Transcription
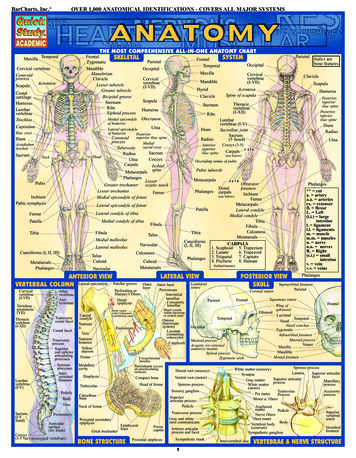
Copyright EMAP Publishing 2020This article is not for distributionexcept for journal club useClinical PracticeSystems of lifeSkeletal systemKeywords Skeletal system/Bonephysiology/Musculoskeletal healthThis article has beendouble-blind peer reviewedIn this article. T he key functions and structure of bone Bone formation and growth, and the process of remodelling Diet and lifestyle factors that can affect bone structureSkeletal system 1:the anatomy and physiology of bonesKey pointsBones are key toproviding the bodywith structuralsupport andenabling movementMost of the body’sminerals are storedin the bonesDiet and lifestyle canaffect the quality ofbone formationAfter bones haveformed theyundergo constantremodellingFRANCESCA CORRAChanges in theremodelling processcan result inpathology such asPaget’s disease ofbone or osteoporosisAuthor Jennie Walker is principal lecturer, Nottingham Trent University.Abstract The skeletal system is formed of bones and cartilage, which are connectedby ligaments to form a framework for the remainder of the body tissues. This article,the first in a two-part series on the structure and function of the skeletal system,reviews the anatomy and physiology of bone. Understanding the structure andpurpose of the bone allows nurses to understand common pathophysiology andconsider the most-appropriate steps to improve musculoskeletal health.Citation Walker J (2020) Skeletal system 1: the anatomy and physiology of bones.Nursing Times [online]; 116: 2, 38-42.The skeletal system is composed ofbones and cartilage connected byligaments to form a framework forthe rest of the body tissues. Thereare two parts to the skeleton:l A xial skeleton – bones along the axis ofthe body, including the skull, vertebralcolumn and ribcage;l A ppendicular skeleton – appendages,such as the upper and lower limbs,pelvic girdle and shoulder girdle.FunctionAs well as contributing to the body’soverall shape, the skeletal system has several key functions, including:l S upport and movement;l P rotection;l M ineral homeostasis;l B lood-cell formation;l T riglyceride storage.Support and movementBones are a site of attachment for ligamentsand tendons, providing a skeletal framework that can produce movement throughthe coordinated use of levers, muscles, tendons and ligaments. The bones act aslevers, while the muscles generate theforces responsible for moving the bones.Nursing Times [online] February 2020 / Vol 116 Issue 2 38ProtectionBones provide protective boundaries forsoft organs: the cranium around the brain,the vertebral column surrounding thespinal cord, the ribcage containing theheart and lungs, and the pelvis protectingthe urogenital organs.Mineral homoeostasisAs the main reservoirs for minerals in thebody, bones contain approximately 99% ofthe body’s calcium, 85% of its phosphateand 50% of its magnesium (Bartl and Bartl,2017). They are essential in maintaininghomoeostasis of minerals in the blood withminerals stored in the bone are released inresponse to the body’s demands, withlevels maintained and regulated by hormones, such as parathyroid hormone.Blood-cell formation (haemopoiesis)Blood cells are formed from haemopoieticstem cells present in red bone marrow.Babies are born with only red bonemarrow; over time this is replaced byyellow marrow due to a decrease in erythropoietin, the hormone responsible forstimulating the production of erythrocytes (red blood cells) in the bone marrow.By adulthood, the amount of red marrowwww.nursingtimes.net
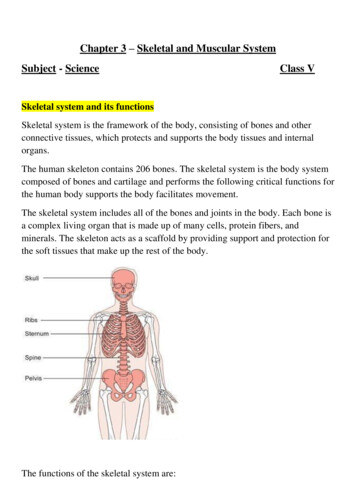
Copyright EMAP Publishing 2020This article is not for distributionexcept for journal club useClinical PracticeSystems of lifeFig 1. Bone structureHyalinecartilageEpiphysisEpiphyseal lineRed bonemarrowStructureBone architecture is made up of two typesof bone tissue:l C ortical bone;l Cancellous bone.Marrow cavityYellow ramenSite ofendosteumSpongybonehas halved, and this reduces further toaround 30% in older age (Robson and Syndercombe Court, 2018).Triglyceride storageYellow bone marrow (Fig 1) acts as a potential energy reserve for the body; it consistslargely of adipose cells, which store triglycerides (a type of lipid that occurs naturally inthe blood) (Tortora and Derrickson, 2009).FRANCESCA CORRABone compositionflexibility to withstand the daily forcesexerted on them. This flexibility and tensile strength of bone is derived from thecollagen fibres. Over-mineralisation of thefibres or impaired collagen production canincrease the brittleness of bones – as withthe genetic disorder osteogenesis imperfecta – and increase bone fragility (Ralstonand McInnes, 2014).Bone matrix has three main components:l 2 5% organic matrix (osteoid);l 5 0% inorganic mineral content(mineral salts);l 2 5% water (Robson and SyndercombeCourt, 2018).Organic matrix (osteoid) is made up ofapproximately 90% type-I collagen fibresEpiphysisand 10% other proteins, such as glycoprotein, osteocalcin, and proteoglycans (Bartland Bartl, 2017). It forms the framework forbones, which are hardened through thedeposit of the calcium and other mineralsaround the fibres (Robson and Syndercombe Court, 2018).Mineral salts are first deposited betweenthe gaps in the collagen layers with oncethese spaces are filled, minerals accumulatearound the collagen fibres, crystallising andcausing the tissue to harden; this process iscalled ossification (Tortora and Derrickson,2009). The hardness of the bone depends onthe type and quantity of the minerals available for the body to use; hydroxyapatite isone of the main minerals present in bones.While bones need sufficient minerals tostrengthen them, they also need to preventbeing broken by maintaining sufficientNursing Times [online] February 2020 / Vol 116 Issue 2 39Cortical boneAlso known as compact bone, this denseouter layer provides support and protection for the inner cancellous structure.Cortical bone comprises three elements:l Periosteum (Fig 1);l Intracortical area;l Endosteum (Bartl and Bartl, 2017).The periosteum is a tough, fibrousouter membrane. It is highly vascular andalmost completely covers the bone, exceptfor the surfaces that form joints; these arecovered by hyaline cartilage. Tendons andligaments attach to the outer layer of theperiosteum, whereas the inner layer contains osteoblasts (bone-forming cells) andosteoclasts (bone-resorbing cells) responsible for bone remodelling.The function of the periosteum is to:l P rotect the bone;l H elp with fracture repair;l N ourish bone tissue (Robson andSyndercombe Court, 2018).It also contains Volkmann’s canals,small channels running perpendicular tothe diaphysis of the bone (Fig 1); theseconvey blood vessels, lymph vessels andnerves from the periosteal surface throughto the intracortical layer. The periosteumhas numerous sensory fibres, so bone injuries (such as fractures or tumours) can beextremely painful (Drake et al, 2019).The intracortical bone is organised intostructural units, referred to as osteons orHaversian systems (Fig 2). These are cylindrical structures, composed of concentriclayers of bone called lamellae, whose structure contributes to the strength of the cortical bone. Osteocytes (mature bone cells)sit in the small spaces between the concentric layers of lamellae, which are known aslacunae. Canaliculi are microscopic canalsbetween the lacunae, in which the osteocytes are networked to each other by filamentous extensions. In the centre of eachosteon is a central (Haversian) canalwww.nursingtimes.net
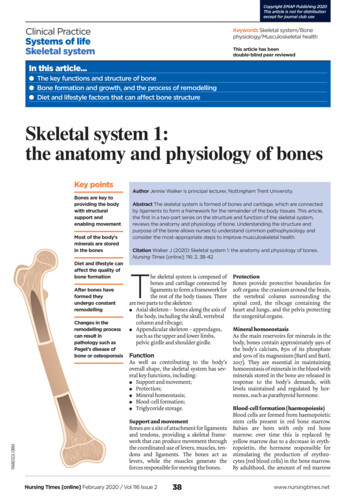
Copyright EMAP Publishing 2020This article is not for distributionexcept for journal club useClinical PracticeSystems of lifeBox 1. Types of bonesFig 2. Anatomy of cortical boneCanaliculiOsteocyteLacunaConcentric lamellaeOsteonInner circumferential lamellaLymphatic vesselOutercircumferentiallamellaPeriosteum:Inner osteogeniclayerMedullarycavityOuter fibrouslayerTrabeculaeCentral canalPerforating canalPeriosteal veinSpongy bonePeriosteal arteryCompact bonethrough which the blood vessels, lymphvessels and nerves pass. These central canalstend to run parallel to the axis of the bone;Volkmann’s canals connect adjacentosteons and the blood vessels of the centralcanals with the periosteum.The endosteum consists of a thin layer ofconnective tissue that lines the inside of thecortical surface (Bartl and Bartl, 2017) (Fig 1).FRANCESCA CORRACancellous boneAlso known as spongy bone, cancellousbone is found in the outer cortical layer. Itis formed of lamellae arranged in an irregular lattice structure of trabeculae, whichgives a honeycomb appearance. The largegaps between the trabeculae help make thebones lighter, and so easier to mobilise.Trabeculae are characteristically oriented along the lines of stress to help resistforces and reduce the risk of fracture (Tortora and Derrickson, 2009). The closer thetrabecular structures are spaced, the greaterthe stability and structure of the bone (Bartland Bartl, 2017). Red or yellow bone marrowexists in these spaces (Robson and Syndercombe Court, 2018). Red bone marrow inadults is found in the ribs, sternum, vertebrae and ends of long bones (Tortora andDerrickson, 2009); it is haemopoietic tissue,which produces erythrocytes, leucocytes(white blood cells) and platelets.Blood supplyBone and marrow are highly vascularisedand account for approximately 10-20% ofcardiac output (Bartl and Bartl, 2017).Blood vessels in bone are necessary fornearly all skeletal functions, including thedelivery of oxygen and nutrients, homoeostasis and repair (Tomlinson and Silva,2013). The blood supply in long bones isderived from the nutrient artery and theperiosteal, epiphyseal and metaphysealarteries (Iyer, 2019).Each artery is also accompanied by nervefibres, which branch into the marrow cavities. Arteries are the main source of bloodand nutrients for long bones, enteringthrough the nutrient foramen, thendividing into ascending and descendingbranches. The ends of long bones are supplied by the metaphyseal and epiphysealarteries, which arise from the arteries fromthe associated joint (Bartl and Bartl, 2017).If the blood supply to bone is disrupted,it can result in the death of bone tissue(osteonecrosis). A common example is following a fracture to the femoral neck,which disrupts the blood supply to thefemoral head and causes the bone tissue tobecome necrotic. The femoral head structure then collapses, causing pain and dysfunction.GrowthBones begin to form in utero in the firsteight weeks following fertilisation (Moini,2019). The embryonic skeleton is firstformed of mesenchyme (connective tissue)structures; this primitive skeleton isreferred to as the skeletal template. Thesestructures are then developed into bone,eitherthroughintramembranousNursing Times [online] February 2020 / Vol 116 Issue 2 40l Long bones – typically longer thanthey are wide (such as humerus,radius, tibia, femur), they comprise adiaphysis (shaft) and epiphyses atthe distal and proximal ends, joiningat the metaphysis. In growing bone,this is the site where growth occursand is known as the epiphysealgrowth plate. Most long bones arelocated in the appendicular skeletonand function as levers to producemovementl Short bones – small and roughlycube-shaped, these contain mainlycancellous bone, with a thin outerlayer of cortical bone (such as thebones in the hands and tarsal bonesin the feet)l Flat bones – thin and usually slightlycurved, typically containing a thinlayer of cancellous bone surroundedby cortical bone (examples includethe skull, ribs and scapula). Most arelocated in the axial skeleton and offerprotection to underlying structuresl Irregular bones – bones that do notfit in other categories because theyhave a range of differentcharacteristics. They are formed ofcancellous bone, with an outer layerof cortical bone (for example, thevertebrae and the pelvis)l Sesamoid bones – round or ovalbones (such as the patella), whichdevelop in tendonsossification or endochondral ossification(replacing cartilage with bone).Bones are classified according to theirshape (Box 1). Flat bones develop frommembrane (membrane models) and sesamoid bones from tendon (tendon models)(Waugh and Grant, 2018). The term intramembranous ossification describes thedirect conversion of mesenchyme structures to bone, in which the fibrous tissuesbecome ossified as the mesenchymal stemcells differentiate into osteoblasts. Theosteoblasts then start to lay down bonematrix, which becomes ossified to formnew bone.Long, short and irregular bones developfrom an initial model of hyaline cartilage(cartilage models). Once the cartilagemodel has been formed, the osteoblastsgradually replace the cartilage with bonematrix through endochondral ossification(Robson and Syndercombe Court, 2018).Mineralisation starts at the centre of thewww.nursingtimes.net
Copyright EMAP Publishing 2020This article is not for distributionexcept for journal club useClinical PracticeSystems of lifeFig 3. Growth plate zonesGrowth plate zonesChanges inchondrocytesResting orquiescent zoneMatrix productionGrowth orproliferation zoneMitosisHypertrophic zoneMatrix calcificationgrowth stops (Ralston and McInnes, 2014).Males are on average taller than femalesbecause male puberty tends to occur later,so male bones have more time to grow(Waugh and Grant, 2018). Over-secretion ofhuman growth hormone during childhood can produce gigantism, whereby theperson is taller and heavier than usuallyexpected, while over-secretion in adultsresults in a condition called acromegaly.If there is a fracture in the epiphysealgrowth plate while bones are still growing,this can subsequently inhibit bone growth,resulting in reduced bone formation andthe bone being shorter. It may also causemisalignment of the joint surfaces andcause a predisposition to developing secondary arthritis later in life. A discrepancyin leg length can lead to pelvic obliquity,with subsequent scoliosis caused by tryingto compensate for the difference.RemodellingCell deathCalcification zonePrimaryspongiosaZone ofossificationFRANCESCA CORRASecondaryspongiosacartilage structure, which is known as theprimary ossification centre. Secondaryossification centres also form at the epiphyses (epiphyseal growth plates) (Danning, 2019). The epiphyseal growth plate iscomposed of hyaline cartilage and has fourregions (Fig 3):l R esting or quiescent zone – situatedclosest to the epiphysis, this iscomposed of small scatteredchondrocytes with a low proliferationrate and anchors the growth plate to theepiphysis;l G rowth or proliferation zone – thisarea has larger chondrocytes, arrangedlike stacks of coins, which divide andare responsible for the longitudinalgrowth of the bone;l H ypertrophic zone – this consists oflarge maturing chondrocytes, whichmigrate towards the metaphysis. Thereis no new growth at this layer;l Calcification zone – this final zone ofthe growth plate is only a few cellsthick. Through the process ofendochondral ossification, the cells inthis zone become ossified and formpart of the ‘new diaphysis’ (Tortora andDerrickson, 2009).Bones are not fully developed at birth,and continue to form until skeletal maturityis reached. By the end of adolescence around90% of adult bone is formed and skeletalmaturity occurs at around 20-25 years,although this can vary depending on geographical location and socio-economic conditions; for example, malnutrition maydelay bone maturity (Drake et al, 2019; Bartland Bartl, 2017). In rare cases, a genetic mutation can disrupt cartilage development, andtherefore the development of bone. This canresult in reduced growth and short statureand is known as achondroplasia.The human growth hormone (somatotropin) is the main stimulus for growth atthe epiphyseal growth plates. Duringpuberty, levels of sex hormones (oestrogenand testosterone) increase, which stopscell division within the growth plate. Asthe chondrocytes in the proliferation zonestop dividing, the growth plate thins andeventually calcifies, and longitudinal boneNursing Times [online] February 2020 / Vol 116 Issue 2 41Once bone has formed and matured, itundergoes constant remodelling by osteoclasts and osteoblasts, whereby old bonetissue is replaced by new bone tissue (Fig 4).Bone remodelling has several functions,including mobilisation of calcium and otherminerals from the skeletal tissue to maintain serum homoeostasis, replacing oldtissue and repairing damaged bone, as wellas helping the body adapt to different forces,loads and stress applied to the skeleton.Calcium plays a significant role in thebody and is required for muscle contraction, nerve conduction, cell division andblood coagulation. As only 1% of the body’scalcium is in the blood, the skeleton acts asstorage facility, releasing calcium inresponse to the body’s demands. Serumcalcium levels are tightly regulated by twohormones, which work antagonistically tomaintain homoeostasis. Calcitonin facilitates the deposition of calcium to bone,lowering the serum levels, whereas theparathyroid hormone stimulates therelease of calcium from bone, raising theserum calcium levels.Osteoclasts are large multinucleatedcells typically found at sites where there isactive bone growth, repair or remodelling,such as around the periosteum, within theendosteum and in the removal of callusesformed during fracture healing (Waughand Grant, 2018). The osteoclast cell membrane has numerous folds that face thesurface of the bone and osteoclasts breakdown bone tissue by secreting lysosomalenzymes and acids into the space betweenthe ruffled membrane (Robson and Syndercombe Court, 2018). These enzymeswww.nursingtimes.net
Copyright EMAP Publishing 2020This article is not for distributionexcept for journal club useClinical PracticeSystems of lifeFor more articles on themusculoskeletal system, go tonursingtimes.net/orthopaedicsFig 4. Bone remodelling processLining bone cellsResting stageBone formationBoneOsteoclastsOsteoclastrecruitmentand activationMatrixsynthesisOsteoblastrecruitmentand activationFRANCESCA CORRABone resorptionOsteoblastsOsteoclast removaldissolve the minerals and some of the bonematrix. The minerals are released from thebone matrix into the extracellular spaceand the rest of the matrix is phagocytosedand metabolised in the cytoplasm of theosteoclasts (Bartl and Bartl, 2017). Once thearea of bone has been resorbed, the osteoclasts move on, while the osteoblasts movein to rebuild the bone matrix.Osteoblasts synthesise collagen fibresand other organic components that makeup the bone matrix. They also secrete alkaline phosphatase, which initiates calcification through the deposit of calcium andother minerals around the matrix (Robsonand Syndercombe Court, 2018). As theosteoblasts deposit new bone tissuearound themselves, they become trappedin pockets of bone called lacunae. Oncethis happens, the cells differentiate intoosteocytes, which are mature bone cellsthat no longer secrete bone matrix.The remodelling process is achievedthrough the balanced activity of osteoclastsand osteoblasts. If bone is built without theappropriate balance of osteocytes, it resultsin abnormally thick bone or bony spurs.Conversely, too much tissue loss or calciumdepletion can lead to fragile bone that ismore susceptible to fracture. The larger surface area of cancellous bones is associatedwith a higher remodelling rate than corticalbone (Bartl and Bartl, 2017), which meansosteoporosis is more evident in bones with ahigh proportion of cancellous bone, such asthe head/neck of femur or vertebral bones(Robson and Syndercombe Court, 2018).Changes in the remodelling balance mayalso occur due to pathological conditions,such as Paget’s disease of bone, a conditioncharacterised by focal areas of increased andTransitiondisorganised bone remodelling affectingone or more bones. Typical features on X-rayinclude focal patches of lysis or sclerosis,cortical thickening, disorganised trabeculaeand trabecular thickening.As the body ages, bone may lose someof its strength and elasticity, making itmore susceptible to fracture. This is due tothe loss of mineral in the matrix and areduction in the flexibility of the collagen.Diet and lifestyle factorsAdequate intake of vitamins and mineralsis essential for optimum bone formationand ongoing bone health. Two of the mostimportant are calcium and vitamin D, butmany others are needed to keep bonesstrong and healthy (Box 2).Box 2. Vitamins and mineralsneeded for bone healthKey nutritional requirements for bonehealth include minerals such as calciumand phosphorus, as well as smallerqualities of fluoride, manganese, andiron (Robson and Syndercombe Court,2018). Calcium, phosphorus and vitaminD are essential for effective bonemineralisation. Vitamin D promotescalcium absorption in the intestines,and deficiency in calcium or vitamin Dcan predispose an individual toineffective mineralisation and increasedrisk of developing conditions such asosteoporosis and osteomalacia.Other key vitamins for healthy bonesinclude vitamin A for osteoblastfunction and vitamin C for collagensynthesis (Waugh and Grant, 2018).Nursing Times [online] February 2020 / Vol 116 Issue 2 42Physical exercise, in particular weightbearing exercise, is important in maintaining or increasing bone mineral densityand the overall quality and strength of thebone. This is because osteoblasts are stimulated by load-bearing exercise and sobones subjected to mechanical stressesundergo a higher rate of bone remodelling. Reduced skeletal loading is associated with an increased risk of developingosteoporosis (Robson and SyndercombeCourt, 2018).ConclusionBones are an important part of the musculoskeletal system and serve many corefunctions, as well as supporting the body’sstructure and facilitating movement. Boneis a dynamic structure, which is continually remodelled in response to stressesplaced on the body. Changes to this remodelling process, or inadequate intake ofnutrients, can result in changes to bonestructure that may predispose the body toincreased risk of fracture. Part 2 of thisseries will review the structure and function of the skeletal system. NTReferencesBartl R, Bartl C (2017) Structure and architectureof bone. In: Bone Disorder: Biology, Diagnosis,Prevention, Therapy. Bit.ly/SpringerBoneDisorderDanning CL (2019) Structure and function of themusculoskeletal system. In: Banasik JL, CopsteadL-EC (eds) Pathophysiology. St Louis, MO: Elsevier.Drake RL et al (eds) (2019) Gray’s Anatomy forStudents. London: Elsevier.Iyer KM (2019) Anatomy of bone, fracture, andfracture healing. In: Iyer KM, Khan WS (eds)General Principles of Orthopedics and Trauma.London: Springer.Moini J (2019) Bone tissues and the skeletalsystem. In: Anatomy and Physiology for HealthProfessionals. Burlington, MA: Jones and Bartlett.Ralston SH, McInnes IB (2014) Rheumatology andbone disease. In: Walker BR et al (eds) Davidson’sPrinciples and Practice of Medicine. Edinburgh:Churchill Livingstone.Robson L, Syndercombe Court D (2018) Bone,muscle, skin and connective tissue. In: Naish J,Syndercombe Court D (eds) Medical Sciences.London: ElsevierTomlinson RE, Silva MJ (2013) Skeletal blood flowin bone repair and maintenance. Bone Research;1: 4, 311-322.Tortora GJ, Derrickson B (2009) The skeletalsystem: bone tissue. In: Principles of Anatomy andPhysiology. Chichester: John Wiley & Sons.Waugh A, Grant A (2018) The musculoskeletalsystem. In: Ross & Wilson Anatomy and Physiologyin Health and Illness. London: Elsevier.CLINICALSERIESSkeletal systemPart 1: Anatomy and physiologyof bonesPart 2: Structure and function ofthe skeletal systemFebMarwww.nursingtimes.net
reviews the anatomy and physiology of bone. Understanding the structure and purpose of the bone allows nurses to understand common pathophysiology and consider the most-appropriate steps to improve musculoskeletal health. Citation Walker J (2020) Skeletal system 1: the anatomy and physiology of bones. Nursing Times [online]; 116: 2, 38-42.