Transcription
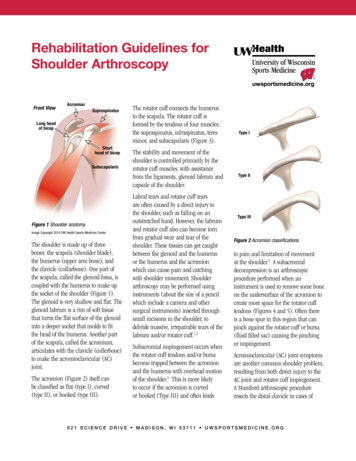
U W H e a lth S p o rts R e h a b i l i t a t i o nRehabilitation Guidelines forBiceps TenodesisThe shoulder has two primary joints.One part of the shoulder blade, calledthe glenoid fossa forms a flat, shallowsurface. This is coupled with thehumerus (shaped like a golf ball) tomake up the joint. The glenoid labrumis a ”ring” of cartilage that turns theflat surface of the glenoid into a slightlydeeper socket, which is similar to restinga golf ball on a golf tee instead of atable top, providing more shoulderstability. Another part of the scapula,called the acromium, articulates withthe clavicle (collar bone) to make theacromioclavicular (AC) joint.The rotator cuff is a group offour muscles: the supraspinatus,infraspinatus, teres minor, andsubscapularis. The rotator cuff tendonsattach around the humeral head (ball)and connects the humerus to thescapula.The long head of the biceps originatesfrom the top of the glenoid fossa andlabrum (top of the golf tee). It thenruns through a groove in the humerus(upper arm bone) to join the short headof the biceps and inserts on a bone inthe forearm1 (See Figure 1). Because ofits position, the long head of the bicepsis also considered to be a secondarystabilizer of the shoulder joint.The long head of the biceps is at riskof injury and degenerative changesdue to its proximity to the rotatorcuff and the acromium. Since thelong head of the biceps can act as asecondary stabilizer of the shoulder, itis also subject to injury during highspeed overhead movements; repetitiveoverhead movements; or forcefulshoulder activities when the elbow isstraight. Specific injuries may includeinflammation and irritation of the biceptendon itself; a problem with the biceptendon in conjunction with one of therotator cuff tendons; or detachment ofpart of the tendon from the attachmentpoint (SLAP tear).1 Bicep tendondegeneration and/or tearing can causesignificant shoulder discomfort anddysfunction (See Figure 2).A biceps tenodesis is a surgicalprocedure which may be performedfor treatment of severe symptomsinvolving the biceps tendon, includinginflammation or partial tears. It maybe performed in isolation or as part ofa larger shoulder surgery, includingsurgery involving the rotator cuff.During the biceps tenodesis, the normalattachment of the biceps tendon on theshoulder socket (glenoid fossa) is cutand reattachment of the tendon is madeon the humerus (upper arm bone).This takes the pressure off the bicepsattachment and places the attachmentbelow the actual shoulder joint.2 Thegoal is to eliminate the shoulder paincoming from the bicep tendon.Different techniques are used toperform a biceps tenodesis. The surgicaltechniques can be broken down in totwo categories: soft tissue techniquesand hardware fixation techniques. Bothtechniques are effective, and chosenbased on surgeon preference and patientindications.The primary soft tissue technique is the“open key hole procedure”. An openkeyhole technique relocates the tendonwithin the groove in the humerus boneafter cutting it from its original locationin the shoulder.1 The procedure involvesthe proximal end (the portion closest tothe it from its original location in theshoulder.) of the biceps tendon beingrolled into a ball and then suturedFront ViewAcromionSupraspinatusLong headof bicepShorthead of bicepSubscapularisFigure 1 Shoulder anatomyImage Copyright 2010 UW Health Sports Medicine Center.The world-class health care teamfor the UW Badgers and proudsponsor of UW Athletics6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o rtsm e d i c i n e . o rg
Rehabilitation Guidelines for Biceps Tenodesistogether as a mass. A keyhole is made inthe groove of the humerus, the tendonmass is then inserted into the keyholeand pulled downward so that the tendonmass is locked in place.3The Pitt technique uses two needlesto pierce the bicep tendon in oppositedirections. Sutures are then threadedthrough the needles to make a suture.This procedure is repeated with theneedle placement reversed to create alocking pattern of the sutures. A knotis used to secure the sutures to thetransverse ligament in the shoulderinstead of to the bone.4The hardware fixation techniquesinclude screw fixation or endobuttonFigure 2a Normal long head of bicep.The muscle has a smooth arc from theshoulder to the elbow.2fixation. In the screw fixation the tendonis detached and then place in a holemade at the top of the bicipital groove.Then an interference screw is placed overthe tendon, in to the bone, to hold it inplace. In the endobutton technique thereleased tendon is secured to a button,the button is then secured behind thebone by sliding it in to a smaller hole atthe top of the bicipital groove. Imagine adrywall type anchor where the pressure isapplied from the inside out.Appropriate rehabilitation is vital tooptimizing your outcome after surgery.The rehabilitation guidelines are tailoredto the type of procedure performed,therefore below you will find rehabilitationguidelines for soft tissue fixationtechniques and rehabilitation guidelinesfor hardware fixation techniques.The rehabilitation guidelines arepresented in a criterion basedprogression. General time frames aregiven for reference to the average, butindividual patients will progress atdifferent rates depending on their age,associated injuries, pre-injury healthstatus, rehabilitation compliance andinjury severity. Specific time frames,restrictions and precautions may also begiven to protect healing tissues and thesurgical repair/reconstruction.Figures 2b and Figure 2c Torn long head of bicep. The muscle has retracted toward the elbow.6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r g
Rehabilitation Guidelines for Biceps TenodesisHardware Fixation Techniques PHASE I (Surgery to 4 to 6 weeks after surgery)Appointments Rehabilitation appointments begin within 7 to 10 days after surgery and continue1 to 2 times per weekRehabilitation Goals Protection of the post-surgical shoulder Activation of the stabilizing muscles of the gleno-humeral andscapulo-thoracic jointsPrecautions Sling immobilization required for soft tissue healing Hypersensitivity in axillary nerve distribution is a common occurrence No bicep tension for 6 weeks to protect repaired tissues—this includes avoidinglong lever arm flexion range of motion and no resisted forearm supination, elbowflexion or shoulder flexion Limit external rotation to 40 for the first 4 weeks No extension or horizontal extension past body for 4 weeksRange of Motion (ROM)Exercises Gentle active and active assistive range of motion for the elbow and wrist Pain free, gentle passive range of motion for shoulder flexion, abduction, internalrotation and external rotation to neutral(Please do not exceed the ROMspecified for each exercise andtime period)Suggested TherapeuticExercise Begin week 3 with sub-maximal shoulder isometrics for internal rotation; externalrotation; abduction; and adduction Hand gripping Cervical spine and scapular active range of motion Desensitization techniques for axillary nerve distributionCardiovascular Fitness Walking, stationary bike—sling on. No treadmill or swimming Avoid running and jumping due to the distractive forces that can occur at landingHardware Fixation Techniques PHASE II(begin after meeting Phase I criteria, usually 6 to 8 weeks after surgery)3Appointments Rehabilitation appointments are 1 time a week for 1 to 2 weeksRehabilitation Goals Full active range of motion Full rotator cuff strength in a neutral positionPrecautions Begin bicep progressive resistive exercises very gradually—this includes avoidinglong lever arm flexion range of motion and avoiding resisted forearm supination,elbow flexion or shoulder flexion No passive range of motion for abduction and external rotation or extension6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r g
Rehabilitation Guidelines for Biceps TenodesisROM Exercises(Please do not exceed the ROMspecified for each exercise andtime period) Shoulder active range of motion Shoulder passive range of motion for flexion or abduction if neededSuggested TherapeuticExercise Scapular squeezes Internal and external rotation in neutral with Theraband resistance—make sure patient is not supinating with external rotation movement Ball squeezesCardiovascular Fitness Walking and/or stationary bike without using arms (No Airdyne) No treadmill, swimming or runningHardware Fixation Techniques PHASE III(begin after meeting Phase II criteria, usually 8 to 12 weeks after surgery)Appointments Rehabilitation appointments are 1 to 2 times per weekRehabilitation Goals Full active range of motion in all cardinal planes with normal scapulo-humeralmovement. 5/5 (full strength) rotator cuff strength at 90 abduction in the scapular plane 5/5 peri-scapular strengthPrecautions All exercises and activities to remain non-provocative and low to medium velocity Avoid activities where there is a higher risk for falling or outside forces to be appliedto the arm No Swimming, throwing or sportsSuggested TherapeuticExerciseMotion Posterior glides if posterior capsule tightness is presentStrength and Stabilization Flexion in prone, horizontal abduction in prone, full can extension, and D1 and D2diagonals in standing Theraband, cable column, and/or dumbbell (light resistance/high repetitions) ininternal rotation and external rotation in 90 of abduction Rowing Balance board in push-up position (with rhythmic stabilization); prone Swiss ballwalkouts; rapid alternating movements in supine D2 diagonal; and closed kineticchain stabilization with narrow base of support4Cardiovascular Fitness Walking, biking, Stairmaster and running (if Phase II criteria is met) No swimmingProgression Criteria The patient can progress to Phase IV if they have met the above stated goals andhave no apprehension or impingement signs6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r g
Rehabilitation Guidelines for Biceps TenodesisHardware Fixation Techniques PHASE IV(begin after meeting Phase III criteria, usually 12 weeks after surgery)Appointments Rehabilitation appointments are once every 2 to 3 weeksRehabilitation Goals Patient to demonstrate stability with higher velocity movements and change ofdirection movements 5/5 (full strength) rotator cuff strength with multiple repetition testing at 90 abduction in the scapular plane Full multi-plane active range of motionPrecautions Progress gradually into provocative exercises by beginning with low velocity, knownmovement patternsSuggested TherapeuticExerciseMotion Posterior glides if posterior capsule tightness is presentStrength and Stabilization Dumbbell and medicine ball exercises that incorporate trunk rotation and controlwith rotator cuff strengthening at 90 abduction Begin working towards more functional activities by emphasizing core and hipstrength and control with shoulder exercises Theraband, cable column and dumbbell in internal rotation and external rotation in90 of abduction Rowing Higher velocity strengthening and control, such as the inertial, plyometrics, andrapid Theraband drills. Plyometrics should start with 2 hands below shoulder heightand progress to overhead, then back to below shoulder with one hand, progressingagain to overhead5Cardiovascular Fitness Walking, biking, Stairmaster and running (if Phase II criteria has been met) No SwimmingProgression Criteria Patient may progress to Phase V if they have met the above stated goals and haveno apprehension or impingement signs6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r g
Rehabilitation Guidelines for Biceps TenodesisPHASE V(begin after meeting Phase IV criteria, usually 20 weeks after surgery)Appointments Rehabilitation appointments are once every 2 to 3 weeksRehabilitation Goals Patient to demonstrate stability with higher velocity movements and change ofdirection movements that replicate sport specific patterns (including swimming,throwing, etc) No apprehension or instability with high velocity overhead movements Improve core and hip strength and mobility to eliminate any compensatory stressesto the shoulder Cardiovascular endurance for specific sport or work demandsPrecautions Progress gradually into sport specific movement patternsSuggested TherapeuticExerciseMotion Posterior glides if posterior capsule tightness is presentStrength and Stabilization Dumbbell and medicine ball exercises that incorporate trunk rotation and controlwith rotator cuff strengthening at 90 abduction and higher velocities Begin working towards more sport specific activities Initiate throwing program, overhead racquet program or return to swimmingprogram depending on the athlete’s sport High velocity strengthening and dynamic control, such as the inertial, plyometrics,and rapid Theraband drills6Cardiovascular Fitness Design to use sport specific energy systemsProgression Criteria Patient may return to sport after receiving clearance from the orthopedic surgeonand the physical therapist/athletic trainer6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r g
Rehabilitation Guidelines for Biceps TenodesisSoft Tissue Technique PHASE I (Surgery to 4 to 6 weeks after surgery)Appointments Rehabilitation appointments begin within 7 to 10 days after surgery and continue1 to 2 times per weekRehabilitation Goals Protection of the post-surgical shoulder Activation of the stabilizing muscles of the gleno-humeral andscapulo-thoracic jointsPrecautions Sling immobilization required for soft tissue rest and comfort 3-10 days. Hypersensitivity in axillary nerve distribution is a common occurrence No excessive bicep loading for 6 weeks to protect repaired tissues—shoulderflexion with weights or bandsRange of Motion (ROM)Exercises Gentle active and active assistive range of motion for the elbow and wrist Pain free, gentle passive and active assisted range of motion for shoulder flexion,abduction, internal rotation and external rotation; progress to active motion astolerated.Suggested TherapeuticExercise Begin week 1 with sub-maximal shoulder isometrics for internal rotation; externalrotation; abduction; and adduction Hand gripping Cervical spine and scapular active range of motion Desensitization techniques for axillary nerve distributionCardiovascular Fitness Walking, stationary bike—sling on. No treadmill or swimming Avoid running and jumping due to the distractive forces that can occur at landingSoft Tissue Technique PHASE II(begin after meeting Phase I criteria, usually 6 to 8 weeks after surgery)7Appointments Rehabilitation appointments are 1 time a week for 1 to 2 weeksRehabilitation Goals Full active range of motion Full rotator cuff strength in a neutral positionPrecautions Progressive and graduated nature of return to activityROM Exercises Full elbow range of motion Shoulder active range of motion Shoulder passive range of motion for flexion or abduction if neededSuggested TherapeuticExercise Scapular stabilization exercises Internal and external rotation in neutral with Theraband resistance Gentle bicep and tricep strengthening exercisesCardiovascular Fitness Progressive return to cardiovascular fitness. Avoid activities where there is a higherrisk for falling or outside forces to be applied to the arm6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r g
Rehabilitation Guidelines for Biceps TenodesisSoft Tissue Technique PHASE III(begin after meeting Phase II criteria, usually 8 to 12 weeks after surgery)Appointments Rehabilitation appointments are 1 to 2 times per weekRehabilitation Goals Full active range of motion in all cardinal planes with normal scapulo-humeralmovement. 5/5 (full strength) rotator cuff strength at 90 abduction in the scapular plane 5/5 peri-scapular strengthPrecautions All exercises and activities begin low to medium velocity Avoid activities where there is a higher risk for falling or outside forces to be appliedto the arm No Swimming, throwing or sportsSuggested TherapeuticExerciseMotion Posterior glides if posterior capsule tightness is presentStrength and Stabilization Flexion in prone, horizontal abduction in prone, full can extension, and D1 and D2diagonals in standing Theraband, cable column, and/or dumbbell (light resistance/high repetitions) ininternal rotation and external rotation in 90 of abduction Scapular Stabilization exercises Balance board in push-up position (with rhythmic stabilization); prone Swiss ballwalkouts; rapid alternating movements in supine D2 diagonal; and closed kineticchain stabilization with narrow base of supportCardiovascular Fitness Walking, biking, Stairmaster and running (if Phase II criteria is met) No swimmingProgression Criteria Full rotator cuff and bicep strength on manual muscle testing.Soft Tissue Technique PHASE IV(begin after meeting Phase III criteria, usually 12 weeks after surgery)8Appointments Rehabilitation appointments are once every 2 to 3 weeksRehabilitation Goals 5/5 (full strength) rotator cuff strength with multiple repetition testing at 90 abduction in the scapular plane Patient to demonstrate stability with higher velocity movements and change ofdirection movements that replicate sport specific patterns (including swimming,throwing, etc) No apprehension or instability with high velocity overhead movements Improve core and hip strength and mobility to eliminate any compensatory stressesto the shoulder Cardiovascular endurance for specific sport or work demandsPrecautions Progress gradually into provocative exercises by increasing velocity, andprogressing from known ton unanticipated movement patterns6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r g
Rehabilitation Guidelines for Biceps TenodesisSuggested TherapeuticExerciseMotion Posterior glides if posterior capsule tightness is presentStrength and Stabilization Dumbbell and medicine ball exercises that incorporate trunk rotation and controlwith rotator cuff strengthening at 90 abduction Begin working towards more functional activities by emphasizing core and hipstrength and control with shoulder exercises Theraband, cable column and dumbbell in internal rotation and external rotation in90 of abduction Scapular Stabilization exercises Higher velocity strengthening and control, such as the inertial, plyometrics, andrapid Theraband drills. Plyometrics should start with 2 hands below shoulder heightand progress to overhead, then back to below shoulder with one hand, progressingagain to overhead Initiate throwing program, overhead racquet program or return to swimmingprogram depending on the athlete’s sportCardiovascular Fitness Design to use sport specific energy systemsProgression Criteria Patient may return to sport after receiving clearance from the orthopedic surgeonand the physical therapist/athletic trainerPHASE V(begin after meeting Phase IV criteria, usually 20 weeks after surgery)9Appointments Rehabilitation appointments are once every 2 to 3 weeksRehabilitation Goals Patient to demonstrate stability with higher velocity movements and change ofdirection movements that replicate sport specific patterns (including swimming,throwing, etc) No apprehension or instability with high velocity overhead movements Improve core and hip strength and mobility to eliminate any compensatory stressesto the shoulder Cardiovascular endurance for specific sport or work demandsPrecautions Progress gradually into sport specific movement patterns6 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r g
Rehabilitation Guidelines for Biceps TenodesisSuggested TherapeuticExerciseMotion Posterior glides if posterior capsule tightness is presentStrength and Stabilization Dumbbell and medicine ball exercises that incorporate trunk rotation and controlwith rotator cuff strengthening at 90 abduction and higher velocities Begin working towards more sport specific activities Initiate throwing program, overhead racquet program or return to swimmingprogram depending on the athlete’s sport High velocity strengthening and dynamic control, such as the inertial, plyometrics,and rapid Theraband drillsCardiovascular Fitness Design to use sport specific energy systemsProgression Criteria Patient may return to sport after receiving clearance from the orthopedic surgeonand the physical therapist/athletic trainerThese rehabilitation guidelines were developed collaboratively by Marc Sherry, PT, DPT, LAT, CSCS, PES(msherry@uwhealth.org) and the UW Health Sports Medicine physician group.Updated 1/2014References1. Krupp RJ, Kevern MA, Gaines MD, KotaraS, Singleton SB. Long Head of the BicepsTendon Pain: Differential Diagnosis andTreatment. Jour Ortho & Sports PT.Feb 2009; 39(2): 55-70.2. Romeo AA, Mazzocca AD, TauroJC. Arthroscopic Biceps Tenodesis.Arthroscopy. Feb 2004; 20(2): 206-213.3. Ozalay M, et al. Mechanical Strengthof Four Different Biceps TenodesisTechniques. Arthroscopy: Jour Arthro &Related Surg. Aug 2005; 21(8): 992-998.4. Lopez-Vidriero E, Costic RS, Fu FH,Rodosky MW. Biomechanical Evaluationof 2 Arthroscopic Biceps Tenodesis:Double-Anchor Versus PercutaneousIntra-Articular Transtendon (PITT)Techniques. Am Jour Sports Med.2010; 38(1): 146-152.6. Burns JP, Bahk M, Snyder SJ. Superiorlabral tears: repair versus bicepstenodesis. J Shoulder Elbow Surg. 2011Mar;20(2 Suppl):S2-8. doi: 10.1016/j.jse.2010.11.013.5. Slenker NR, Lawson K, Ciccotti MG,Dodson CC, Cohen SB. Biceps tenotomyversus tenodesis: clinical outcomes.Arthroscopy. 2012 Apr;28(4):576-82. doi:10.1016/j.arthro.2011.10.017. Epub 2012Jan 28.Copyright 2014 UW Health Sports Medicine Center106 2 1 S c i e n c e D r i v e M a d i s o n , W I 5 3 7 1 1 u ws p o r t sm e d i c i n e . o r gSM-38331-14At UW Health, patients may have advanced diagnostic and /or treatment options, or may receive educational materials that vary from this information. Please be aware that this information is not intended to replacethe care or advice given by your physician or health care provider. It is neither intended nor implied to be a substitute for professional advice. Call your health provider immediately if you think you may have a medicalemergency. Always seek the advice of your physician or other qualified health provider prior to starting any new treatment or with any question you may have regarding a medical condition.
Strength and Stabilization Dumbbell and medicine ball exercises that incorporate trunk rotation and control with rotator cuff strengthening at 90 abduction and higher velocities Begin working towards more sport specific activities Initiate throwing program, overhead racquet program or return to swimming