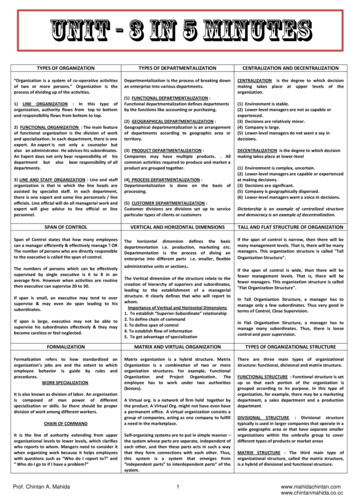
Transcription
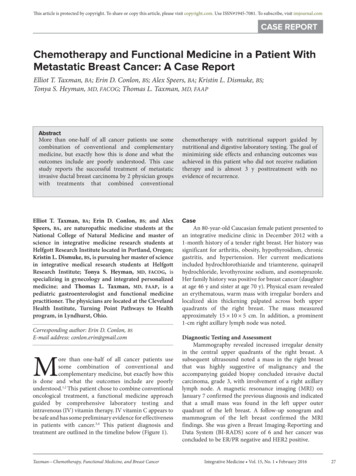
This article is protected by copyright. To share or copy this article, please visit copyright.com. Use ISSN#1945-7081. To subscribe, visit imjournal.comCASE REPORTChemotherapy and Functional Medicine in a Patient WithMetastatic Breast Cancer: A Case ReportElliot T. Taxman, BA; Erin D. Conlon, BS; Alex Speers, BA; Kristin L. Dismuke, BS;Tonya S. Heyman, MD, FACOG; Thomas L. Taxman, MD, FAAPAbstractMore than one-half of all cancer patients use somecombination of conventional and complementarymedicine, but exactly how this is done and what theoutcomes include are poorly understood. This casestudy reports the successful treatment of metastaticinvasive ductal breast carcinoma by 2 physician groupswith treatments that combined conventionalElliot T. Taxman, BA; Erin D. Conlon, BS; and AlexSpeers, BA, are naturopathic medicine students at theNational College of Natural Medicine and master ofscience in integrative medicine research students atHelfgott Research Institute located in Portland, Oregon;Kristin L. Dismuke, BS, is pursuing her master of sciencein integrative medical research students at HelfgottResearch Institute; Tonya S. Heyman, MD, FACOG, isspecializing in gynecology and integrated personalizedmedicine; and Thomas L. Taxman, MD, FAAP, is apediatric gastroenterologist and functional medicinepractitioner. The physicians are located at the ClevelandHealth Institute, Turning Point Pathways to Healthprogram, in Lyndhurst, Ohio.Corresponding author: Erin D. Conlon, BSE-mail address: conlon.erin@gmail.comMore than one-half of all cancer patients usesome combination of conventional andcomplementary medicine, but exactly how thisis done and what the outcomes include are poorlyunderstood.1,2 This patient chose to combine conventionaloncological treatment, a functional medicine approachguided by comprehensive laboratory testing andintravenous (IV) vitamin therapy. IV vitamin C appears tobe safe and has some preliminary evidence for effectivenessin patients with cancer.3,4 This patient diagnosis andtreatment are outlined in the timeline below (Figure 1).Taxman—Chemotherapy, Functional Medicine, and Breast Cancerchemotherapy with nutritional support guided bynutritional and digestive laboratory testing. The goal ofminimizing side effects and enhancing outcomes wasachieved in this patient who did not receive radiationtherapy and is almost 3 y posttreatment with noevidence of recurrence.CaseAn 80-year-old Caucasian female patient presented toan integrative medicine clinic in December 2012 with a1-month history of a tender right breast. Her history wassignificant for arthritis, obesity, hypothyroidism, chronicgastritis, and hypertension. Her current medicationsincluded hydrochlorothiazide and triamterene, quinaprilhydrochloride, levothyroxine sodium, and esomeprazole.Her family history was positive for breast cancer (daughterat age 46 y and sister at age 70 y). Physical exam revealedan erythematous, warm mass with irregular borders andlocalized skin thickening palpated across both upperquadrants of the right breast. The mass measuredapproximately 15 10 5 cm. In addition, a prominent1-cm right axillary lymph node was noted.Diagnostic Testing and AssessmentMammography revealed increased irregular densityin the central upper quadrants of the right breast. Asubsequent ultrasound noted a mass in the right breastthat was highly suggestive of malignancy and theaccompanying guided biopsy concluded invasive ductalcarcinoma, grade 3, with involvement of a right axillarylymph node. A magnetic resonance imaging (MRI) onJanuary 7 confirmed the previous diagnosis and indicatedthat a small mass was found in the left upper outerquadrant of the left breast. A follow-up sonogram andmammogram of the left breast confirmed the MRIfindings. She was given a Breast Imaging-Reporting andData System (BI-RADS) score of 6 and her cancer wasconcluded to be ER/PR negative and HER2 positive.Integrative Medicine Vol. 15, No. 1 February 201627
This article is protected by copyright. To share or copy this article, please visit copyright.com. Use ISSN#1945-7081. To subscribe, visit imjournal.comFigure 1. Timeline of Patient CareIntegrative CareConventional CarePatient presents with 1-mo history Dec 15of tender right breast2012Dec 202013Jan 3IV Vitamin C Treatment Protocol (Riodran IVC Protocol, 2009)25-75 g, 2-3 /wk, totaling 97 infusionsFirst vitamin C infusion (25 g)Dietary and supplementationrecommendation initiatedIVC - Dose increased to 50 gJan 7Jan 10Jan 22Jan 30Jan 29Feb 19IVC - Dose increased to 75 gStress, sleep, and exercise addressedExercise program initiatedFeb 26Mar 12Mar 29Apr 2Apr 23May 14CDSA testingNutrEval testingMay 28Jul 6Sep 24Oct 181-y follow-up post-op;No signs or symptoms of IBCUltrasound and biopsyMRI, diagnosisBone scan, PET-CT pyChemotherapyChemotherapyJun 4Jul 25Completed 97 infusions of IVCSporadic Vitamin CTreatments (IV, oral)Jan 7MammogramMammogram, MRISurgeryFinal does of trastuzumabHypersensitivity reactionDec 172014Aug 5Abbreviations: MRI, magnetic resonance imaging; PET-CT, positron emission tomography-computed tomography;IVC, intravenous cholangiogram; CDSA, comprehensive digestive stool analysis; IBC, inflammatory breast cancer;IV, intravenous.28Integrative Medicine Vol. 15, No. 1 February 2016Taxman—Chemotherapy, Functional Medicine, and Breast Cancer
This article is protected by copyright. To share or copy this article, please visit copyright.com. Use ISSN#1945-7081. To subscribe, visit imjournal.comTable 1. Functional Medicine ProtocolInterventionsMedications Levothyroxine sodium: 130 μg QDEsomeprazole: 40 mg QDQuinapril hydrochloride: 20 mg QDHydrochlorothiazide and triamterene:37.5/25 QDDiet Low glycemic indexDairy freeGluten freeAdequate proteinSupplementation Melatonin: 20 mg QHS Digestive enzymes AC Probiotics: 60 billion CFU BIDo Lactobacillus acidophilus NCFMo Bifidobacterium animalis Bi-07 Medical food shake bid Vitamin D3: 5000 IU QD EPA:DHA: 6000 mg QD Wheat germ extract: 5.5 g QD Oral vitamin C: 18-24 g QD Standardized herbal inflammation reliefsupplementExercise Program 10 min of bicycling bid, working toward30 min/day Qigong classesSleep Program Sleep instructions with log to record sleepSupportRecommendations Individual counseling Group support Part-time caregiver/companionAbbreviations: QD, once per day; QHS, at bedtime; AC, beforemeals; CFU, colony-forming unit; BID, twice per day; NCFM,Lactobacillus acidophilus NCFM; Bi-07, Bifidobacterium animalisBi-07; IU, international units; EPA:DHA, eicosapentaenoicacid:docosahexaenoic acid.Table 2. Oncology ProtocolOncology RecommendationsChemotherapy 6 doses of DCT given 1 every 3 wk Docetaxel: 144 mg, dose 1; 112 mg,doses 2 to 6 Carboplatin: 354 mg, all 6 doses Trastuzumab: 500 mg average (basedon weight)Surgery Mastectomy based on response tochemotherapyRadiation Daily radiation for 6 wk followingsurgeryAbbreviation: DCT, docetaxel, carboplatin, trastuzumab. .Taxman—Chemotherapy, Functional Medicine, and Breast CancerTreatmentThe patient was evaluated at an integratedoncology program that used a functionalmedicine approach guided by comprehensive,panel-based nutritional and digestivelaboratory testing and IV vitamin C. The useof IV vitamin C therapy in cancer remainscontroversial, although some preliminarytrials have shown IV vitamin C to be safe andpotentially effective in improving quality oflife and fatigue in patients with cancer.3,4 Atthis visit, the patient received her first infusionof IV vitamin C (25 g), which was toleratedwell. Biweekly infusions were scheduled forthe next year. The functional medicinetreatment protocol is described in Table 1.On January 22, 2013, the patient receiveda bone scan and positron emission tomographycomputed tomography (PET-CT) scan of thechest, abdomen, and pelvis, all of which werenegative. A medical oncologist recommendedthe treatment plan, outlined in Table 2.Chemotherapy began on January 29, afterwhich the patient reported no symptoms. Thefollowing day, the dosage of IV vitamin C wasincreased to 50 g, which the patient toleratedwell. The patient was compliant with thenutrition program and had decided to stoptaking esomeprazole. A breast exam wasperformed on February 26 and it was noted thattenderness and erythema of the right breast hadremarkably decreased. At this clinic visit, IVvitamin C dosage was increased to 75 g. OnMarch 29, the patient reported fatigue,exacerbated by exercise, as well as alopecia butno other postchemotherapy symptoms werenoted. The patient initiated an exerciseprogram at this time, but adherence was poor.At an April 30 clinic visit, it was notedthat the patient’s weight had dropped to78 kg, and her blood pressure had remainedsteady at 120/60 mm Hg. A decision wasmade at this time to discontinue allhypertension medications. The patient wasexperiencing worsening fatigue and bloodwork was notable for hematocrit of 33%.Six cycles of chemotherapy werecompleted by May 31 and a breast examrevealed no palpable mass. A comprehensivedigestive stool analysis (CDSA) study and aNutritional Evaluation (NutraEval) laboratorytests were ordered, the results of which areshown in Tables 3 and 4. A mammogram onJune 6 showed increased pleomorphiccalcifications posterior to known malignancyand a MRI showed a good overall response toIntegrative Medicine Vol. 15, No. 1 February 201629
This article is protected by copyright. To share or copy this article, please visit copyright.com. Use ISSN#1945-7081. To subscribe, visit imjournal.comTable 3. Genova NutraEval Test ResultsMalabsorption MarkersMarkerValue Reference RangeIndoleacetic acid (IAA) dL 4.2Phenylacetic acid (PAA)0.10 0.12Bacterial Dysbiosis MarkersMarkerValue Reference RangeDihydroxyphenylpropionic acid11.3 5.3(DHPPA)3-Hydroxyphenlacetic acid5.3 8.14-Hydroxyphenlacetic acid19 29Benzoic acid0.23 0.05Hippuric acid603 603Yeast/Fungal Dysbiosis MarkersMarkerValue Reference RangeArabinose3.6 96Citramalic acid3.0 5.8Tartaric acid dL 15Cellular Energy & Mitochondrial MetabolitesCarbohydrate MetabolismMarkerValue Reference RangeLactic acid6.41.9 to 19.8Pyruvic acid2.77 to 32β-OH-Butyric acid (BHBA)2.5 2.8Energy MetabolismMarkerValue Reference RangeCitric acid13940 to 520Cis-Aconitic acid1610 to 36Isocitric acid5922 to 65α-Ketoglutaric acid (AKG)124 to 52Succinic acid dL0.4 to 4.6Malic acid1.4 3.0β-OH-β-Methylglutaric acid (HMG)12 15Fatty Acid MetabolismMarkerValue Reference RangeAdipic acid1.4 2.8Suberic acid1.1 2.1Neurotransmitter MetabolitesMarkerValue Reference RangeVanilmandelic acid4.80.4 to 3.6Homovanillic acid18.21.2 to 5.35-OH-indoleacetic acid20.43.8 to 12.13-Methyl-4-OH-phenyglycol0.150.02 to 0.22Kynurenic acid4.8 7.1Quinolinic acid4.8 9.1Kynurenic/Quinolinic ratio1.00 0.44Vitamin MarkersMarkerValue Reference Rangeα-Ketoadipic acid0.9 1.7α-Ketoisovaleric acid1.04 0.97α-Ketoisocaproic acid0.97 0.89α-Keto-β-Methylvaleric acid3.1 2.1Formiminoglutamic acid (FIGIu)0.7 1.5Glutaric acid0.43 0.51Isovalerylglycine2.0 3.7Methylmalonic acid1.2 1.9Xanthurenic acid0.63 0.963-Hydroxypropionic acid135 to 223-Hydroxyisovaleric acid12 2930Integrative Medicine Vol. 15, No. 1 February 2016Toxin & Detoxification MarkersMarkerValue Reference Rangeα-Ketophenylacetic acid0.42 0.46(from Styrene)α-Hydroxyisobutyric acid13.6 6.7(from MTBE)Orotic acid0.770.33 to 1.01Pyroglutamic acid3116 to 34Tyrosine MetabolismMarkerValue Reference RangeHomogentisic acid67 192-Hydroxyphenylacetic acid0.68 0.76Creatinine ConcentrationMarkerValue Reference RangeCreatinine3.73.1 to 19.5 mmol/LNutritionally Essential Amino AcidsMarkerValue Reference RangeArginine2210 to 64Histidine302296 to 1136Isoleucine3524 to 58Leucine5530 to 87Lysine4545 to 286Methionine9330 to 82Phenylalanine4826 to 71Taurine25968 to 538Threonine13665 to 252Tryptophan8728 to 111Valine4023 to 61Nonessential Protein Amino AcidsMarkerValue Reference RangeAlanine195146 to 486Asparagine10349 to 182Aspartic acid4435 to 86Cysteine6021 to 78Cystine5026 to 78γ-Aminobutyric acid14 31Glutamic acid255 to 21Glutamine219172 to 570Proline52 to 18Tyrosine8233 to 124Intermediary MetabolitesB Vitamin MarkersMarkerValue Reference Rangeα-Aminoadipic acid2211 to 73309 to 49α-Amino-N-butyric acidβ-Aminoisobutyric acid5622 to 192Cystathionine dL6 to 333-Methylhistidine252131 to 318Urea Cycle MarkersMarkerValue Reference Range14.0 to 19.0Ammonia41.8mmol/g creatinineCitrulline6112 to 45Ornithine114 to 21168 to 465Urea371mmol/g creatinineTaxman—Chemotherapy, Functional Medicine, and Breast Cancer
This article is protected by copyright. To share or copy this article, please visit copyright.com. Use ISSN#1945-7081. To subscribe, visit imjournal.comTable 3. (continued)Glycine/Serine MetabolitesMarkerValue Reference RangeGlycine389639 to 3306Serine296187 to 568Ethanolamine198208 to 514Phosphoethanolamine3118 to 70Phosphoserine4628 to 63Sarcosine34 48Dietary Peptide Related MarkersMarkerValue Reference RangeAnserine (dipeptide) dL7 to 126Carnosine (dipeptide)2810 to 1041-Methylhistidine53492 to 1046β-Alanine23 21Markers for Urine RepresentativenessMarkerValue Reference RangeGlutamine/Glutamate9 10Ammonia41.814 to 49 mmol/gcreatineArginine/Ornithine2.0 1.1Urine representativeness index95 to 10Omega 3 Fatty AcidsMarkerValue Reference Rangeα-Linolenic (ALA) 18:30.12 0.09 wt %Eicosapentaenoic (EPA) 20:53.07 0.16 wt %Docosapentaenoic (DPA) 22:53.24 1.14 wt %Docosahexaenoic (DHA) 22:65.9 2.10 wt %% Omega 3s12.3 3.8Omega 6 Fatty AcidsMarkerValue Reference RangeLinoleic (LA) 18:210.110.5 to 16.9 wt %γ-Linolenic (GLA) 18:30.050.03 to 0.13 wt %Dihomo-γ-linolenic (DGLA) 20:31.18 1.19 wt %Arachidonic (AA) 20:41715 to 21 wt %Docosatetraenoic (DTA) 22:41.411.50 to 4.20 wt %Eicosadienoic 20:20.29 0.26 wt %% Omega 6s29.630.5 to 39.7Omega 9 Fatty AcidsMarkerValue Reference RangeOleic 18:11110 to 13 wt %Nervonic 24:14.02.1 to 3.5 wt %% Omega 9s14.913.3 to 16.6Saturated Fatty AcidsMarkerValue Reference RangePalmitic C16:02018 to 23 wt %Stearic C18:01814 to 17 wt %Arachidic C20:00.290.22 to 0.35 wt %Behenic C22:00.950.92 to 1.68 wt %Tricosanoic C23:00.150.12 to 0.18 wt %Lignoceric C24:02.02.1 to 3.8 wt %Pentadecanoic C15:00.090.07 to 0.15 wt %Margaric C17:00.340.22 to 0.37 wt %% Saturated Fats41.439.8 to 43.6Taxman—Chemotherapy, Functional Medicine, and Breast CancerMonounsaturated FatsOmega 7 FatsMarkerValue Reference RangePalmitoleic 16:10.24 0.64 wt %Vaccenic 18:11.16 1.13 wt %5-OH-indoleacetic acid20.43.8 to 12.1Trans FatMarkerValue Reference RangeElaidic 18:10.38 0.59 wt %Delta - 6 Desaturase ActivityMarkerValue Reference RangeLinoleic/DGLA 18:2/20:38.66.0 to 12.3Cardiovascular RiskMarkerValue Reference RangeOmega 6s/Omega 3s2.43.4 to 10.7AA/EPA 20:4/20:5512 to 125Omega 3 index9.0 4.0Oxidative Stress MarkersGlutathione (whole blood)675 669 μmol/L 10.0 μmol/gLipid peroxides (urine)8.2creatine8-OHdG (urine)23 15 μg/g creatineCoenzymes Q10, ubiquinone (plasma) 1.10 0.43 to 1.49 μg/mLElemental Markers (RBCs)Nutrient ElementsMarkerValue Reference RangeCopper0.642 0.466 to 0.721 μg/gMagnesium46.130.1 to 56.5 μg/gManganese0.041 0.007 to 0.038 μg/gPotassium34602220 to 3626 μg/gSelenium0.730.25 to 0.76 μg/gZinc13.47.8 to 13.1 μg/gToxic ElementsMarkerValue Reference RangeLead0.013 0.048 μg/gMercury dL 0.0039 μg/gAntimony0.002 0.002 μg/gArsenic0.032 0.071 μg/gCadmium0.001 0.001 μg/gTin0.0010 0.0009 μg/g% Saturated fats41.439.8 to 43.6Integrative Medicine Vol. 15, No. 1 February 201631
This article is protected by copyright. To share or copy this article, please visit copyright.com. Use ISSN#1945-7081. To subscribe, visit imjournal.comTable 4. CDSA Test ResultsDigestion/AbsorptionMarkerValuePancreatic elastase 1145Putrefactive SCFAs (total)3.1Gut ImmunologyMarkerValueEosinophil protein X1.1Calprotectin 16MetabolicMarkerValueBeneficial SCFAs econdary Bile AcidsMarkerValueLithocholic acid (LCA)2.30Deoxycholic acid (DCA)4.04LCA/DCA ratio0.57ParasitologyCryptosporidiumGiardia lambliaEntamoebahistolytica/disparReference Range 201 μg/g1.3 to 8.6 μmol/gReference Range 7.0 μg/g 50 μg/gReference Range 13.6 μmol/g 2.5 μmol/g6.1 to 7.9337 to 4433 U/gReference Range0.65 to 5.21 mg/g0.67 to 6.76 mg/g0.37 to sscheduledforJuly 25. One month before surgery, blood pressure wasstable at 130/70 mm Hg without medication and hematocritwas 27.8% and stable.On July 25, a right modified radical mastectomy wasperformed with sentinel lymph node excision andcomplete axillary lymph node dissection. In addition, aleft simple mastectomy was performed. The pathologyreport showed no residual carcinoma in the right breastand skin. Sentinel nodes 1 and 2 were negative formetastatic carcinoma, along with 13 axillary lymphnodes. Fibrocystic changes with microcalcifications anda focal carcinoma in situ were found in the left breast.Postsurgery, the patient refused radiation therapy butcontinued complying with her functional medicine planand planned to continue her vitamin C infusions twiceper week to complete 1 year of therapy.The patient received her last dose of trastuzumab onSeptember 24. Two months following surgery on September30, the patient’s hematocrit had returned to baseline levelsat 41%. During this time, the patient’s blood pressure hadbegun to rise and her cardiologist placed her on a newhypertension medication. After beginning this medication,the patient experienced a hypersensitivity reaction onOctober 18 characterized by dermatographism, urticaria,and severely elevated blood pressure. The reaction wastreated with methylprednisolone, diphenhydramine, andIV fluids. The patient followed up with cardiology to followpossible cardiotoxicity. At the patient’s next functionalmedicine visit on October 31, it was decided to decrease herIV vitamin C infusions to 50 g.32Integrative Medicine Vol. 15, No. 1 February 2016The patient remained off of hypertension medicationsand her blood pressure remained stable at 140/70 mm Hgthrough the end of the year. The year-long IV vitamin Cprogram, consisting of twice-weekly infusions, wascompleted on December 17 and totaled 97 infusions. Thepatient continued to improve and began traveling again. Ata follow-up visit on January 21, 2014, blood work wasnormal and the patient reported doing very well. A 1-yearpost-op clinic visit on August 5, 2014, showed a normalcomplete blood count (CBC) and comprehensive metabolicpanel (CMP) with no signs or symptoms of breast cancer.This case is unique because of the integrated approachguided in part by nutritional and digestive evaluation(NutrEval) from a Clinical Laboratory ImprovementAmendments (CLIA)-certified laboratory testing company(Genova Diagnostics, Asheville, NC, USA) that was used inthe management of this patient with advanced ductal breastcarcinoma.5 Because this is a case report from the real worldpractice of medicine, it is not possible to determine theresponsibility of the treatments in this patient’s success inachieving remission. Nevertheless, the patient survived hercancer with minimal side effects during treatment and is nowin her third year of remission. This case study highlights thepotential benefits of integrative therapy in the comanagementof patients with invasive ductal carcinoma of the breast.Patient Perspective“I was worried about the side effects of chemotherapy but Inever had to have a blood transfusion, I only had diarrheaonce, and no nausea and vomiting. I had a little bit of fatiguebut stayed active and did not have to change my lifestylevery much. I was able to be with my friends and family, andto taste and eat food while I was being treated. I thoughtthat I looked better than the other chemotherapy patients Isaw when I went to get treatments. They all looked so sickand so much older than me! The worst thing was losingmy hair! I knew that the medications had a long list of sideeffects and at the beginning I did not understand that theycould be minimized, but they were! I had chemotherapyand surgery but never had any radiation. Two years later, Iam still cancer free and feel great. I may be healthier nowthan I was before my diagnosis and treatment.”Author Disclosure StatementNo financial support was provided for this paper. And the authors have no conflictsof interest to declare.References1. Garland SN, Valentine D, Desai K, Li S, Langer C, Evans T, Mao JJ.Complementary and alternative medicine use and benefit finding amongcancer patients. J Alt Complement Med. 2013;19(11):876-881.2. Huebner J, Muenstedt K, Prott, FJ, et al. Online survey of patients with breast canceron complementary and alternative medicine. Breast Care. 2014;9(1):60-63.3. Carr AC, Vissers MCM, Cook JS. the effect of intravenous vitamin c oncancer- and chemotherapy-related fatigue and quality of life. Front Oncol.2014;4:283.4. Sebastian PJ, Sun AY, Chen C, Espey MG, Drisko J, Levine M. Vitamin C:Intravenous use by complementary and alternative medicine practitionersand adverse effects. PLoS ONE. 2010;5(7): e11414.5. Genova Diagnostics. About us. https://www.gdx.net/about. AccessedNovember 15, 2015.Taxman—Chemotherapy, Functional Medicine, and Breast Cancer
Taxman—Chemotherapy, Functional Medicine, and Breast Cancer Integrative Medicine Vol. 15, No. 1 February 2016 27 Elliot T. Taxman, BA; Erin D. Conlon, BS; and Alex Speers, BA, are naturopathic medicine students at the National College of Natural Medicine and master of science in integrative medicine research students at