Transcription
M IN D SCAPE SMASS GENERAL DEPARTMENT OF PSYCHIATRY NEWSLETTER FOR FRIENDS AND SUPPORTERS SPRING 2018Helping patients on medical and surgical unitsIEmbedded psychiatrists and psychologists work to reduce complications and stresst’s okay to see wild animals roaming close upwhen you’re on safari — but not when they’re in yourhospital room.Yet, that’s what 67-year-old Walter J experienced during aprolonged hospital stay following spine surgery for acute back pain.Over time, he became increasingly detached from hospital staff anddisinterested even in his family’s visits. Then he refused oralmedications. The bedside nurse outwardly observed that Mr. J“seems to have just givenup” — a clear sign ofdepression. Inwardly, thesituation was far worse.And, who would expectthat treatment for restlesslegs would cause a medicalcrisis? It happened toMary W, a 47-year-oldpatient with bipolardisorder and serious kidneydisease who was admittedto Mass General afterrefusing treatment at herlocal hemodialysis centerand exhibiting paranoiddelusions directed towardthe staff.the medical team, the CL recommended a different RLSmedication that helped Ms. W’s paranoia recede and allowedher to resume hemodialysis.The CL called to consult on Mr. J’s case learned that Mr. J had seenwild animals running through his room and was fearing for hissanity. Guided by years of training and experience, the CL realizedMr. J was exhibiting signs of delirium, a dangerous condition thatwarranted additional medical tests. One of these revealed apreviously undetectedurinary tract infection, thetreatment for which helpedstop Mr. J’s delirium inits tracks.Care at the Bedside“Being hospitalized for amedical illness is stressful,”observes Felicia A. Smith,MD, director of both theMGH Division of Psychiatry& Medicine and PsychiatryConsultation Services.“Patients with a history ofmental illness are certainly atelevated risk for developingpsychiatric complicationswhen they’re admitted forTheodore A. Stern, MD, Chief Emeritus, Avery D. Weisman, MD Psychiatry ConsultationService; Felicia A. Smith, MD, Chief, Avery D. Weisman, MD Psychiatry Consultationmedical reasons. But theConsultationService; Nicholas Kontos, MD, Director, Fellowship in Consultation-Liaison Psychiatry;same complications nofPsychiatryandMedicine.Liaisonsdevelop with any patientIn cases like these — andwhen the diagnosis of a disease or its treatment triggers emotional,thousands of others each year — experts from the Department ofbehavioral or cognitive effects,” Dr. Smith explains.Psychiatry’s Consultation Service are called to the bedside inmedical or surgical wards to identify and treat patients’ behavioralCLs typically do their assessments in the tight quarters ofand neurocognitive symptoms.two-bedded hospital rooms amid IV poles, tray tables and thesignals and alarms of medical equipment — often with patientsBy integrating specialized, deep knowledge of both psychiatry andattached to various tubes and wires. Adding to those physicalmedicine, the Consultation Service Liaisons — or CLs, as they arechallenges, medically ill patients stay in the hospital only six days onknown — are able to resolve psychiatric complications that canaverage. “Locating a pathological condition along the vast borderchallenge medical staff and interfere with the patient’s medical carebetween psychiatry and medicine, determining the root cause andand mental well-being.treating it quickly is the fundamental task and challenge of consultationIn Ms. W’s case, the CL discovered that a recent dosage increase inpsychiatry,” notes Theodore Stern, MD, chief emeritus of theher medication for restless leg syndrome (RLS) was interactingPsychiatry Consultation Service and director from 1978 to 2017.badly with her medication for bipolar disorder. Working with(Continued on page 7)
From the ChiefOur spring issue highlights the roleof the department of Psychiatry inthe quality of care at Mass General.About 43,000 people of all ages areadmitted to our medical andsurgical units each year. For morethan one in six patients, apsychiatrist or psychologist servesas a member of the care team – alevel of collaboration that is perhapsthe highest in the nation.These specially trained cliniciansmay be called upon when a patient with a pre-existingpsychiatric disorder needs to be treated in a hospital wardfor a serious disease, injury or illness. The stress of thehospital environment, despite the attentiveness of staff orthe amenities, can trigger a worsening of behavioral andemotional symptoms.The inverse also applies. A patient who has never had amental health issue can suddenly develop anxiety,depression or paranoia, or become disruptive. This canhappen because of the side effects of medication, thedistress of a life-threatening diagnosis, or the impact of adisease or injury in the brain. Our psychiatry consultationliaisons, CLs as they are called, work at the patient’sbedside to sort out the complex “chicken or egg” questionsabout the cause of psychiatric symptoms.The article on gratitude also underscores our faculty’sinterest in the connection between mental and physicalhealth. Depression can compromise a person’s successfullong term recovery from a heart attack. Observing thisrelationship first hand, Dr. Jeff Huffman set out to developa clinical intervention based on positive psychology, andits encouraging results are shared.The theme of gratitude, but of another kind, continues inthis issue with a profile of donors Liz and Kent Dautenwhose generosity established the Dauten Center forBipolar Treatment Innovation. For an illness that affectsthree in 100 adults, research to develop more effective,better tolerated clinical remedies is urgently needed, so weare deeply appreciative of the Dautens’ philanthropiccommitment and of their extra gift in linking their nameswith this vital work.Jerrold F. Rosenbaum, MDPsychiatrist-in-Chief,Massachusetts General HospitalStanley Cobb Professor of Psychiatry,Harvard Medical SchoolPAG E T WOFaculty NewsErin Dunn, ScD, of the Center forGenomic Medicine (CGM), andRakesh Karmacharya, MD, PhD, ofthe Psychiatric and NeurodevelopmentalGenetics Unit in the CGM, have receivedErin Dunn, ScDthe National Instituteof Mental Health Biobehavioral ResearchAward for Innovative New Scientists.Dunn will undertake the study“Childhood adversity, DNA methylation,and risk for depression,” whileKarmacharya’s research will be “Ex vivoRakesh Karmacharya,signature of psychosis and treatmentMD, PhDresponse in patient-derived neurons.”Jacob Holzer, MD, has received theHarvard Medical School Program inPsychiatry and the Law Larry H.Strasburger, MD, Award for OutstandingForensic Presentation. Holzer, who receivedthe award for “Individual anti-governmentrhetoric, violence, and vulnerability: loneJacob Holzer, MDactor violence,” is the lead co-editor of thetextbook Geriatric Forensic Psychiatry: Principals and Practice,2018, published by Oxford University Press.Stephanie Sogg, PhD, psychologist inthe MGH Weight Center, has been awardedthe American Society for Metabolic andBariatric Surgery’s (ASMBS) 2017Distinguished Behavioral Health ProviderAward. This award recognizes an ASMBSbehavioral health member who has madeStephanie Sogg, PhDan extraordinary effort for promoting thevalues of behavioral health: clinical excellence, advocacy, researchand education.Olivia I. Okereke, MD, MS, director ofGeriatric Psychiatry Research, was elected asan At-Large Board Member of the AmericanAssociation of Geriatric Psychiatry. Withnearly 2,000 geriatric psychiatrists and otherhealthcare professionals, the associationOlivia I. Okereke,MD, MSpromotes the mental health and well-being ofolder people through professional education, public advocacy andsupport of career development for clinicians, educators andresearchers in geriatric psychiatry and mental health.Luana Marques, PhD, director ofCommunity Psychiatry, PRIDE (Programfor Research in Implementation andDissemination of Evidence-BasedTreatments) is the President-Elect of theAnxiety and Depression Association ofLuana Marques, PhD America. Dr. Marques has been an activemember of the association — with itsmore than 1,800 professional members — since 2008 and hasserved on the board since 2016.MINDSCAPES S P R I N G 2 01 8
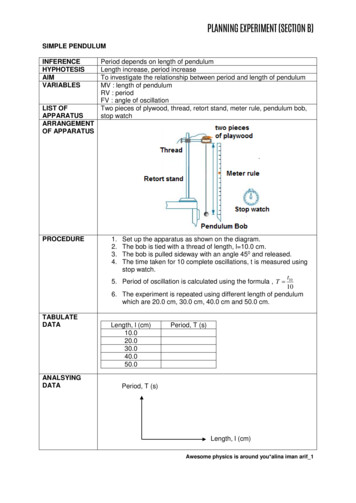
A Grateful Life May be a Longer LifeRecovery in Heart Disease Tied to Psychological FactorsIn 63 B.C., the Roman politician and lawyer Cicero wrote, “Gratitudeis not only the greatest of the virtues but the parent of all others.”Huffman and Lyubomirsky, who is professor of Psychology at theUniversity of California, Riverside, soon decided to study the linkbetween gratitude and recovery. “Gratitude is important, complexand powerful. Not all people who have a medical event experiencesignificant gratitude – only about half of patients we’ve encountered,in fact,” says Huffman.More than 2,000 years later, the understanding of gratitude has receiveda scientific twist, thanks in part to the MGH Cardiac Psychiatry ResearchProgram (CPRP). Led by Jeff Huffman, MD, director of ClinicalS er vicesintheDepartment of Psychiatry,the program focuses onthe connections betweenmental health andmedical health in patientso Exerciseswith heart disease and Week 1: Gratitude for Positive Eventsother chronic conditions. Week 2: Personal StrengthsA key component is the Week 3: Gratitude Letterrole of optimism and Week 4: Enjoyable and Meaningful Activitiesgratitude in health andhow these positive Week 5: Remembering Past SuccessPositivepsychological states may Week 6: Acts of KindnessPsychology forimpact – and, possiblyHealthy Recovery Weeks 7 & 8: Participant Choiceimprove – outcomes forpatients with chronic oracute illnesses, like a heartattack or type 2 diabetes.The study of gratitude andits impact on patients’long-term health dates toHappiness-promoting activities that patients with heart disease practiced in a research studyHuffman’s early days asconducted by the MGH Cardiac Psychiatry Research Program.a psychiatrist.To understand the rolegratitude plays in cardiacrecovery, Huffman andcolleagues in the MGHCPRP enrolled 164people hospitalized for aheart attack, having themreturn two weeks after,where they completed aformal measure of overallgratitude and specificgratitude related to health.Six months later, theywere asked to wear stepcounters for a week togatheradditionalinformation about theirrecovery. The team foundthat gratitude at twoweeks was associated withoverall greater adherenceto medication, healthierdiet and more exercise sixmonths later, as well as better health-related quality of life and lowerrates of developing depression and anxiety.Happiness and Health Program“I have always been interested in this relationship,” says Huffman. “Overtime, as I was seeing patients in the hospital, I began to have a goodsense about who was going to recover successfully, and who was not,which was often based on psychological factors.” Some patients weretemporarily depressed after a cardiac event, but still hopeful about gettingbetter. They seemed to recover well. Other patients were not necessarilydepressed, but at the same time lacked motivation, gratitude, or hope.They really struggled.The CPRP team believes a positive and grateful approach to life isteachable and has been testing this with therapeutic activities likewriting a letter of gratitude, using humor, capitalizing on personalstrengths, recalling past success and doing kind acts of all sizes. Theresults are gaining momentum on a national level. The CPRP nowhas support from theNational Institutes of“Gratitude is important, complex andHealth and thepowerful. Not all people who have aAmerican DiabetesAssociation to studymedical event experience significantthese interventionsgratitude – only about half of patientsin patients with heartattac ks, c hronicwe’ve encountered, in fact.”heart disease, andtype 2 diabetes.— Jeff C. Huffman, MD“For years, I had quietlykept this idea about thelink between positivityand recovery. Then oneday I happened across abook by a researchernamedSonjaLyubomirsky, PhD.She’s a major contributorto the field of ‘positivepsychology’ and the scientific evidence that being happier, more hopeful,and having greater well-being can improve health outcomes. I thought:this is exactly what my patients need!”PAG E T H R E E“We are excited tofurther this area of research in the hope that this gratitude and wellbeing-focused intervention really might help people get and stayhealthy,” says Huffman. “And for heart attack patients, the stakes couldnot be higher.”MINDSCAPES S P R I N G 2 01 8
The Dauten Family Center for BipolarGift from Chicago couple creates a global hub forNKent and Liz Dautenearly three of 100 adults 18 and over inthe United States had bipolar disorder in the lastyear, and it’s estimated that more than four of 100will experience bipolar disorder at some time in their lives.For Chicago area residents Liz and Kent Dauten, these statisticsare very personal. Two of their four children were diagnosedwith the disorder in their mid to late teens. “After theircompletely normal childhoods, it was like a lightning boltstruck our entire family,” said Kent Dauten.The couple set out to learn about an illness they “had hardlyheard of ” and to get their children launched on the treatmentjourney. They also resolved to make advancing knowledge andtreatment of bipolar disorder their top philanthropic priority.Inspired by the compassionate treatment of one of theirchildren as well as the forward-thinking research of AndrewNierenberg, MD, the Dautens made a gift in 2016 to MassGeneral to launch a new center that would revolutionizeunderstanding of the disorder.Innovative ThinkingBipolar disorder is a lifelong mood disorder resulting inalternating episodes of mania and depression. It often recurs,even with treatment. Despite recent progress identifying genesthat contribute to the development of the disorder, thebiological underpinnings are not well understood. Researchfunding is sparse even though the disease costs patients, familiesand society an estimated 210 billion a year.PAG E F O U R“Bipolar disorder costs a lot in terms of personal suffering andthe monetary cost is staggering. Even though it’s so prevalent,it is grossly understudied,” says center director Dr. Nierenberg.Dr. Nierenberg, Professor of Psychiatry at Harvard MedicalSchool and the Thomas P. Hackett Chair of Psychiatry atMass General, is among the most widely cited internationalexperts on bipolar disorder.“Our wildest dream is for scientists tobe able to understand the genetic pieceof [bipolar disorder] and developtherapies. And even beyond that,we hope to see the development ofpersonalized therapies that might bespecific to individual patients.”— Kent DautenThe last time a drug was developed specifically to treat bipolardisorder was 70 years ago, when lithium was introduced.Lithium has a variety of side effects that drive the urgency tofind new treatments.Breaking the Log JamThe Dautens hope to break that log jam. “Our wildest dreamis for scientists to be able to understand the genetic piece ofit and develop therapies,” Mr. Dauten says. “And even beyondMINDSCAPES S P R I N G 2 01 8
Treatment Innovationresearch, education and outreachthat, we hope to see the development of personalized therapiesthat might be specific to individual patients.”That’s why Dauten Center researchers are casting a wide net.They are collaborating with researchers around the globe —the University of Oxford, University of Paris, Deakin Universityin Australia, University of Toronto, and McLean Hospital inBelmont, Mass. — to create an epicenter of research,coordinating studies and pursuing innovative ideas.A Disorder of Brain MetabolismDr. Nierenberg points to promising evidence that bipolardisorder is a disorder of brain energy metabolism — theprocess by which cells convert nutrients into energy. Becausebipolar disorder patients swing from periods of very highbrain energy (mania) to periods of low energy (depression),a major study of the center is using imaging technology tolook for abnormalities of brain metabolism in people withbipolar disorder.To explore the development of new medications,Dr. Nierenberg and fellow clinician-researchers are testing avariety of drugs against brain cells (neurons) of people withbipolar disorder grown in laboratory conditions. They are alsostudying lifestyle factors such as diet, exercise and mindfulness.As part of its mission to educate the next generation ofresearchers, the center also hosts research fellows and visitingprofessors from around the world.The Stigma of Bipolar DisorderOrdinarily circumspect about their philanthropic interests,the Dautens decided to give their name to the center to helpfight the stigma of mental illness that often prevents peoplefrom seeking treatment and providing funding. Before decidingto give their name to the center, they talked with their children.“Our name is their name, too,” Mr. Dauten says. “We allagreed, if we’re not willing to put our names on this, whatdoes that say about our small part in the battle to fightthat stigma?”Dr. Nierenberg admires their decision. “Kent and Liz are reallywonderful people who want to make a difference and showby example that they are willing to fight stigma and inspireothers to do similarly. Their generosity and engagement haveinspired others to contribute and to help guide our clinicalprogram and promote participation in research.” The centernow has a growing advisory council of patients and familymembers motivated to support innovation. Liz and KentDauten were its first members.Adapted from an article by Kay Cahill published ongiving.massgeneral.org, February 2018.PAG E F I V EThe Top 10 Reasons Why theWorld Needs a Center forBipolar Treatment Innovation(10) There is no cure for the lifelong condition of Bipolar Disorder,only treatments which are more trial-and-error guessworkthan science.(9) The last major drug discovery specific to treating BipolarDisorder was in 1948 when an Australian researcheraccidentally discovered that Lithium is an effective moodstabilizer. It is still considered the gold standard 70 years laterdespite its limitations.(8) Most mood stabilizing drugs for Bipolar Disorder havesignificant side effects like gastrointestinal distress/diarrhea,rapid and severe weight gain, rashes, and tremors; thisoften leads to medication non-compliance and furthercomplicates treatment.(7) The manic phase of Bipolar Disorder makes patients feel sogood, even euphoric, that they stop taking medications, socompliance suffers (as can their savings accounts, personalrelationships and jobs).(6) There is no medical test to predict whether an individual willdevelop Bipolar Disorder, so you just have to wait for thepeculiar and dangerous behavioral symptoms to present inorder to diagnose it. The length of time from a person’s firstBipolar symptoms to correct diagnosis and treatment typicallyranges from 3 ½ to 10 years.(5) The symptoms of Bipolar Disorder can range from debilitatingdepression to euphoric mania to extreme psychosis. To anoutsider, someone with Bipolar Disorder may be incorrectlyperceived as being unmotivated, apathetic and even lazy.(4) Bipolar Disorder episodes can cause individuals to dropout of life for months at a time due to extended hospitalizationand the search for effective medication regimens, sacrificingschooling, jobs, and friendships along the way.(3) Although it may be improving, Bipolar Disorder is stillsuch a stigmatized mental illness that individuals and theirfamilies are reluctant to speak about it in public (if at all), andoften cope with it alone rather than with social support as isthe case with other diseases.(2) With most other illnesses you “have” them; with BipolarDisorder you “are” the disease. A person can have cancer butis Bipolar. Even worse, while other diseases can kill you, withBipolar Disorder you are perceived as killing yourself, giventhe high risk of suicide.(1) Over 6 million people in the United States alone suffer fromthis devastating and life-altering illness—we can and need todo better!From remarks by Kent and Liz Dauten at the opening of theDauten Center for Bipolar Treatment Innovation, October 16, 2017.MINDSCAPES S P R I N G 2 01 8
MGH Psychiatry Out and AboutThe Alice and Harold Alpert Psychiatry GrandRounds Lecture in Medical Education,January 25, 2018Benefit for the MGH NeurotherapeuticsProgram, Sistina Restaurant, New York,March 19, 2018Jerrold F. Rosenbaum, MD; Edward M. Hundert, MD, Alpert Grand Roundsguest speaker; Jonathan E. Alpert, MD, PhD, former associate chief ofPsychiatry at MGH; Maurizio Fava, MDJoan A. Camprodon, MD, PhD, MPHDirector, Division of Neuropsychiatry and NeuromodulationBreakfast Seminar, London, England, May 3, 2018Jerrold F. Rosenbaum, MDPeter L. Slavin, MDMalik Dahlan, MGH President’s Council Member, withLeadership Council for Psychiatry Members,Donna Stearns and Dale SinesiPAG E S I XNearly 100 guests gatheredon Thursday, May 3 atClaridge’s in London for abreakfast seminar,Advances and Innovations inMental Health Care.The event featuredpresentations byDrs. Jerry Rosenbaum,Maurizio Fava andJanet Wozniak, followed bya panel discussionmoderated by Mass GeneralPresident, Dr. Peter Slavin.Claridge’sJanet R. Wozniak, MDMaurizio Fava, MDBritain W. Nicholson, MDSenior Vice Presidentand Chief Development OfficerMINDSCAPES S P R I N G 2 01 8
(Continued from page 1)Highly Specialized, Expert TeamThe impact of the CLs in the quality of inpatient care at MassGeneral is considerable, with medical and surgical teams requestingconsultations for nearly 7,000 of the 43,000 patients admittedannually, making it one of the busiest and largest psychiatryconsultation services in the country. The Psychiatry ConsultationService was opened in 1956 and later named for its founder, iconicpsychiatrist Avery Weisman, MD.“Locating a pathological condition alongthe vast border between psychiatry andmedicine, determining the root cause andtreating it quickly is the fundamental task andchallenge of consultation psychiatry.”— Theodore A. Stern, MDThe program’s current faculty includes 10 full-time-equivalentconsulting psychiatrists augmented by a core group of third-yearpsychiatry residents. Further support is provided by three fellowschosen each year to participate in the MGH Fellowship inPsychosomatic Medicine, which is the oldest consultationpsychiatry training program in the country, according to FellowshipDirector Nick Kontos, MD.The team’s psychiatrists and psychologists have expertise in specificmedical disciplines, such as cardiology, oncology and neurology. Someof them are expert in the special needs of heart, liver, kidney and lungtransplant recipients; victims of burns, opiate overdoses and othertraumas; and patients with HIV/AIDS and other infectious diseases.A separate Pediatric Psychiatry Consultation Program is devoted tosupporting medically ill children and adolescents.Care in Outpatient Settings“The close partnership of CLs with their medical and surgicalcolleagues has helped shape a culture of mutual respect with theDepartment of Medicine and the rest of the hospital,” notesDr. Stern. It also increases accuracy and efficiency in a difficult,acute care environment. Neuropsychiatric symptoms can produceunpredictable and sometimes violent behaviors that are lifethreatening to the patient, and dangerous for medical staff. “Therapid response by CLs to diagnose and treat through behavior orchemical intervention often makes a huge difference in very serioussituations,” says Nadia Quijije, MD, director of the Burns andTrauma Consultation team.Caring forChildren and TeensAttending to an adult medical patientwho is unwilling or unable to talk can be difficult, butworking with children and adolescents — who oftendon’t have the language skills or vocabulary todescribe what’s wrong or how they feel — can beeven harder.This is the daily challenge that the PediatricPsychiatry Consultation Service team addresseswithin the inpatient units and outpatient clinics ofMassGeneral Hospital for Children (MGHfC). Led byEric Hazen, MD, and Elizabeth Pinsky, MD, the teamincludes five part-time child and adolescentElizabeth G. Pinsky, MD, and Eric P. Hazen, MDpsychiatrists and two part-time child psychologists.The group also works with severe burn victims at nearby Shriners Hospital for Children in Boston.All are specially trained in the developmental needs of patients ranging in age from toddlers to late adolescents and sometimesyoung adults. Most of them are dealing with a range of illnesses — from injuries and other physical trauma, to the medicalcomplications of eating disorders or attempted suicides, to the impact of chronic conditions like epilepsy and asthma, topotentially life-threatening illnesses like cancer and cystic fibrosis.“We help patients and their families cope with the symptoms that these conditions and diseases trigger and with the side effects ofvarious treatments — including depression, anxiety, acting out and not cooperating with their care,” notes Dr. Hazen. “A primarygoal is to help everybody involved understand the child’s experience, to allow the child to feel safe again.”The team also plays a critical role in being quarterbacks for their care, adds Dr. Hazen. “We get all the information, put it together,and make sure everyone involved — the patient, family, medical providers, and sometimes others outside the hospital — knowsthe treatment plan.”Each year the team collaborates with medical and surgical colleagues in caring for upwards of 500 young patients in the hospitaland some 250 others in MGHfC’s outpatient pediatric specialty practices, according to Dr. Hazen.PAG E S E V E NMINDSCAPES S P R I N G 2 01 8
NONPROFIT ORGU.S. POSTAGEPAIDN.READING, MAPERMIT NO. 211Development Office125 Nashua Street, Suite 540Boston, MA 02114-2548MINDSCAPES S P R I N G 2 01 8Save These DatesPsychiatry Academy Patient and Family Education SeriesSaturday, June 23, 2018Bipolar Education DayDirected by Andrew A. Nierenberg, MDSponsored by the Dauten Family Center for Bipolar Treatment InnovationSaturday, September 22, 2018Substance Use DisordersDirected by John F. Kelly, PhDSponsored by the Recovery Research InstituteTuesday, October 2, 2018Behavioral Health and the Launch fromAdolescence to Young AdulthoodDirected by Timothy E. Wilens, MDSponsored by the Joan and Leonard Engle Family FoundationSaturday, November 10, 201816th Annual Schizophrenia Education DayDirected by Oliver Freudenreich, MD, and Daphne J. Holt, MD, PhDSponsored by an Anonymous DonorAll sessions are held at the Starr Center, Richard Simches Building,185 Cambridge Street, Charles River Plaza, Boston, EXCEPTthe October 2 event, which takes place in the O’Keefe Auditorium at 5 pm.For more information and to register for all sessions please -educationMINDSCAPESSpring 2018 Vol. 11, No.1CHIEF OF PSYCHIATRYJerrold F. Rosenbaum, MDEXECUTIVE DIRECTOR OFDEVELOPMENTCarol W. TaylorDIRECTOR OF DEVELOPMENTCOMMUNICATIONSRobert TomshoPROJECT MANAGERAidan ParkinsonWRITINGNoah BrownKay CahillJohn HebertEDITORLauren DagneseDESIGNArch MacInnesPHOTOGRAPHYMGH Photo LabErnie Savarese, LondonMindscapes is published forfriends and supporters of theMassachusetts General HospitalDepartment of Psychiatry.www.massgeneral.org/psychiatryIf you do not wish to receive certain orall fundraising communications fromMassachusetts General Hospital,please call our toll-free number,877.644.7733, or visitgiving.massgeneral.org/com-pref.
MASS GENERAL DEPARTMENT OF PSYCHIATRY NEWSLETTER FOR FRIENDS AND SUPPORTERS SPRING 2018 MINDSCAPES Helping patients on medical and surgical units Embedded psychiatrists and psychologists work to reduce complications and stress t's okay to see wild animals roaming close up when you're on safari — but not when they're in your hospital .