Transcription
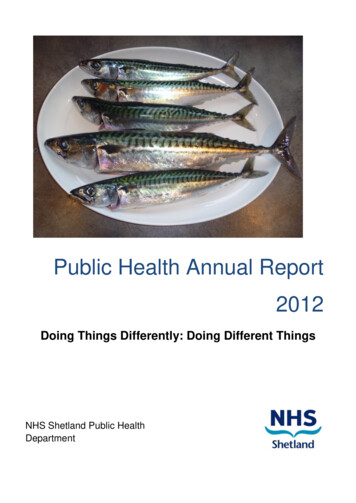
Public Health Annual Report2012Doing Things Differently: Doing Different ThingsNHS Shetland Public HealthDepartment
A recipe for mackerelCatching your own fish isn‟t essential to this recipe; it just adds to the fun. The key tosuccess is sharing fresh, tasty food with friends and family; all pitching in and havinga good time.You will need:A bunch of friends, family, neighbours (preferably of different generations)A boat, fishing lines and some bait (alternatively you can use shop bought fish– but it isn‟t quite the same)To accompany the fish: fresh veg a little wine laughter – to tasteStep 1: Catch your mackerel.Choose a fine day, take your friends and family off on the boat and catch your fish.Relax, enjoy yourselves, have fun. Let the older generation teach the youngergeneration how to fish.Step 2: CookPrepare your fish in whatever way you want: add some seasoning, some spice orleave it as it is. Barbeque on the beach, stick under the grill, fry in the pan - it‟s up toyou. All join in and help cook the food.Step 3: ServeAdd some fresh veg, some tatties or brown bread. Serve with a small glass of wine ifyou like, iced water for the bairns.Step 4: EatAs step 1: relax, enjoy yourselves, have fun2
Table of ContentsIntroduction . 4Public Health Ten Year Plan: Changing the World(Executive Summary) . 4Improving Health – how far have we come? . 7Asset-based approaches – not the „nanny state‟ . 27The Big 3.and the even Bigger Questions. 38Smoking .39Alcohol .47Obesity .56Poverty & Inequalities . 66A personal perspective . 79Now it‟s over to you. . 82AcknowledgmentAs usual, I am indebted to the contributions and help given by colleagues both withinthe Department of Public Health, across NHS Shetland, and in partner organisationsincluding Shetland Islands Council, other Community Planning Board partners andother organisations working for the improvement of health in Shetland. In particularmy thanks go to: Kathleen Anderson, Kim Govier, Wendy Hatrick, Andy Hayes, DavidKerr, Dr Susan Laidlaw, Elizabeth Robinson, members of the Health ImprovementTeam, and colleagues and clients from Community Alcohol and Drug Service Shetlandfor the Recovery quotes.Dr Sarah TaylorDirector of Public Health3
During 2011/12 the Public Health Department decided that the time had come for a change.We could carry on doing the things we have traditionally done, making slow but steadyprogress, or we could be more ambitious, set our sights higher, do things differently. We setdown these thoughts in our Ten Year Plan: Changing the World. The executive summarybelow describes our reasons for change and a radical vision for action. The rest of ourAnnual Report gives more insight into how we might achieve this.Public Health Ten Year Plan: Changing the World(Executive Summary)This strategy was written to answer the questions we posed in the 2011 Public HealthAnnual Report: what can we achieve to improve health in Shetland? How much should weinvest? Where should we focus our effort? Are there different approaches that we shouldtake?It attempts to set out a bold and radical vision for the future of Shetland in which people livelonger, in good health, and where everyone contributes to the communities that they live in.Our strategy looks longer term, is more ambitious, thinks more holistically about health. Weneed to make better use of the resources we have, so we need to do things better – bemore efficient, build our knowledge and experience of what works, and have a biggerimpact in what we do. We want to move beyond just focusing on specific „unhealthy‟behaviours, to take a more positive approach to improving our health both personally andas a community.The strategy summarises the case for investing in health improvement, with evidence forsavings to be made on health (and other) services through the prevention of ill-health. Itsets out the current context of non-sustainable public sector services, and reducingbudgets. It develops the theme of 'doing things differently' through early intervention, assetbased approaches, developing resilience at personal and community levels, with anemphasis on tackling inequalities - not widening the gap.4
The strategy then sets out the longer term outcomes we are working towards, and how wecan achieve them, using familiar themes that illustrate different public health approaches:Smoking: Early intervention that means people don't start to smoke in the first place or helpsthem quit before it becomes an ingrained habit or addiction. Using incentives to help people stop smoking, which might be about motivation inpregnancy or around children, or personal goals and rewards. Community action - developing and supporting a non-smoking culture.Obesity: Tackling the stigma and prejudice around being underweight and overweight Tackling the factors which cause and contribute to being an unhealthy weight. Taking direct action to help people to be more active and to eat more healthily; bothindividually and at policy and community levels. Early intervention with families and through nurseries and schools to preventchildhood obesity, which includes working with pregnant women, promoting breastfeeding, and working directly with children and families to tackle weight issuessuccessfully.Alcohol: Changing the culture on drinking to tackle harmful drinking and make it easier forpeople with a problem to come forward and ask for help. Working in partnership with the Licensed Trade, police, environmental health topromote sensible drinking. Early intervention through programmes such as Alcohol Brief Interventions to flagrisky drinking at an early stage and offer appropriate help and support for people tochange their habits.Poverty & Inequalities:Although Shetland is a relatively prosperous community, and we have, for the most part, agood quality of life, there are still people living in Shetland in poverty, families who are notable to access services, or get the help and support they need, and people who suffer fromdiscrimination and exclusion. Recent research by young people (“Poverty is bad: let‟s fix it!”)has identified local issues and action to take: around lack of available/affordable transport,5
isolation, mental health and substance misuse problems, and stigma. The Fairer Shetlandprogramme is coordinating local work to tackle poverty and deprivation with priorities on fueland transport poverty, and dealing with the consequences of the current UK WelfareReforms. We need to tackle health inequalities alongside economic and social inequalities,and our priorities on this are:The Keep Well programme – focusing on our most deprived communities and households,and delivering health checks and preventative services to people who are „hardest to reach‟or who do not normally access primary care services.Early Years – preventing problems in children and families before they become entrenched,and building the capacity of families to give children the best chances in life.Specific work on supporting parenting: Improving children and parents‟ emotional resilience and mental wellbeing. Intervening in domestic abuse in families with children to break the cycle of violence. Long term conditions and chronic disease management:o Recognizing that people who live with chronic disease are often the expertson their diseases.o Supporting them to manage their condition with appropriate advice and help.o Promoting early intervention to prevent complications, and helping people tobe as independent as possible and reach their full potential, with whatevercondition or disability they have.Other themes will develop as we do more work and these include: mental health andwellbeing; developing resilience and the capacity of communities to help themselves; healthpromoting health services.This strategy won‟t have it all right, and it certainly doesn‟t yet have all the detail it needs.But the evidence is that we could make a significant difference to the health of people inShetland over the next 10 years, with the right focus and effort. The challenge is to makethat happen.6
Improving Health – how far have we come?How do we improve health? To answer in simple terms, we have to increase the things thathave a positive impact on health, and reduce the things that make health worse. Howeverthe things that influence health are complex, and may be the result of a number of factorsincluding personal biology and genetics; environment; culture; socio-economiccircumstances; personal beliefs and attitude; and behaviour. To complicate things further,what we mean by „health‟ and good health or poor health differs between individuals andbetween different populations.And, what we know about attitudes towards health andinfluences on health has changed over the years, withadvances in science and changes in culture: it is hardto believe that cigarette advertising used to useendorsements by doctors about the pleasure ofsmoking.So, if the factors that affect health are complex, howwe influence these factors is also complex. Somethings can‟t be changed: such as family history andgenetic make upa and the fact that we all get older.However, we can change attitudes and behaviour,both at an individual level and population level – it maytake a long time and may not be easy, but can be done.But just having the scientific knowledge and evidence which has the potential to changeattitudes and behaviour will not necessarily mean that things will change. As well asacceptance by the population, there needs to be political will and often (but not always)significant investment. However, as we discussed in last year‟s Public Health AnnualReport, there is a strong business case for health improvement as investing in improvinghealth which then prevents illness will save money in the long term.1 How GovernmentaAlthough scientific advances in gene technology may make this possible in the future: but thisdoes bring with it ethical dilemmas.7
policy is influenced is very complex, with „health‟ being one factor to take into accountalongside economics, international relations and industry concerns. Consider, for example,how valuable the alcohol industry is to both the treasury (through taxation) and localeconomies, through employment.In this chapter, we will look at some of the most important health issues, past and present,and how successful, or otherwise, we have been in tackling them through traditional healthimprovement approaches.Clean water and vaccinesAccording to the World Health Organisation, the two public health interventions with thegreatest impact are clean water and vaccination.2 Implementing these lifesavinginterventions required scientific advances; investment of resources; legislation and changesin people‟s beliefs and thinking. And, although we take these for granted now in oursociety, there are still huge parts of the world where people do not have clean water, anddo not have access to vaccination. Even where high quality, safe and free vaccinationprogrammes are in place (as in the UK) people do not always access them, often becauseof personal beliefs and attitudes.We now do not think twice about the importance of clean water, and we are well aware that„dirty‟ water may carry bugs that cause dangerous infectious diseases. Centuries ago, wheninfectious diseases were very common, people believed that they became ill due tochanges in the air around the diseased tissue of people who already had the illness. Thiswas developed into the „Miasma‟ theory of disease which proposed that a vapour in the aircaused diseases. However, in 1854, a cholera outbreak in London led to a new theory: thatcholera was spread from person to person, by something from thegut of an infected person being ingested by a healthy person. JohnSnow, a doctor, investigated the outbreak by plotting thegeographical location of all the people with cholera and then linkingthem with a particular water supply (from the „Broad Street Pump‟).Further investigation involving London water supplies demonstratedthat cholera was associated with drinking water contaminated bysewage. With the invention of the microscope in the 1670s, it waspossible to see micro-organisms in substances such as blood and8
water. But no association was made between these and illness in man until the late 1800swhen the Germ theory of disease was developed. 3Once people knew that germs in the water caused disease, they could then take action toeither prevent people drinking the contaminated water (John Snow got the Broad StreetPump handle removed); or clear the germs out of the water (the water treatment processesthat we use nowadays); or prevent the germs getting into the water in the first place(sanitation - which is the provision of facilities and services for the safe disposal of humansewage).It is a similar story with vaccines. As long ago as 429 BC, the Greek historian Thucydidesnoticed that those who survived a smallpox plague did not become re-infected with thedisease.4 In 900 AD, the Chinese started to use a simple form of vaccination calledvariolation. The aim was to prevent smallpox by exposing healthy people to smallpox scabs,by either putting some of the scab tissue under the skin or up the nose. Variolation startedto be used in England in the early 18th century; it caused mild illness, and sometimes deathbut there was less smallpox in the populations that used it. This was at a time whensmallpox was the most infectious disease in Europe and killed 20% of the people infected. 5Then in 1796, Dr Edward Jenner discovered vaccination as we know it now. Initially he wasridiculed, but eventually the scientific community, and the wider population, was convincedthat it worked and vaccination grew in popularity throughout Europe and then in America.However in the late 1800s people started to oppose vaccination – not believing that it couldreally work and that it took away people's civil liberties.6 These viewpoints still exist today,despite all the evidence about the effectiveness of vaccines:The eradication of smallpox has been a global immunisation success: now the onlysmallpox virus left in the world is in a small number of secure laboratories.Following the introduction of a vaccine against meningitis C in 1999, the number ofcases in Scotland has dropped by 90%.In the UK, many diseases that were previously very common are now rare, such asdiptheria.Even though safe and effective vaccinations are available, we have not yet been able tocontrol certain diseases such as measles. Although considerable progress has been madeglobally, there are still some challenges. In developing countries, or those affected by war9
and civil unrest, the funding to pay for vaccinations and the health infrastructure required todeliver a programme may not be available. Even in countries such as the UK where there isa well resourced childhood vaccination programme, not all children are able to benefit. Avery small number are unable to have vaccinations because of particular medicalconditions. A far greater number of children are not immunised because their parents donot take up the vaccinations offered.For most vaccine preventable disease, the number of children who are unvaccinated issmall enough to allow herd immunity. This means that the unvaccinated children areprotected because enough other children have been vaccinated to prevent the infectioncirculating through the community. However, in the case of the MMR vaccine in the UK, theuptake is low enough in some places, including Shetland, to allow measles to circulate,potentially causing outbreaks of illness.One of the reasons why parents do not vaccinate their children is because they are notconvinced by the evidence given by healthcare professionals and scientists for the need forvaccination. Of course people have a choice: but the scientific and health communitieshave a responsibility to ensure that the information we give out to people is accessible,consistent and understandable so that people can make an informed choice regardingvaccinations, as with other health protection and health improvement interventions.A Model of Health ImprovementIn thinking about health improvementactions and programmes, it is helpfulto have a structure in place to planactivity. There are a number ofmodels of health improvement: theone on the left was developed by A.Beattie in 1991.7This model shows that healthimprovement actions can be at anindividual level, or population level, orsomewhere in between. They can10
also be authoritative (telling people what to do) or negotiated (enabling people orpopulations to change), or again somewhere in between.Different health improvement activities can be plotted somewhere on this grid: so legislationsuch as the ban on smoking in public places, seatbelt laws, age restrictions on thepurchase of alcohol and tobacco is at a population level and is authoritative. Smokingcessation and weight management services are generally at an individual, or small group,level and tend to be negotiated.Midwife advising apregnant womanto stop smokingAlcohol andtobacco salesBan on smoking inpublic placesHealth promotionin schoolsFacilitated weightmanagementprogrammeSupport group forhelp people withalcohol problemsArticle in localpress about fluvaccinationCommunity groupidentifying ahealth needdeveloping ownsolutionsMost health improvement programmes need a range of activities spread across the grid tobe effective. So if we have public information campaigns to tell people to stop smoking, wealso need to put in place smoking cessation services to help them.The range of interventions that we employ for particular health issues will vary. In generalthe provision of information and education, at individual (e.g. advice from the GP), smallgroup (e.g. school) and population (e.g. national campaigns) levels is the basis of manyprogrammes. If we are looking at individual behaviours such as smoking, drinking andphysical activity then individual „negotiated‟ activities will be useful as long as people takethem up. If we are looking at protecting individuals or groups, then legislation is useful;legislation can happen when we have an agreement in society to oblige people to comply11
and to police that compliance, which is as much an individual as a group responsibility.Legislation is often about protecting children (e.g. minimum age laws) or other members ofthe population whose health could be affected (ban on smoking in public places; drinkdriving laws).It is important to recognise that just telling people to do something or not do somethingdoes not necessarily change an individual‟s behaviour. Wearing seatbelts is an example.Whilst legislating for passengers (especially children) can be seen as protecting the peoplewho are not in control of the car, it could be argued that the driver should be able to maketheir own choice, given balanced information. But before legislation, compliance withpublic information and advice was poor. In the UK a law was introduced in 1983 requiringdrivers to wear seatbelts. This must have been seen by the population as something sonecessary, that people should not have a choice, although it took more than ten years toget it through Parliament. By this stage, the population was generally accepting of therationale for the law, and as people are generally law abiding, and action was taken againstthose who did not comply, then they did change behaviour. 8 Now in 2012, seatbeltwearing is taken for granted by nearly all the population: though we still see public safetyadvertisements reminding people.12
We do also use the evidence that says that a GP, or other doctor, spending a few minutesdiscussing smoking with a patient or asking them about drinking, can be the catalyst thatsomeone needs to make them change behaviour. It does not seem to happen frequently,but it is such a relatively low cost action that only a few people have to change behaviour tomake it cost effective.9 And although that particular conversation may not be the one thatpersuades someone to change behaviour, it may help them start to think about it andeventually they will decide themselves to make the change; especially if they are hearingthe same message in other settings. When smoking cessation services were first brought inacross the UK in the late 1990s, this „brief intervention‟ was the first element of a tieredapproach to supporting people to quit. More recently in Scotland we have introduced theAlcohol Brief Intervention (ABI) which is a similar idea, that by asking a patient aboutdrinking and giving some brief advice, a proportion of people who have harmful drinkingpatterns will modify their drinking without any further help.10But what we often find is that some groups of people find it much easier to changebehaviour than others. The people who can find it most difficult are those who are moredisadvantaged, vulnerable, socially excluded, or have multiple health issues for example.And there is a problem in that when health improvement interventions are implemented ona population wide basis, they are most effective in changing behaviour in the groups thatfind it easiest to change and less effective in the more vulnerable groups, which means thatwe effectively leave behind people who are more disadvantaged and the inequalities gapincreases. This is discussed further in the chapter on Poverty & Inequalities. Theselimitations with traditional programmes have led to a more targeted approach in many areasof health improvement, such as using social marketing techniques for campaigns.13
Social marketing is a method of applying the science of marketing to social policy andbehaviour change in the context of health improvement. In a book on social marketing,subtitled „Why should the devil have all the best tunes?‟, Gerard Hastings argues that thetechniques used by big companies to get us to eat big brand beef burgers and smokeparticular types of cigarettes can also be used to encourage people to eat healthily,preserve their lungs and walk to work.11 But to do this we need to be cleverer aboutunderstanding our target audiences. Social marketing uses techniques such as brandingand „segmentation‟, therefore understanding the very different reasons that people have for(e.g.) drinking alcohol, and the very different ways that different groups of people usealcohol will help us to design interventions which are far more likely to have an impact onthem, because they are far more likely to be relevant.Shetland Public Health Annual Report 201012There is also the balance between targeting interventions and yet not stigmatising people.So for example, in Shetland we have a sexual health clinic that is open to anyone, and ispromoted as such. The advertising for the clinic has to be targeted to ensure that all thepotentially more vulnerable groups see the clinic as being for them (for example youngpeople and older people, people who are lesbian, gay, bisexual and transgendered).Furthermore, where people find it more difficult to make behaviour change to improvehealth, then health improvement interventions have to make it easier for people to make thechanges.14
What influences behaviour?In previous Public Health Annual Reports we have looked at what motivates people tochange behaviour. In 2010, we wrote about risk taking, and how people decide what actionto take based on their perception of risk:Threats that are unfamiliar, exotic, involuntary and „man made‟ are often seen as more of ahealth risk than those that are familiar, domestic, voluntary and „natural‟. So people oftenworry less about the potential health effect of, for example, smoking and excess alcohol(familiar, domestic and a voluntary element) than the potential health effects of terrorism ornuclear accident (unfamiliar, involuntary and man made) or bird flu (unfamiliar, exotic andinvoluntary).13In last year‟s Annual Report we looked at different approaches to influencing behaviourincluding the „nudge‟ approach as favoured by the UK Government:The government cannot force people to live healthy lives. People can be helped andencouraged to make healthier choices. Local communities working together, and with agood understanding of human behaviour, will achieve more than extra laws and lecturesfrom the government.14In 2011, the House of Lords Science and Technology Committee published a report onbehaviour change.15 This describes how some choices are consciously planned ordeliberative, and some are unconscious or non-deliberative. The report uses the analogy ofbuying and driving a car: buying a new car will usually be made only after much consciousdeliberation (along with unconscious motivations), but when a car is being driven down avery familiar route the driver will be acting automatically, ie not really having to think aboutwhere they are going. The report states:Both deliberative and non-deliberative choices and actions can be affected by social factors(such as personal interaction and interaction within, and between, groups) and the largescale social context (such as state of the economy). Behaviour is also influenced by thephysical environment in which it takes place. The ready availability of cheap and unhealthyfood, for example, makes it more likely that people will consume it. Similarly, if there arevery busy roads and no cycling lanes, people are less likely to travel by bike.So, for example, the smoking ban has made it easier for people who want to stop smokingto avoid cigarettes when they are on a night out; creating safe footpaths and green spacesmakes it easier for people to walk and exercise outside; reducing the price of fruit andvegetables would make it easier for people to choose these over other foods. Whilst this15
has been done using legislation in many cases, there is still a long way to go in changingenvironments to make the healthier choice the easier choice.The House of Lords report went on to discuss what are the gaps in our knowledge aboutbehaviour change:.lack of understanding about aspects of the automatic system, particularly in relation tohow emotional processes regulate everyday behaviour; a lack of comparative research intothe limits to the transferability of behaviour change interventions across cultural differences;uncertainty about how genes interact with environmental and social factors to causebehaviour; and, a lack of understanding about the effect of social dynamics on behaviour.So there is clearly more that we need to understand about what motivates and supportspeople to change behaviour; and especially which of these factors we can influence, andhow. However, there is a lot that we do already know, and the following sections look athow far we have come in changing behaviour and improving health across our three priorityareas: smoking; alcohol and obesity.Smoking in public places: legislation and changing attitudesThe history of smoking, and tobacco control, can be used as an example of how there hadto be changes to a number of different factors in order to improve health (in this case byreducing smoking behaviour). Firstly there had to be an acknowledgement that smokinghad an adverse effect on health. This was suggested as far back as 1604, but the largescale studies that showed a clear link between smoking and ill health were conducted in the1950s. Up until that point smoking was seen as the „norm‟ with two thirds of men andincreasing numbers of women smoking tobacco. Smoking was promoted in the armedforces during the two world wars; cigarettes were included in soldiers‟ rations and millions offree cigarettes distributed by tobacco companies. In America,tobacco was designated as a protected crop and certain brandsused the fact that doctors smoked them as an endorsement forthat brand. Even when the scientific evidence was available, ittook years for Governments to take action which could affect theirrevenue from tobacco taxation, and which put them up against thepowerful tobacco industry.In 1999, David Pollock published a book called Denial & Delay,subtitled The Political History of Smoking and Health, 1951-1964:Scientists, Government and Industry as seen in the papers at the Public Records Office.1616
This book described the earliest steps in trying to convince government and society thattobacco was damaging to health. Pollock describes how, year after year, expert statementsfrom advisory groups and the Medical Research Council were watered down and ignored.Anecdotally, Iain Macleod, the Chief Medical Officer at the time, chain-smoked while hemade the first Ministry of Health announcement on the subject!The annual reports of the Medical Officer for Health for Shetland in the 1950s illustrate quiteclearly the uphill battle he had with trying to persuade the population, and the localauthority, that smoking should not be allowed in public places.1956: “Efforts to persuade the young to remain non-smokers are unlikely to besuccessful unless we are prepared to show moderation in our own smoking habits.Could not a start be made locally by the public agreeing to give up smoking in buses,cinemas, restaurants and food shops? “1957 “In time the public will object to seeing a layer of smoke exhaled from the lungsof others settling over the table in a restaurant or over the food in a Baker‟s shop.”1958 “The climate of opinion at present is such that I think we must wait and hopethat in a few years time the public will start listening to the small voices of the few whoare trying to call attentio
Prepare your fish in whatever way you want: add some seasoning, some spice or leave it as it is. Barbeque on the beach, stick under the grill, fry in the pan - it‟s up to you. All join in and help cook the food. Step 3: Serve Add some fresh veg, some tatties or brown bread. Serve with a small glass of wine if you like, iced water for the bairns.