Transcription
Physiology and Pathophysiology of LiverProf. Anil Dhawan MD FRCPCHDirector , King’s Cell Therapy UnitDirector Paediatric Liver GI and NutritionCentreKing’s College HospitalLondon
Remit of the talk Applied anatomySynthetic functionsDetoxification functionsCommon pathophysiology states in liver disease–––––Hepatorenal syndromeHepatopulmonary syndromeAscitesEncephalopathyPortal hypertension
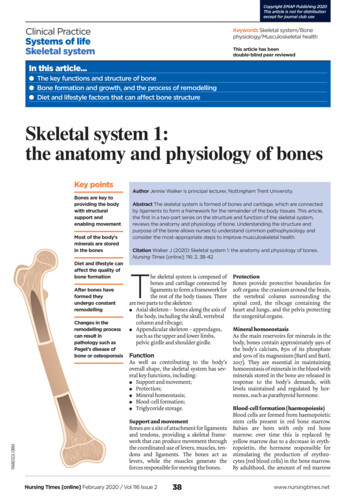
Hepatic Blood FlowDual blood supplyHepatic Artery (40%)Portal vein (60%)OutflowThree Hepatic Veins
Formation of bileCentral function of liver
Focal biliary teOSTα/βCl-MRPsMRP2CholangiocyteBA
triglyceridesproteinglycogengalactosefree fatty acidsG6Pglucosepyruvatelactateamino acidsfatty acyl-CoAacylcarnitinesPDHorganic acidsNH4 ß-oxidationUrea cycleketonesTCA cyclereducing equivalentsrespiratory chainATPUrea
aminoacidopathiesproteinamino acidsorganic acids organic acidemiaNH4 Urea cycle urea cycle disordersUrea
pathway: branched chain amino thylacrylyl-CoA2-oxo-isocaproateMSUDisovaleric acidaemia3-methylcrotonylCoA carbox yl-CoAHMG CoA lyase def2-methylacetoacetyl-CoAb- ketothiolase nyl semialdehydeacetacetic acidacetyl-CoApropionyl-CoApropionic acidaemiamethylmalonyl-CoAmethylmalonic acidaemiasuccinyl-CoA
Detoxification Functions of Liver
1. Initial Event2. Toxin-concentrationHydrophobic substances Infection (bact./viral) Hydrophobic bile acids Bleeding Bilirubin Intoxication Toxin Hypothesis of Liver failure: plasmatic NO Ischemia ProstacyclineVicious cycle of autointoxication other Indol/Phenol-3. SecondaryOrgandysfunctions Brain (HE, Edema) Kidneys (HRS) Cardiovascular system(SVRI , MAP , CI ) Bone marrow (Depression) Immune system (Activation/Paralysis) Liver (Inflammation, Necrosis, Apoptosis)Metabolits Toxic fatty acids Thiols Digoxin/Diazepamlike subst.Hydrophilic substances Ammonia Lactate AAA
NAFLD In Children
Pathogenesis of NAFLD
Fatty sis ofFatty acids
AdipocytesInsulinXIncreased uptakeof fatty acidsFatty acidsMitochondrialß-oxidation overloadIncrease in cytochrome P-450 4AIncrease in cytochrome P-450 2E1TNF- RadPC-1LeptinFatty acidsXHEPATOCYTETNF- RadPC-1LeptinFatty acidsInsulinLipid peroxidationAccumulationof fatty acidsIncrease in glycoloysisDecrease inapolipoproteinB-100XVLDLSynthesis of fatty acidsAccumulation of triglyceridesHyperinsulinemia
InsulinAdipocytesIncrease inlipolysisIncreased uptakeof fatty acidsTNF- RadPC-1LeptinFatty acidsXInsulinXTNF- RadPC-1LeptinFatty acidsFatty acidsAcyl-coenzyme dacyl-coenzyme AAcyl-coenzyme AH2O2Peroxisomalß-oxidationMicrosomal -oxidationPPAR- H2O2Expression ofuncoupling protein-2Diacarboxylicfatty acidHEPATOCYTE
Pathogenesis of NAFLD
Pathogenesis of NAFLDROS to Steatohepatitis
Vascular Pathologies Portal inflow– EHPVO– Portal Vein Sclerosis Hepatic artery pathologies– Rare , hepatic artery problems more seen after LTx Hepatic venous outflow– Budd Chiari Syndrome– Sinusoidal obstruction syndrome
Medussa Head venous pattern
Spider Naevi
Renal Involvement In Liver Disease
Pathogenesis of Acute Kidney InjuryArterial vasodilatation (‘’VASOPLEGIA’’)Decreased SVRHigh Cardiac OutputRenal Auto-regulation becomes PressureDependent - Intra-renal Vasoconstriction42
Aetiology of renal involvement in LD Multifactorial Hypovolaemia induced pre-renal AKI Acute tubular necrosis due to profoundhypovolemia and hypotension. Direct drug nephrotoxicity (paracetamol,NSAIDs) OR Drugs affecting both liver/kidney Hepatorenal syndrome Intra-abdominal hypertension (IAH) anddevelopment of ICS44
HEPATO-RENAL SYNDROME
HRS - Diagnosis of exclusion Hepatorenal syndrome (HRS) is defined as theoccurrence of renal failure in a patient withadvanced liver disease in the absence of anidentifiable cause of renal failure The diagnosis of HRS is one of exclusion,so investigations should be performed torule out other common causes of AKI.47
Characteristics of Type 1 and Type 2 Hepatorenal SyndromeCoursePrecipitatingEventHistory ofDiureticResistantAscitesPrognosisType -1 HRSPrecipitousPresent in doubling of50% of casesserum creatinine in 2 weeksMay or maynot bepresentWithout therapy90-daysurvival of 10%Type -2 HRSGraduallyprogressiveAlwaysPresentMedian survival6 monthsAbsent
Ascites
404030302020Compliance IAPIntra-abdominal pressureSugrue et al Arch Surg 1999 134:1082Malbrain CCM 2005;33:315263 patients 40.7% increased IAPRenal dysfunction:32% with IAP elevated14% with normal IAP32% IAP 1240% IAP 20IAP10IAPCVPPcwP100000IVCPSVCP1010202030304040
HEPATOPULMONARY SYNDROME
HPS and clubbing in CLD
Definition – HEPATOPULMONARYSYNDROMEArterial Oxygenation Defect induced by intrapulmonary vasculardilatation(IPVD) associated with hepatic diseasePage 53
Hepatopulmonary syndrome (HPS)Liver diseaseShunting &Arterial hypoxemiaIntrapulmonaryVascular dilatationIn absence of intrinsic cardiopulmonary disease
Pathogenesis Enhanced pulmonary production of nitric oxide Exhaled nitric oxide increased in HPS , normalise aftertransplant Nitric oxide synthesized by nitric oxide synthase – eNOand iNO eNO – pulmonary endothelial cells iNO – alveolar macrophages Endothelin 1 acts through ET-A (vascular smoothmuscle)or ET-B receptors (pulmonary endothelium) ET-A causes vasoconstriction, ET-B causes vasodilatationPage 55
Mechanism of hypoxaemia in HPSPage 56
Clinical Features of HPS Non-specific Dyspnoea at rest/exertion Platypnoea/orthodeoxea – Arterial PaO2 decreases by5% or more when the patient moves from a supine to anupright position -further ventilation-perfusion mismatch Spider nevi, digital clubbing, cyanosis Differential Diagnosis : Several pulmonary complications or pleuralcomplications Porto-pulmonary hypertension (PPHTN)Page 57
CARDIOVASCULAR INVOLVEMENT IN ALF
Cardiovascular changes in ALF Pathogenesis Multi-factorialLesser intake, ongoing losses - hypovolaemiaSevere SIRS and sepsis play a paramount role.Vasodilatation - due to loss of vascular toneleads to systemic hypotension, low effectivearterial blood volume and high cardiac output Cytokine release from the failing liver appears tobe partly responsible for the observedhaemodynamic disturbances Subclinical myocardial injury59
ImplicationThe associated cardiovascular collapse andorgan hypo-perfusion may be central to theprogression of multiple organ failure60
Strategy Target hypovolaemia - fluids Target SIRS, infection - antibiotics Target vasodilatation – vasopressorsnoradrenaline , vasopressin If myocardial depression - Inotropes Target Adrenal insufficiency Optimise oxygen delivery61
Neurological Involvement In Liver Disease
Neurologic Support; Brain SwellingAcute Hepatic DysfunctionNeurotoxins; AmmoniaAstrocytic metabolismto glutamineIncreased intra-cellularosmotic loadMitochondrial toxicityFailure ofenergy metabolismNeurotransmitteralterationsSystemic InflammatoryResponseVascular functionVasomotor dysfunctionEndothelial dysfunctionAlterations in BBB ?Water/neurotoxinpermeabilityMitochondrial toxicityFailure ofenergy metabolism
Neurological involvement in ALF Highly contentious in ALFConcept of Hyperaemia vs IschaemiaRisk factors for ICP ?Neuro-critical care monitoring –To Bolt or Notto bolt ? Role of non/minimally invasive monitoring ? Management uncertainties ?
Who is at risk of raised ICP? 25-75% of ALF with Grade iii/ivencephalopathy Rapid onset High ammonia Younger age Inotropic support RRT
Neurologic Support; Arterial Ammonia andRisk of Cerebral OedemaALF Cases, n 165BERNAL W, ET AL. HEPATOLOGY 2007; 46:1844-52
Why does raised ICP matter Compromises CPPTranstentorial herniation2nd commonest cause of death in ALFDoes measuring it help?
Summary
ConclusionsUnderstanding of applied anatomy andphysiology is essential to understand thecomplications and natural history of liver disease
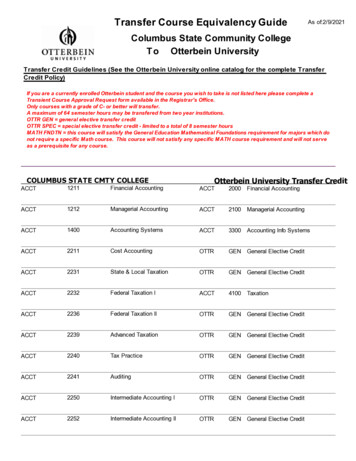
Common pathophysiology states in liver disease -Hepatorenal syndrome -Hepatopulmonary syndrome -Ascites -Encephalopathy -Portal hypertension. Hepatic Blood Flow Dual blood supply Hepatic Artery (40%) Portal vein (60%) Outflow Three Hepatic Veins . Formation of bile Central function of liver . PC OCT NTCP OATP OC BA OA MDR3 OA MRP2