99(9):1096-104Ciesla ND. Lines, Tubes, catheters, and Physiologic Monitoring in the ICU.Cardiopulmonary Physical Therapy Journal. 2000.Darovic, GO. Hemodynamic Monitoring: Invasive and Noninvasive Clinical Application,2nd edition. W.B. Saunders Company; 1995Dean, E. Mobilizing patients in the ICU: Evidence and principles of practice. Acute CareProspectives. 2008. Vol. 17(1).Hillegas EA and Sadowsky HS. Essentials of Cardiopulmonary Physical Therapy, 2ndedition; W.B. Saunders Company; 2001Irwin S and Tecklin JS. Cardiopulmonary Physical Therapy: A Guide to Practice, 4thedition; Mosby; 2004American College of Sports Medicine’s Resource Manual for Guidelines for ExerciseTesting and Prescription, 4th edition; Lippincott Williams and Wilkins; 2001ASPM
Hillegas EA and Sadowsky HS. Essentials of Cardiopulmonary Physical Therapy, 2nd edition; WB. .Saunders Company ;2001 Irwin S andTecklin JS. Cardiopulmonary Physical Therapy: A Guide to Practice, 4th edition; Mosby; 2004 American College of Sports Medicine's Resource Manual for Guidelines for Exercise