Transcription
BANGLADESHWHAT’S INYOUR NCDPOLICYANALYSING THE STRENGTH OFDIET-RELATED NCD POLICIES INBANGLADESHDivision of Health Systems and PopulationsStudies, icddr,b, BangladeshCentre for Gender and Global HealthUniversity College London, UK
The strength of national diet-related policies should match the severity of the burden of noncommunicable diseases (NCDs) in Bangladesh, and guide government action focused on themost critical dietary drivers and population groups at risk.Yet, while Bangladesh has recognised the importance of addressing NCDs, there has been littlerigorous analysis of country-level policies to tackle NCDs associated with unhealthy diets.This brief presents an assessment of national policies and strategies to promote healthy dietsand offers evidence-informed recommendations for shaping comprehensive, effective andequitable diet-related NCD policies.The research presented has been conducted as part of a six-country study comparing national NCDpolicies to global recommendations, and evaluating the extent to which policies include effective andequitable attributes to improve population health. Study countries included Afghanistan, Bangladesh,Nepal, Pakistan, Tunisia and Vietnam.Research in Bangladesh was led by a team based at the Division of Health Systems and PopulationsStudies Division, icddr,b, in partnership with the Centre for Gender and Global Health, UniversityCollege London.The study was funded by the UK’s Medical Research Council under grant number MR/P025188/1 andfrom the European Union under grant agreement No 1260.Date of publication: 2019
PAGE 1NCDS IN BANGLADESHWhile Bangladesh continues to address a high burden of communicable diseases, it faces a growingepidemic of non-communicable diseases (NCDs). In 2017, 67% of deaths were due to NCDs. Onequarter of all men and one-fifth of women are at risk of premature death from NCDs.Rapid economic growth has lifted Bangladesh out of the UN list of least developed countries. Yeteconomic progress has not been shared equitably and is contributing to stark and widening incomedisparity and, consequently, a dietary differential. Both the affluent, who consume increasing amountsof processed food, and impoverished populations, who are deprived of adequate nutritious food, areexposed to the risks of non-communicable diseases.FIG.1NCDS ACCOUNT FOR FIVE OF THE TOP TEN CAUSES OF PREMATUREDEATH IN BANGLADESH – AND ARE ON THE RISETop 10 causes of years of life lost (YLLs) in 2017 and percent change, 2007-2017, all ages, numberFIG.2UNHEALTHY DIET IS AMONG THE MOST SIGNIFICANT – ANDFASTEST GROWING – DETERMINANTS OF NCDSTop 10 risks contributing to DALYs in 2017 and percent change, 2007-2017, all ages, number2017 ranking1234567Metabolic risks8Environmental/occupational risks9Behavioral risks101111 Determinant related to unhealthy dietData for Figures 1 and 2 from Institute of Health Metrics and Evaluation, 2019: http://www.healthdata.org/bangladesh
PAGE 2THE GLOBALRESPONSE TO NCDSMany interventions for the prevention andcontrol of NCDs exist. Given the resourceconstraints faced by all countries and their needto prioritise the most effective interventions, theWorld Health Organization (WHO) hasidentified a set of evidence-based “Best Buy”interventions that are not only highly costeffective but also feasible and are recommendedfor implementation in all countries.Several of the Best Buys are explicitly aimed ataddressing unhealthy diets.1 These interventionsare designed to mainly address the structuraldrivers and commercial determinants of diet, anapproach likely to yield greater benefits at thepopulation level compared to individuallyfocused interventions.2,3NCDs: On the global agenda at lastWhile the burden of NCDs has beenhistorically neglected by the global healthcommunity, prioritisation and action toprevent and address NCDs is expanding.The first UN General Assembly High-LevelMeeting on NCDs in 2011 marked a criticalturning point in mobilising politicalattention and policy action at national andglobal levels, as did the inclusion of anNCDs-related target in the SustainableDevelopment Goals (3.4, to reducepremature mortality from NCDs by onethird by 2030).2%OF ALL GLOBALHEALTH FINANCING ISALLOCATED TO NCDSACTION IN BANGLADESHBangladesh has acknowledged NCDs as asignificant issue and set out its response in arange of policy documents, including the 7thFive-Year Plan, the Health, Nutrition andPopulation Strategic Plan, and the MultisectoralAction Plan for Prevention and Control ofNoncommunicable Diseases 2018-2025. TheMultisectoral Action Plan promotes a health-inall-policies approach, with an emphasis onprevention – including through strengtheningpreventive measures in primary health care,tobacco/alcohol control regulation andencouraging healthy diets. Strong legislativemeasures to reduce consumption of salt, sugarand saturated fatty acid or trans-fats, however,are lacking.Bangladesh Policy Analysis: Our researchDuring 2017-2019, we undertook an in-depthanalysis of the Government’s policies forcontrolling diet-related NCDs, and comparednational responses to global recommendationsfor all countries. The purpose of the study was toidentify where and how policy could bestrengthened to more effectively address thegrowing burden of NCDs in the country.
PAGE 3P O L I C Y D O C U M E N T A N A LY S I S : O U R Q U E S T I O N STHREE DIMENSIONS OF A ROBUST POLICY FRAMEWORK TOADDRESS AND PREVENT NCDS1233C O M P R E H E N S I V E : ARE BANGLADESH’S NCD POLICIESCONSISTENT WITH GLOBAL RECOMMENDATIONS? [TABLE 1]E F F E C T I V E : DO BANGLADESH’S NCD POLICIES HAVEADEQUATE AUTHORITY, ACCOUNTABILITY MECHANISMS ANDBUDGET? [TABLE 1 & FIGURE 3]E Q U I TA B L E : DO BANGLADESH’S NCD POLICIES PROMOTEEQUITY AND HUMAN-RIGHTS BASED APPROACHES? [FIGURE 4]OUR METHODSWe conducted an in-depth policy content analysisanalysis framework to explore issues of actorfollowed by stakeholder interviews. The contentof policies inside and outside the health sectorpower, ideas (how the issue is perceived andportrayed), context, and policy characteristicswere reviewed to determine: (1) whether theywere consistent with WHO Best Buys; (2) how(including severity of the problem and theavailability of effective interventions), tomuch authority the policy has (e.g. whether it isnational law or a sectoral strategic plan); (3)understand: (1) why some of the Best Buys havesucceeded in gaining political and policy attention;systems of accountability; (4) any associatedbudgetary line items; (5) the extent of attention(2) why other Best Buys are absent from thecurrent policy response; (3) what explains policypaid to issues of equity (including gender) andhuman rights. We synthesised these findings intocontent and its characteristics (particularly inrelation to questions of authority, accountability,rights-based approaches, etc); and (4) what ita “policy cube” to graphically present keyfeatures of the policy responses to combat dietrelated NCDs (see page 6).In-depth interviews were conducted withstakeholders purposely selected from a variety oforganisations and sectors. We used a policywould take for neglected/absent Best Buys to behigher up the current policy agenda.The study received approval from the ethicsboards of icddr,b, Bangladesh and UniversityCollege London, UK.
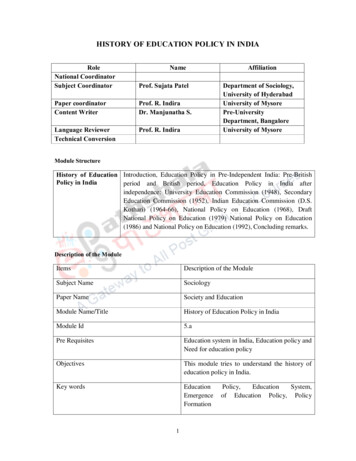
OUR FINDINGSTABLE 1. BANGLADESH’S NCD-RELATED HEALTH POLICIES:COMPREHENSIVENESS OF BEST BUYS AND POLICY EFFECTIVENESSBest Buys: Cost-effective interventionsPresent?AuthorityAccountabilityBudget Reduce salt intake through reformulation of food products and settarget levels for salt in foods and meals Goal to decrease salt consumption Reformulation of food products to decrease salt Set target salt level in foodsxxxx 30% reduction in salt consumption Reduce salt intake through the establishment of a supportiveenvironment in public institutionsReduce salt intake through a behaviour change communication andmass media campaign Mass media campaign to reduce salt intake Behaviour change communication on salt xxxxReduce salt intake through front-of-pack labellingEffective interventions Cost effectiveness of / 100 per disabilityadjusted life year averted in low & middle-income countriesEliminate industrial trans-fats through the development oflegislation to ban their use in the food chain Goal to eliminate industrial trans-fatsxxxx Legislation to ban use of trans-fats in food chainxxxx Reduce sugar consumption through effective taxation on sugarsweetened beverages Goal to reduce sugar intake Taxation on sugar-sweetened beverages Subsidies to increase uptake of fruits and vegetablesxxxxReplace trans-fats and saturated fats with unsaturated fats throughreformulation, labelling, fiscal or agricultural policies Limit portion and package size to reduce energy intake and the riskof overweight/obesityxxxxImplement nutrition education and counselling to increase intake offruits and vegetables Implement nutrition labelling to reduce total energy intake (kcal),sugars, sodium and fats Implement mass media campaign on healthy diets Promote exclusive breastfeeding for first 6 months of life Other recommended interventions
PAGE 5TABLE 1. KEYAuthorityAccountability High authority Abides by key principles of accountability4 Budget line item assigned to policy Medium authority Low authorityA national lead/implementing agency isnamed and is assigned responsibility forreporting in the public domain Budget line item planned but noevidence for line item identified No mechanism for accountability found No budget line item identifiedBudgetsub-componentPOLICIES WITH BEST BUY INTERVENTIONSMultisectoral Action Plan for Prevention and Control of Noncommunicable Diseases (2018-2025), 2018, Ministry ofHealth & Family Welfare, Government of People’s Republic of Bangladesh.Breast-Milk Substitutes (BMS) Act, 2013, Government of People’s Republic of Bangladesh.FIG. 3HIERARCHY OF POLICY AUTHORITY IN BANGLADESHThe relative level of authority of policy documents has beencategorised, which can indicate the likelihood that bureaucrats,industry and society will act on INESTANDARDOPERATIONAL PLANSTRATEGYFIG. 4HEALTH AND RIGHTS IN BANGLADESH POLICYRights-based policies can strengthen countries’ efforts to address the determinants of NCDs. A rights-basedapproach has been central to progress in the AIDS response, both in ensuring that individuals are protectedagainst discrimination and committing the State to take positive actions. We find however, that human rightslanguage and concepts are largely absent from NCD policies.5NCD POLICY“People are protected by law againstNCD related risk factors.”Strategic Plan for Surveillance andPrevention of NCDs 2011-2015“Policies and programmes shouldaddress the social determinants andneeds of poor and marginalizedcommunities, and reduce health andsocial inequities.”Multisectoral Action Plan for Prevention andControl of NCDs 2018-2025HIV POLICY“Human rights approaches reduce vulnerabilities to HIV,and include rights such as access to health care,information, confidentiality and gender equity.”National Strategic Plan For HIV and AIDS Response 2018-2022“The necessity of enabling environments to addresshuman rights violations and gender inequality wasIdentified partnership with the Human RightsCommission was deemed suitable.”National Strategic Plan For HIV and AIDS Response 2011-2015“By the year 2010, people at risk of HIV infection willhave access to the means of protection in ways thatrespect their human rights and dignity and will beempowered to protect themselves and others.”National Strategic Plan For HIV and AIDS Response 2004-2010
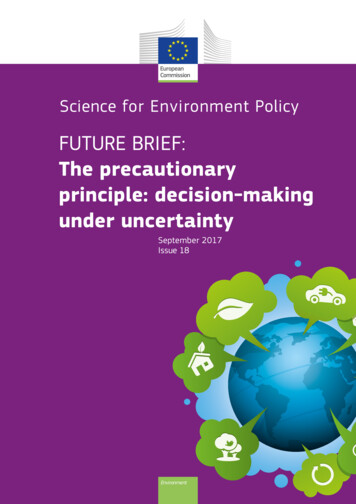
PAGE 6BRINGING IT ALL TOGETHER:THE POLICY CUBEThe “Policy Cube,” brings together the three axesof our policy content review: 1) dietary policyEffectiveness. Mechanisms to ensure effectiveimplementation require considerable action. Whilecomprehensiveness, or the extent to which WHOBest Buys are reflected in national policydocuments; 2) the effectiveness of a policy’sstrategies are comprehensive, translating wordsinto action suffers from a lack of politicalcommitment and authority. NCD action planscarry the lowest level of authority. The soleimplementation and enforcement mechanisms,such as the level of authority of the policy,whether it has an associated budget, and whethersystems of accountability are specified, and; 3) the2exception is the Breast Milk Substitutes Act 2013which has strong authority in controlling theextent to which the policy documents are orientedtowards principles of equity, gender and humanmarketing of breastmilk substitutes and babyfoods. Further, while a National MultisectoralNCD Coordination Committee exists, theirrights. A full cube would represent a robust policyframework for the prevention and control ofauthoritative power to incorporate WHO BestBuys in policies and laws is limited.NCDs.Equity. While the Multisectoral Action Plan doesComprehensiveness. With 12 of the 18 Best Buys,Bangladesh’s policies are fairly comprehensive ofacknowledge the increased vulnerability ofmarginalised communities to NCDs and the roleglobal recommendations. The country is workingtowards reducing salt intake by 30% by 2025, andwhile there is not yet a clear target for reducingsugar consumption, policies and taxes have beenof social inequities in driving differential healthoutcomes, it lacks any specific languageconcerning human rights or gender equality anddoes not identify key populations at higher risk ofintroduced to encourage reduction.NCDs.FIG. 5POLICY CUBE BANGLADESH: THREE DIMENSIONS OF ASSESSING NCDPOLICY FRAMEWORKSEffectiveness (authority,accountability, budget):NEEDS STRONG ATTENTIONComprehensiveness ofbest buy measures:Equity, gender and rightsorientation:NEEDS STRONG ATTENTIONPERFORMANCE OFPOLICY FRAMEWORKADEQUATE
PAGE 7S TA K E H O L D E R S W E I G H I NINTERVIEWS WITH STAKEHOLDERS ON THEMAJOR IMPEDIMENTS TO PROGRESS INADVANCING THE NCD AGENDA: KEY FINDINGSPOWERAbsence ofcoordination betweenMinistry of Health andother ministriesPOWERLeadership and civilsociety mobilisationshould play primaryroles in policy making“I don’t think that the Ministry of Health is coordinating well with otherministries, including finance, to tackle NCDs. All problems related tohealth should be addressed by the MoH. The Ministry of Finance willprovide support if they want to increase taxes on sugar.KII 18, Ministry of Finance official“Currently, civil society in Bangladesh does not play a very important roleto promote healthy diets to tackle the burden of NCDs. In the past, CABplayed a key role in the anti-tobacco campaign. Civil societyorganisations, especially CAB, can work as a pressure group toimplement laws or act on taxation of sugar.KII 10, Official from UN agencyIDEASLow understanding oflinks betweenunhealthy diet andNCDsCHARACTERISTICSPerception thattaxing sugary drinkswill disproportionatelyharm poor people“Bangladeshi farmers sweat a lot during summer. They need to take moresalt. People also need sugar for energy. Where is the evidence that if youeat more sugar you will get diabetes? We also do not have evidence inour country about the relationship between salt intake and hypertension.KII 15, Government official“Imposing tax on sugar-sweetened beverages may not eliminate theproblem. Rather a price hike will affect poor people. They will be deprivedof access to nutritious food. Sugar-sweetened beverages are still a sourceof energy. On the other hand, taxation will not convince more affluentpeople to buy less and consume less.KII 5, ResearcherOPPOSITIONStrong oppositionfrom the private foodindustry to taxation onsugarCULTURAL NORMSSalt and sugarconsidered not only asfood, but an integralpart of culture“Private industries are powerful and they can influence the policy makingprocess. Many politicians are businessmen and owners of industries,which will influence the process of policy prioritisation.“We like to eat sweets. Salt and taste are also related. As representativesof government, we need to think carefully about how to change culturalnorms in Bangladesh. If the government imposes a tax on sugar, the pricewill increase and people will not be happy with the government.Awareness sessions would be good options to change people’s behaviour.KII 15, Government officialKII 23, Government official
PAGE 8R E C O M M E N DAT I O N SThe following recommendations arise from our policy analysis and stakeholder interviews. Theyshould be considered as a strategic package of elements that are mutually reinforcing andinterdependent, and require the engagement of a range of identified stakeholders.1.Inform relevant stakeholders of dietary Best Buys. The Ministry of Health andFamily Welfare (MoHFW) should use biannual meetings of the NationalMultisectoral NCD Coordination Committee (NMNCC) to inform members of thecommittee on the burden of diet-related NCDs, determinants, effective interventionsand the potential cost of inaction.2.Increase frequency of meetings among stakeholders. The MoHFW should conveneregular meetings of the NMNCC members at a more technical level to discuss theprogress and challenges of each ministry in relation to their responsibilities inimplementing the multisectoral action plan.3.Disseminate the evidence base on the causes, burden and costs of NCDs globallyand in Bangladesh. The MoHFW should promote and support the development ofnational capacity for identifying appropriate evidence on the causes, burden andcosts of NCDs.4.Increase involvement of coordinated civil society in the NCD response. MoHFWand development partners should strengthen and adequately resource a coalition ofcivil society organisations (CSOs) that have the capacity and interest to promoteNCD prevention and control. Existing powerful and nationally present CSOs shouldbe encouraged to engage with NCD policy activities.5.Shift cultural norms and food industry behavior around consumption of salt andsugar. Encourage the NMNCC to adopt a twin-track strategy to shift cultural norms.Use multi- and professional mass-media communications to promote changes indietary choices and behaviour, backed with legislative mechanisms to shiftindustry’s behaviours, e.g. banning advertising to children, ensuring front-of-packlabelling, etc.6.Strengthen regulatory capacity to monitor and enforce healthy food standards.Encourage NMNCC to pursue legislation to strengthen the ability of the BangladeshStandards and Testing Institution and Bangladesh Food Safety Authority to set andenforce standards relevant to the Best Buys, e.g. elimination of trans-fats inprocessed food.7.Include time-bound targets in NCD policies. To convey a sense of urgency, monitorprogress and ensure accountability, encourage NMNCC to ensure baselines andtargets become the norm in dietary NCD plans and policies.8.Encourage consideration of a rights-based approach to NCD policy formulation.The NMNCC should be encouraged by an advocacy coalition, comprised ofinterested public health practitioners, academics and civil society, to consider thebenefits of including rights, gender and equity concepts, language and targets infuture diet-related NCD policies.
REFERENCES1World Health Organization. ‘Best Buys’ and Other Recommended Interventions for the Prevention and Control ofNoncommunicable Diseases. https://www.who.int/ncds/management/WHO Appendix BestBuys.pdf2Roberts, S, Pilard, L, Chen, J, Hirst, J, Rutter, H, Greenhalgh, T. (2019). Efficacy of population-wide diabetes andobesity prevention programs: An overview of systematic reviews on proximal, intermediate, and distal outcomesand a meta-analysis of impact on BMI. Obesity Reviews; 1– 17.3Stuckler, D., & Nestle, M. (2012). Big Food, Food Systems, and Global Health. PLoS Medicine; 9(6), E1001242.4Key principles of accountability, namely: i) a national lead/implementing agency is named and is assignedresponsibility for reporting in the public domain; ii) a mechanism for independent monitoring of progress onimplementation is described; and iii) remedial actions/sanctions/fines are outlined if implementation progressdoes not occur. From: Williams C, Hunt P. (2017). Neglecting human rights: accountability, data and SustainableDevelopment Goal 3, The International Journal of Human Rights; DOI:10.1080/13642987.2017.1348706.5Buse K, Aftab W, Akhter S, et al. Time to clarify State obligations and accountability on NCDs with human rightsinstruments. BMJ Global Health 2019;0:e002155. doi:10.1136/bmjgh-2019-002155
For further information, please contact:Dr. Sadika Akhtersadika@icddrb.orgFind a digital copy of this brief at:Centre for Gender and Health, UCLwww.ighgc.org/projects/pa4ncdsHealthy Societies 2030www.healthysocieties2030.org/ncds/policy
National Strategic Plan For HIV and AIDS Response 2011-2015 "By the year 2010, people at risk of HIV infection will have access to the means of protection in ways that respect their human rights and dignity and will be empowered to protect themselves and others." National Strategic Plan For HIV and AIDS Response 2004-2010 NCD POLICY HIV POLICY